Scroll down to listen to this article.
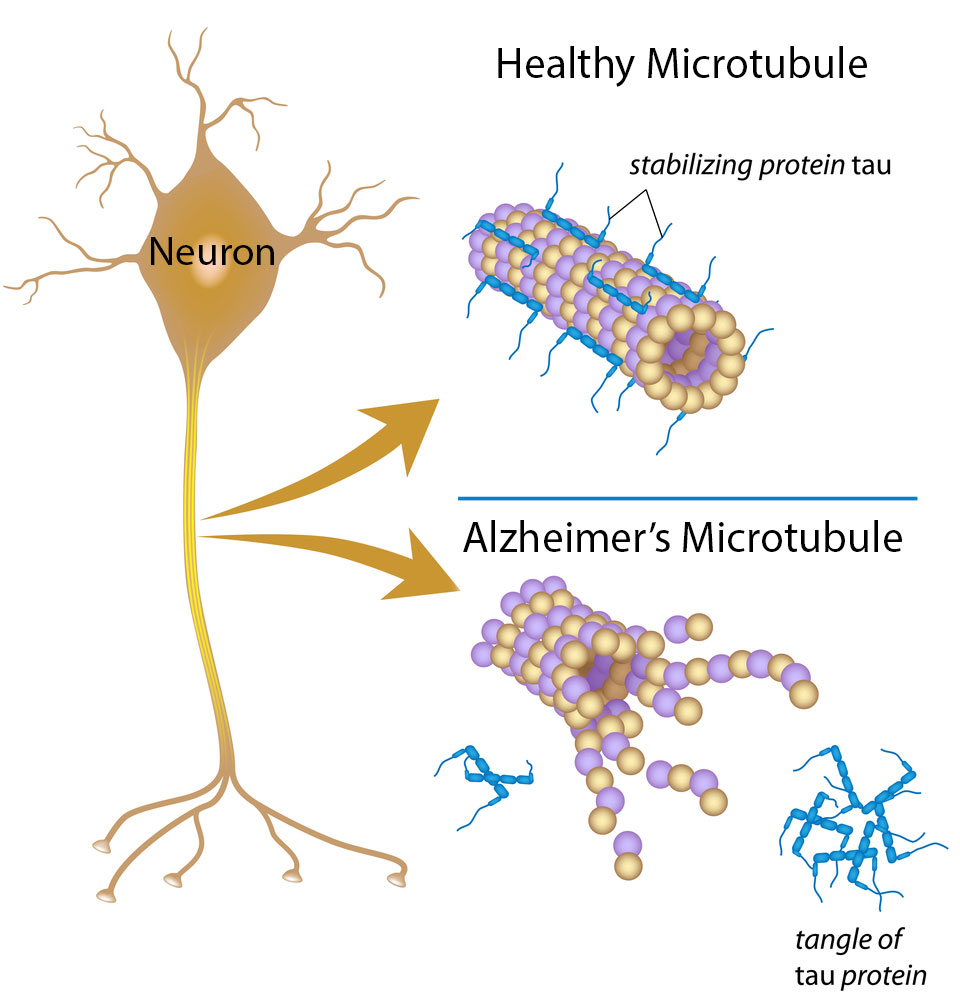
Alzheimer’s Dementia, often shortened to AD, is abjectly terrible. People with the disease lose memories, language, and the ability to function by themselves. It was first described over a hundred years ago by Dr. Alzheimer, and there has been startlingly little progress in treating the disease since. Alzheimer’s disease is a dementia characterized by two kinds of brain deposits: amyloid plaques and tau tangles. It’s the most common type of dementia. Dr. Alzheimer also noticed the distinct presence of extra cholesterol in the brain, which we will return to.
We have few medications that are approved to help with Alzheimer’s. Even these don’t cure the disease but instead slow its progress. This indicates a fundamental lack of a good model for how the disease starts or progresses. The first big hypothesis for Alzheimer’s was the cholinergic hypothesis; that there is a paucity of a neurotransmitter called acetylcholine causing the damage. Unfortunately, drugs that increase acetylcholine don’t stop the disease progression. The second big hypothesis, the one that is currently in vogue, is the amyloid cascade hypothesis. According to this theory an amyloid precursor known as amyloid beta (Aβ) is the cause of Alzheimer’s. This makes a lot of sense, as Aβ is the main component of amyloid plaques and people with a genetic predisposition to make extra Aβ tend to get Alzheimer’s (called familial Alzheimer’s). There are a few inconsistencies in this hypothesis: the distribution of Aβ doesn’t match how bad the disease is, and risk factors that increase Aβ don’t match those of Alzheimer’s. To make matters worse, in spite of decades of research, over 99% of clinical research studies targeting Aβ have failed to bring a medication to market.1
Enter the Lipid Invasion Model. This is a new hypothesis developed in 2021 to explain the root cause of Alzheimer’s dementia. The basic idea is that the barrier between the brain and the rest of the body degrades, which allows cholesterols and free fatty acids to “invade” the brain and cause damage. The less basic idea is the rest of this article.
To begin, let’s discuss the barrier between the brain and the body, aptly called the Blood Brain Barrier. The barrier is made up of the blood vessels of the brain. These are special blood vessels with unique properties. The cells that make up the walls of the blood vessels, called epithelial cells, are joined together with tight junctions that keep small charged particles from getting past. These epithelial cells are dotted with special transporters that only let in certain nutrients. Other brain cells called pericytes and astrocytes surround the epithelial cells (on the brain side) and keep out stragglers. This allows the brain to maintain the environmental conditions that it needs to function. Instead of letting a free flow of blood to cells, the blood brain barrier only lets in specific amounts of specific nutrients. One of the key items that is restricted by the blood brain barrier is lipids.
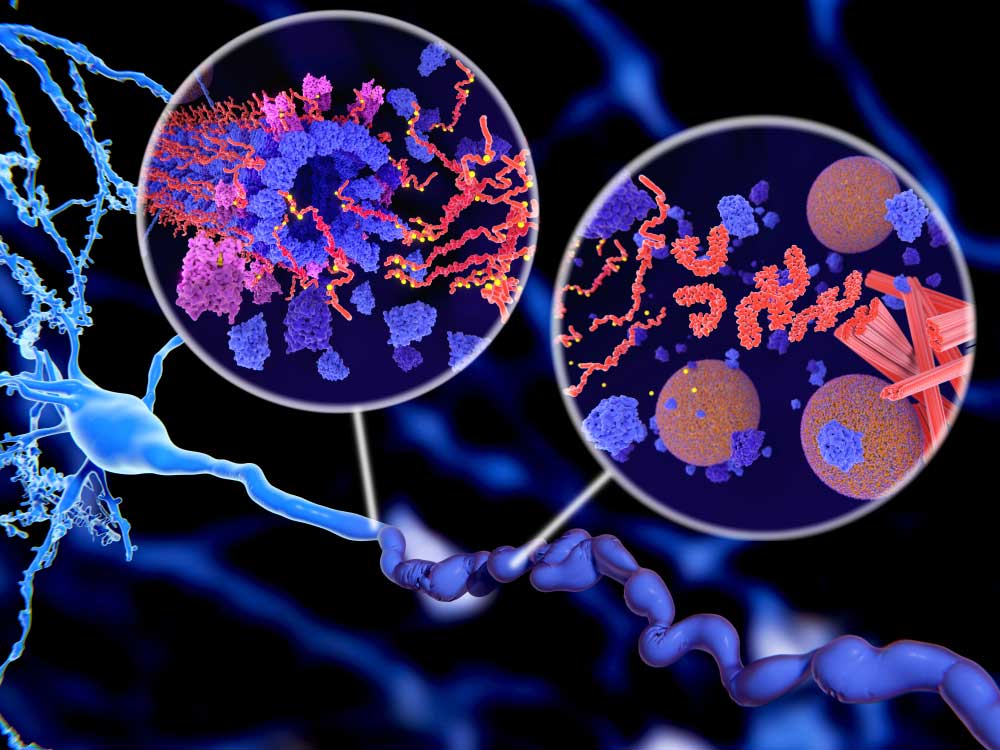
“Lipids” is another name for fats. In the body they perform several vital functions, and in the brain they are critical. Even though the brain is only 2% of the body’s weight, it contains nearly a ¼ of the body’s cholesterol. It uses this for cell repair, creating synapses (learning), releasing communication particles, and for coating neurons to increase the speed of thought. The two lipids relevant to this discussion are cholesterol and free fatty acids. These are energy-dense particles that don’t dissolve in watery liquids like blood. Instead, they need to hitch a ride to be transported through the bloodstream. In the brain, cholesterols and free fatty acids must be transported in small, dense, protein-rich particles called lipoproteins. In the body, lipoproteins come in many different sizes (including low-density lipoproteins, known as LDL). In addition, free fatty acids can be transported in a different protein called albumin. Part of the blood brain barrier’s job is to keep these two systems of transporting lipids separate.
The Lipid Invasion Model postulates that this separation system fails. When this happens the brain can’t handle the extra lipids. Free fatty acids in particular have a detrimental effect. They cause oxidative stress that can result in cell damage and change the energy regulation of neurons, causing problems, and activating immune receptors causing an inflammatory response. Inflammation can result in astrocyte cells producing extra cholesterol, making the problem worse. On top of this, excess lipids in the brain are thought to limit the ability of neurons to grow and cause the amnesia typical of Alzheimer’s. Finally, excessive lipids may cause the brain to create amyloid beta, the precursor to the stereotypical amyloid plaques.
So what goes wrong with the blood brain barrier? Scientists think the barrier degrades over time. Those tight junctions loosen, the transporters let in too many items, or items of the wrong type, and different proteins on the surface of epithelial cells disrupt the barrier. Additionally, microbleeds in the brain let unrestricted blood flow through and interact without the epithelial cells’ consent. The barrier lets the wrong type of materials cross, including lipids. In Alzheimer’s patients, we see free fatty acids and non-brain-native lipoproteins (including the risky APOE4) spread through the brain. The risk factors for blood brain barrier damage are eerily similar to those of Alzheimer’s dementia:
- Aging is the number one risk factor
- Brain trauma (CTE from football has similar symptoms)
- High blood pressure
- Stress
- Lack of sleep
- Smoking
- Drinking
- Obesity
- Diabetes
- Genetic differences
- Amyloid beta – that’s right, Aβ disrupts the blood brain barrier in a cruel feedback loop
So what can we do with this new hypothesis? The most important step is to research it! I need to reiterate that this is only a hypothesis. It’s still only a few years old, and there is no experimental data verifying the veracity of this very vivacious version of Alzheimer’s. There is some early evidence the lipid invasion model may have merit; people on lipid-lowering statin medication have significantly lower rates of Alzheimer’s. If experimentation verifies the hypothesis, we may see new methods of targeting Alzheimer’s, hopefully with a much higher success rate!
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Chaves, J. C., Dando, S. J., White, A. R., & Oikari, L. E. (2023). Blood-brain barrier transporters: An overview of function, dysfunction in Alzheimer’s disease and strategies for treatment. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease, 166967. https://eprints.qut.edu.au/244794/1/151230849.pdf
1Cummings, J. L., Morstorf, T., & Zhong, K. (2014). Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimer’s research & therapy, 6(4), 1-7. https://alzres.biomedcentral.com/articles/10.1186/alzrt269?_ga=2.232085279.1814812906.1525132800-565150820.1525132800
Hu, Z. L., Yuan, Y. Q., Tong, Z., Liao, M. Q., Yuan, S. L., Jian, Y., … & Liu, W. F. (2023). Reexamining the Causes and Effects of Cholesterol Deposition in the Brains of Patients with Alzheimer’s Disease. Molecular Neurobiology, 60(12), 6852-6868. https://link.springer.com/article/10.1007/s12035-023-03529-y
Jick, H. Z. G. L., Zornberg, G. L., Jick, S. S., Seshadri, S., & Drachman, D. A. (2000). Statins and the risk of dementia. The Lancet, 356(9242), 1627-1631. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(00)03155-X/abstract
Rudge, J. D. A. (2022). A new hypothesis for Alzheimer’s disease: The lipid invasion model. Journal of Alzheimer’s Disease Reports, 6(1), 129-161. https://content.iospress.com/articles/journal-of-alzheimers-disease-reports/adr210299
Rudge, J. D. A. (2023). The Lipid Invasion Model: Growing Evidence for This New Explanation of Alzheimer’s Disease. Journal of Alzheimer’s Disease, (Preprint), 1-14.https://content.iospress.com/articles/journal-of-alzheimers-disease/jad221175#ref007
Wang, H., Kulas, J. A., Higginbotham, H., Kovacs, M. A., Ferris, H. A., & Hansen, S. B. (2022). Regulation of neuroinflammation by astrocyte-derived cholesterol. bioRxiv, 2022-12. https://doi.org/10.1101/2022.12.12.520161
Xiong, H., Callaghan, D., Jones, A., Walker, D. G., Lue, L. F., Beach, T. G., … & Zhang, W. (2008). Cholesterol retention in Alzheimer’s brain is responsible for high β-and γ-secretase activities and Aβ production. Neurobiology of disease, 29(3), 422-437. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2720683/