Scroll down to listen to this article.
The immune system is awesome, but overwhelming. It’s filled with billions of cells and quintillions of proteins. There are neutrophils, dendritic cells, antibodies, B cells, macrophages, lymphoid cells, lymphocytes, the complement system, and more! Instead of trying to understand the whole thing, let’s narrow our focus down to just one type of cell, the T cell, and just one variant, T-helper 17, or Th17.
T-cells are a type of white blood cell and are about the size of a red blood cell. They are adaptive, which means they change in response to threats. These cells start as virgin (or naïve) cells and transform into a specialized version when danger is detected. T-cells can be divided into two parts: killers and helpers. Killers are good at killing other (hopefully bad) cells, while helpers activate other cells and amplify immune responses. The cell we’re focusing on, Th17, is a type of helper cell, but a special one.
Th17 was first identified in 2005, but scientists have rapidly learned loads about it. It is particularly good at helping the body fight unusual attackers like fungi and certain bacteria. When activated, it releases a powerful signaling chemical that increases inflammation and recruits other white blood cells, telling them to come and fight. In addition, it can assist in tightening the spaces between our border cells to keep invaders out. When the body detects unknown particles, cells release signaling molecules. When a T-helper cell encounters the right mix of these molecules, it transforms into the rallying Th17 captain which sounds the alarm.
Unfortunately, all that shimmers is not silver. Th17 can certainly be useful in some circumstances, but it can be dangerous when activated by the wrong signals. In many of these cases, Th17 cells tell white blood cells to go nuts and attack anything that moves (or doesn’t move), but without a clear opponent, they just attack whatever’s around and cause an autoimmune response. Th17 has been implicated in diseases like experimental autoimmune encephalomyelitis (EAE), arthritis, and inflammatory bowel diseases (IBD) like Ulcerative Colitis. Let’s look at ulcerative colitis as an example.
Ulcerative colitis is an inflammatory bowel disease where the immune system attacks benign bacteria or food particles. The causes aren’t clear, but part of the problem is a thinning of the mucus and separation of border cells that line the intestines. Many signaling molecules called interleukins (abbreviated IL-) are released in the disease state, including three important ones for Th17. These are IL-1β, IL-6, and IL-23 (write this down for the quiz at the end). The first two activate Th17, and that’s when IL-23 can turn it into a problem. In the presence of IL-23, Th17 sends wild signals and can cause the autoimmune problems listed above, including ulcerative colitis. Also, remember how Th17 helps tighten the spaces between border cells? It turns out that in the presence of IL-23 this function doesn’t work properly and the borders stay open, letting in more particles that the body attacks with inflammation.
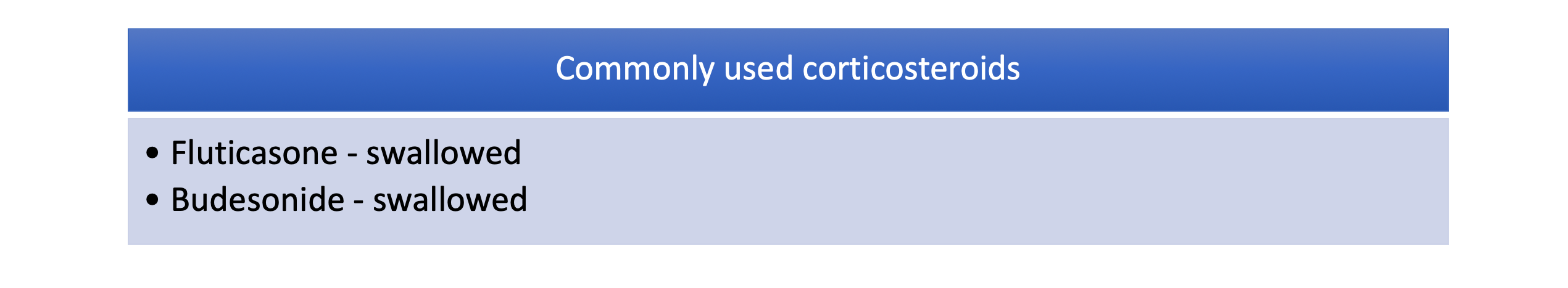
Scientists have been trying to find ways to solve the problems caused by Th17 since long before it was even known to exist. In the past, a treatment for something like ulcerative colitis might have been limited to restricting your diet. Currently, anti-inflammatory medications, steroids, and/or surgeries are used. Those are all big solutions bound to affect many other parts of the body and immune system. Now that Th17 has been identified as an occasional dirty traitor, researchers are instead targeting this specific cell to hopefully stop it from being activated incorrectly. With luck, we can help the T-helper cell to help us instead of unhelping us.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Kałużna, A., Olczyk, P., & Komosińska-Vassev, K. (2022). The role of innate and adaptive immune cells in the pathogenesis and development of the inflammatory response in ulcerative colitis. Journal of clinical medicine, 11(2), 400. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8780689/
Sender, R., Weiss, Y., Navon, Y., Milo, I., Azulay, N., Keren, L., … & Milo, R. (2023). The total mass, number, and distribution of immune cells in the human body. Proceedings of the National Academy of Sciences, 120(44), e2308511120. https://doi.org/10.1073/pnas.2308511120
Tesmer, L. A., Lundy, S. K., Sarkar, S., & Fox, D. A. (2008). Th17 cells in human disease. Immunological reviews, 223(1), 87-113. https://doi.org/10.1111/j.1600-065X.2008.00628.x
Wu, B., & Wan, Y. (2020). Molecular control of pathogenic Th17 cells in autoimmune diseases. International immunopharmacology, 80, 106187. https://doi.org/10.1016/j.intimp.2020.106187