When a looming deadline stresses me out, I often remember the classic advice to take a deep breath – but what if you can’t? This may be the case for people with chronic obstructive pulmonary disease, also called COPD. COPD is a progressive lung disease that may feel like you are trying to breathe through a tiny cocktail straw. This difficulty in breathing is caused by the deterioration of the structure of the lungs. It affects around 10% of the global population and nearly 15% of Americans, resulting in approximately 150 thousand deaths per year in the US. COPD rates increase as socioeconomic status drops, meaning it is more prevalent among poorer individuals.
COPD symptoms can range from mild to severe. Shortness of breath, cough, and excess phlegm are common. More severe COPD can result in hospitalization and death. Cardiovascular disease, diabetes, obesity, and chronic bronchitis both affect and are affected by COPD. Lifelong accumulation of damage to the lungs characterizes COPD, with risk factors including most things that affect lung health. Some risk factors can’t be helped, like genetics or lung development from childhood. Others are environmental, including air pollution and infections like tuberculosis or HIV. Several risks can be mitigated through lifestyle choices, the most important being smoking. Smoking directly puts destructive particles into your lungs, greatly increasing your chances of developing COPD. This includes cigarettes, but also vaping, and marijuana. Inactivity, a poor diet, and jobs that expose you to particulate matter, like stone dust and pesticides, also contribute. The final risk factor is time. Lung capacity peaks in your early 20s and damage to the lungs from the above causes accumulates over time. So how do these things cause damage, and what can we do about it?
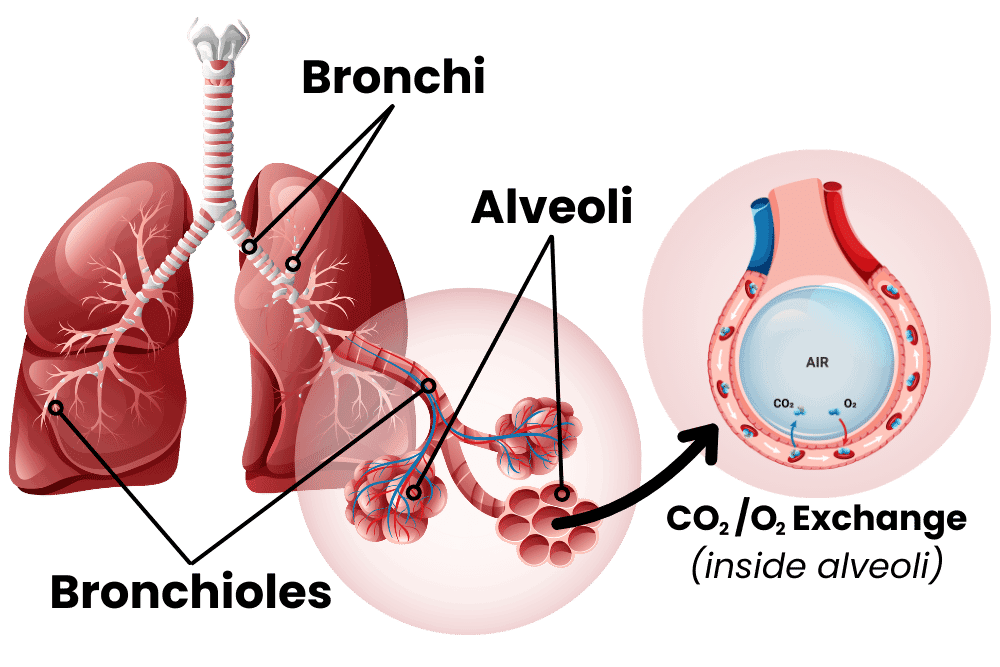
To understand COPD, let’s first inhale a little crash course on the lungs. I always see lungs drawn like they’re giant balloons, but they’re really more like sponges. The airway moves from the big throat to smaller and smaller fractal channels called bronchi and bronchioles until they reach the alveoli. These are teeny-tiny little balloons, and there are hundreds of millions of them in the lungs. These tiny sacs have thin walls and are the interface between air and blood, allowing for carbon dioxide to be exchanged for fresh oxygen. The tiny sacs provide a lot of surface area for this exchange to take place. Altogether, the inner surface of all the alveoli is called the lung parenchymal, and its surface area is close to the size of a tennis court! The lungs can’t expand on their own, so the smooth muscle of the lungs keeps bronchi and bronchioles from collapsing. When the lung is damaged over time, COPD may occur. This damage manifests in the airway, the alveoli, or both.
The airway, made up of bronchi and bronchioles, can become inflamed, resulting in bronchitis (bronchi + itis, meaning inflammation of). The lungs have their own immune system, including a slimy mucus layer, but chronic insults to the lungs (like smoking for years and years) can degrade this system. With bronchitis, big and dangerous immune cells like macrophages, neutrophils, and lymphocytes may enter the lungs. These cells are good at removing invaders but can cause damage to surrounding tissue through inflammation. When the damage lasts for years, this chronic inflammation can narrow the airways, degrade tissue, and cause a thickening or scarring of lung tissue called fibrosis. The end result of all of this is increased resistance from the airway: it’s harder for the lungs to draw in air. Emphysema occurs when the lung parenchymal is damaged. Alveoli are destroyed, some of them combine into larger holes, and functional surface area is reduced. This reduces the lungs’ capacity and elasticity, making them less able to deflate. The combined effects of bronchitis and emphysema lower lung function – you can’t exchange as much carbon dioxide for oxygen.
So what can we do to fix COPD? The first step is to stop the damage. Smokers with COPD should stop immediately. Quitting smoking can be extremely hard, especially as many smokers started in their teens when the brain was still cementing lifelong habits. You should also improve other modifiable lifestyle risks; increase exercise, make sure your diet is healthy, and try to reduce exposure to air pollution. Doctors recommend lowering the risks of exacerbating infections by getting vaccines for flu, RSV, COVID, pneumonia, and Tdap. Beyond these measures, pharmacology can provide relief. Medical treatments are generally added in a stepwise, increasing fashion to control symptoms and to reduce exacerbations with a minimum of side effects.
The major available medications are usually lumped into bronchodilators and antimuscarinic drugs. Bronchodilators do just what it sounds like they do, they dilate (expand) the bronchi and bronchioles. Beta2 agonists are the archetypal bronchodilators, they change the function of lung muscle and widen airways. They can be short-acting beta-agonists (SABA) or long-acting (LABA). Antimuscarinic drugs are similar. They act on muscarinic receptors in smooth muscle. These receptors regulate bronchodilation, mucus secretion, and inflammation. There are short and long-acting muscarinic receptor antagonists (SAMA and LAMAs). On top of these, an inhaled corticosteroid (ICS) may help reduce inflammation. LABA medications may increase the effectiveness of ICS inflammation reduction. When a single medication fails to control symptoms or stop complications, a dual medication of LABA + ICS or LABA + LAMA may be prescribed. Mounting evidence is also showing that a triple medication of LABA + LAMA + ICS may provide advanced relief when a dual medication isn’t sufficient. If these combination medications pan out, those with COPD may be able to finally breathe a sigh of relief.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Adeloye, D., Chua, S., Lee, C., Basquill, C., Papana, A., Theodoratou, E., … & Global Health Epidemiology Reference Group (GHERG. (2015). Global and regional estimates of COPD prevalence:
Systematic review and meta–analysis. Journal of global health, 5(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4693508/
Alagha, K., Palot, A., Sofalvi, T., Pahus, L., Gouitaa, M., Tummino, C., … & Chanez, P. Íp(2014). Long-acting muscarinic receptor antagonists for the treatment of chronic airway diseases. Therapeutic advances in chronic disease, 5(2), 85-98. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3926345/
GOLD, 2023 Global Initiative for Chronic Obstructive Lung Disease (GOLD). (2023). 2023 Report: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. https://goldcopd.org
Rabe, K. F., Martinez, F. J., Ferguson, G. T., Wang, C., Singh, D., Wedzicha, J. A., … & Dorinsky, P. (2020). Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. New England Journal of Medicine, 383(1), 35-48. https://www.nejm.org/doi/10.1056/NEJMoa1916046
Suki, B., Stamenovic, D., & Hubmayr, R. (2011). Lung parenchymal mechanics. Comprehensive Physiology, 1(3), 1317. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3929318/
CDC & National Center for Health Statistics. (May 2, 2024). Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm