GRID VIEW
Alzheimer’s disease is probably my biggest fear. Unfortunately, this means the anxiety surrounding it can also be debilitating. If I forget a coworker’s name, is that a sign? What if I “forget” that pizza is not on the whole 30 diet? Jokes aside, worrying about Alzheimer’s can interfere with daily life. So, how can you differentiate between the normal lapses we all get, changes due to aging, and the serious brain alterations that occur during Alzheimer’s dementia? On the MedEvidence!™ Podcast Neurologist Stephen Toenjes, MD, describes the key factor of Alzheimer’s, “there are normal changes that are associated with aging. But we do not lose our memory as we age. If there’s memory loss, there is something wrong. There is damage [1].” He continues by having us imagine “somebody put the milk in the cabinet. I just ask, ‘Where does the milk go?’ And the patient will say ‘In the refrigerator’. And that illustrates that the person knows that the milk goes in the refrigerator. They didn’t forget that it goes in the refrigerator, they just weren’t paying attention to what they were doing. [1]” A patient with Alzheimer’s would not remember where the milk goes. This differentiation between brain changes due to normal aging and those due to Alzheimer’s can pose real challenges for doctors; diagnosing Alzheimer’s can be a long and complex process [2]. Many of the steps to diagnose Alzheimer’s are investigations into other things that may be causing mental changes. Unfortunately, there are currently no cures for Alzheimer’s dementia, though clinical trials are actively attempting to fill this void [2]. An early diagnosis may be particularly important for those seeking a clinical trial for Alzheimer’s because the disease gets worse over time. We may not be able to reverse the effects of Alzheimer’s dementia, but the earlier a patient receives treatments being developed, the more effective they can be at preventing decline [2]. Creative Director Benton Lowey-Ball, BS, BFA
References: [1] Koren, MJ. Toenjes, S. & McKormick, M. (13 April, 2022). Is it Alzheimer’s or something else? In MedEvidence! Truth Behind the Data [Podcast]. [2] National Institute on Aging. (8 December, 2022) How is Alzheimer’s disease diagnosed? U.S. Department of Health and Human Services, National Institutes of Health. https://www.nia.nih.gov/health/alzheimers-symptoms-and-diagnosis/how-alzheimers-disease-diagnosed [3] Jack Jr, C. R., Andrews, J. S., Beach, T. G., Buracchio, T., Dunn, B., Graf, A., … & Carrillo, M. C. (2024). Revised criteria for diagnosis and staging of Alzheimer’s disease: Alzheimer’s Association Workgroup. Alzheimer’s & Dementia, 20(8), 5143-5169. https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.13859
Scroll down to listen to this article.
Listen to the article here:
https://medevidence.com/dementia-vs-alzheimers
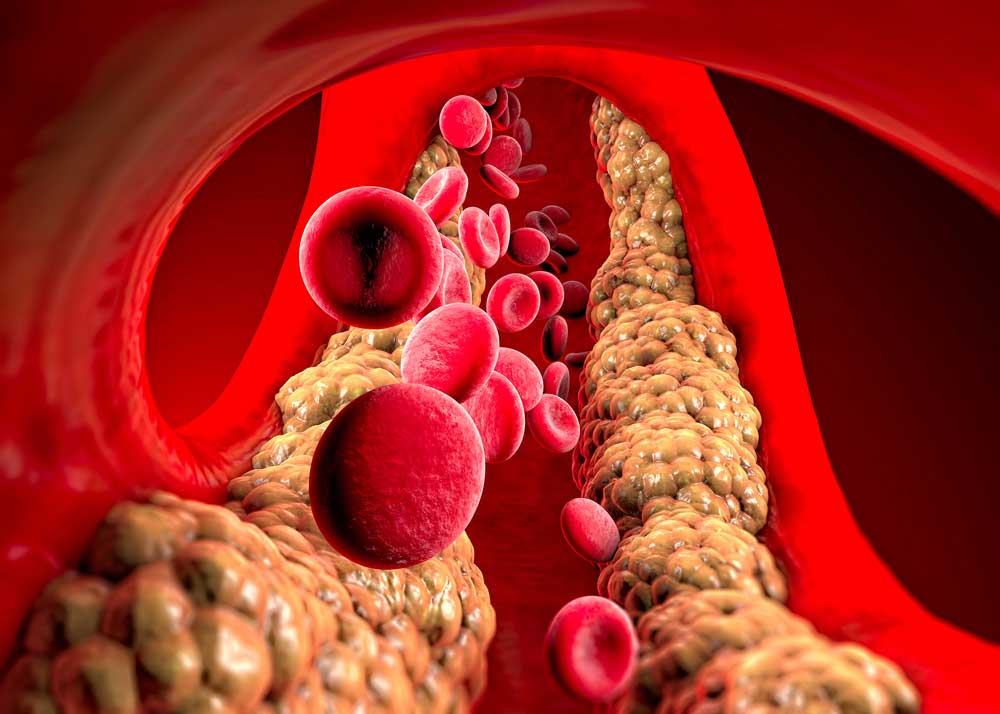
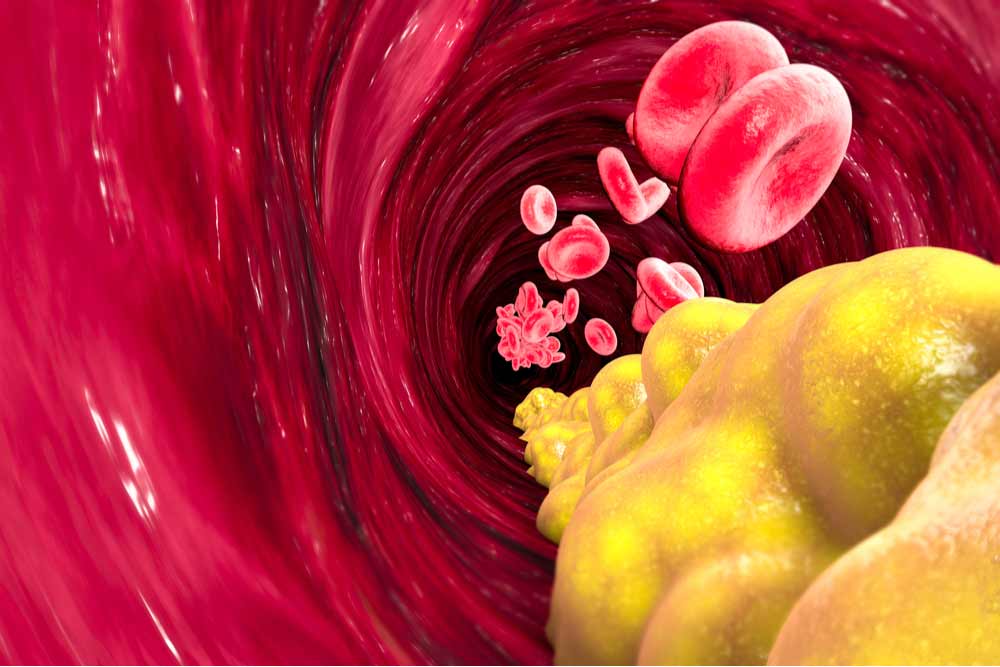
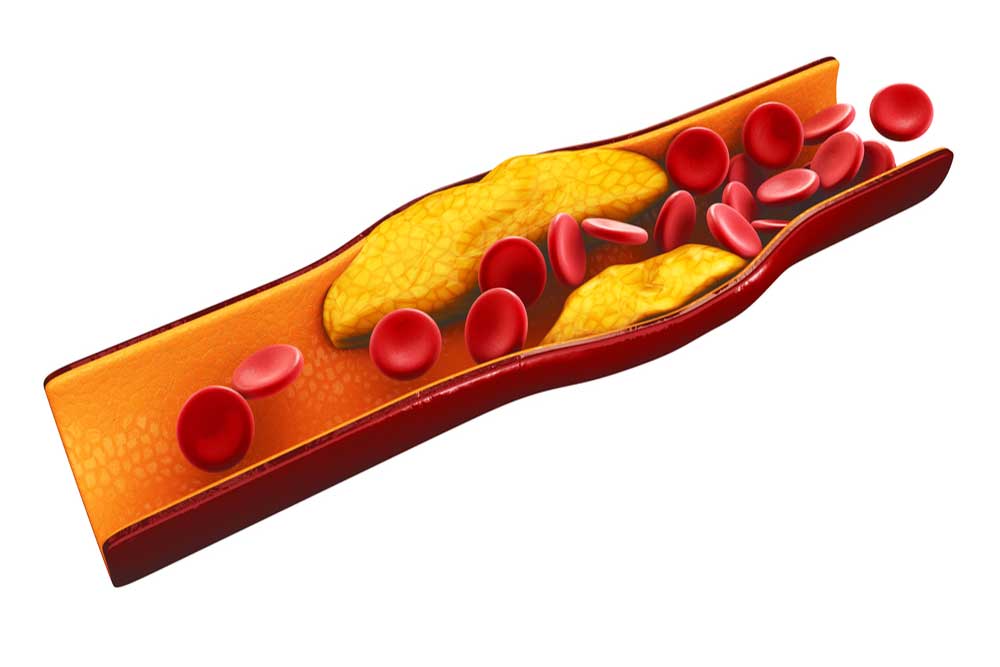
Have you noticed people sunbathing at the beach? They often try to get smooth, shiny, tanned legs. However, if your skin appears shiny, hairless, and changes color without explanation, it’s worth consulting a doctor—these could be signs of peripheral artery disease. Peripheral artery disease (PAD) is precisely what it sounds like, a disease affecting the peripheral arteries. Arteries carry oxygenated blood from the heart all over the body, and the “peripheral arteries” are those outside of the heart and brain. The exact criteria for what causes this low blood flow isn’t always well-defined, which makes statistics a little iffy, but around 6-7% of people in America have PAD [1, 2]. This number is higher in African Americans than in other groups, and the risk increases with age [2]. Peripheral Artery Disease (PAD) most frequently damages the arteries responsible for supplying oxygen to the legs, which is why symptoms typically manifest in the legs before affecting other areas of the body. Symptoms include: These sound painful and aggravating, and if left untreated PAD can have serious consequences. Low blood flow to the limbs can result in the need for amputation. On top of this, PAD is indicative of bigger problems with the cardiovascular system and may present a higher risk for heart attack, stroke, and death. All these complications can make sunbathing less enjoyable. With PAD, low blood flow typically occurs in medium or large vessels. The walls of these vessels may narrow from plaques in a process called atherosclerosis, or they may become blocked by a blood clot called thrombosis. There are a few other potential limiters of blood flow, though the strictest definition of PAD is from atherosclerosis alone. In response to low blood flow to the area, the body tries to compensate by growing new arteries and changing muscle composition, especially in the calves. When the body can’t effectively compensate, muscles are reduced, fat increases, and the small blood vessels stop working properly. This can lead to an accumulation of fats, limited waste clearance, and inflammation. Altogether, fats in the skin can leave it shiny, low blood supply can change the color, and reduced oxygen in hair follicles can cause them to function improperly or die, leaving the skin smooth and hairless [3]. Conditions that may indicate risk: [4, 1] So what can be done? The first step is diagnosis. The classical symptom of calf cramping pain (intermittent claudication) isn’t present in a majority of PAD patients [1]. Those at higher risk (such as smokers with type 2 diabetes) may want to take an ankle-brachial index (ABI), which is a quick, non-invasive test comparing the blood pressure in the upper arms to the blood pressure in the ankles. If a healthcare provider diagnoses PAD, they can offer several possible solutions. Treatments that help lower the risk of major cardiovascular problems are critical. A doctor may prescribe aspirin or other medications that lower the chance of blood clots, or statins that lower the circulating fats in the blood [5]. Smokers may be encouraged to quit or be prescribed the use of smoking cessation tools. Other medications may be prescribed to target associated conditions like high blood pressure or diabetes, further reducing risk to the cardiovascular system. Several treatments target PAD specifically, including exercise. Supervised, structured exercise – including treadmill and resistance training, may help reduce pain and increase leg function. It may be as simple as walking on the beach instead of lying in the sunchair to get that tan. Special medications like cilostazol target arterial muscles. Advanced cases of PAD may require revascularization, where the arteries are cleared using surgery or other means. Proper footwear may also help, and clinical trials continue to search for new treatments for PAD. These may include therapies that target cells or genes and new ways to revascularize peripheral arteries without surgery. So the next time your legs look like a sunbather’s dream (but your arms don’t), consider checking with your doctor and local clinical research center to look for care options. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: [1] Golledge, J. (2022). Update on the pathophysiology and medical treatment of peripheral artery disease. Nature reviews cardiology, 19(7), 456-474. https://www.nature.com/articles/s41569-021-00663-9 [2] Allison, M. A., Ho, E., Denenberg, J. O., Langer, R. D., Newman, A. B., Fabsitz, R. R., & Criqui, M. H. (2007). Ethnic-specific prevalence of peripheral arterial disease in the United States. American journal of preventive medicine, 32(4), 328-333. https://www.sciencedirect.com/science/article/pii/S0749379706005587 [3] Dean, S. M. (2018). Cutaneous manifestations of chronic vascular disease. Progress in Cardiovascular Diseases, 60(6), 567-579. https://www.sciencedirect.com/science/article/pii/S0033062018300549?via=ihub [4] Fowkes, F. G. R., Aboyans, V., Fowkes, F. J., McDermott, M. M., Sampson, U. K., & Criqui, M. H. (2017). Peripheral artery disease: epidemiology and global perspectives. Nature Reviews Cardiology, 14(3), 156-170. https://www.nature.com/articles/nrcardio.2016.179 [5] Gerhard-Herman, M. D., Gornik, H. L., Barrett, C., Barshes, N. R., Corriere, M. A., Drachman, D. E., … & Walsh, M. E. (2017). 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 135(12), e686-e725. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000470 Related Reading Umuerri, E. M. (2019). Skin manifestations of peripheral artery disease: Prevalence and diagnostic utility. Journal of Clinical and Preventive Cardiology, 8(3), 121-125.
When a looming deadline stresses me out, I often remember the classic advice to take a deep breath – but what if you can’t? This may be the case for people with chronic obstructive pulmonary disease, also called COPD. COPD is a progressive lung disease that may feel like you are trying to breathe through a tiny cocktail straw. This difficulty in breathing is caused by the deterioration of the structure of the lungs. It affects around 10% of the global population and nearly 15% of Americans, resulting in approximately 150 thousand deaths per year in the US. COPD rates increase as socioeconomic status drops, meaning it is more prevalent among poorer individuals. COPD symptoms can range from mild to severe. Shortness of breath, cough, and excess phlegm are common. More severe COPD can result in hospitalization and death. Cardiovascular disease, diabetes, obesity, and chronic bronchitis both affect and are affected by COPD. Lifelong accumulation of damage to the lungs characterizes COPD, with risk factors including most things that affect lung health. Some risk factors can’t be helped, like genetics or lung development from childhood. Others are environmental, including air pollution and infections like tuberculosis or HIV. Several risks can be mitigated through lifestyle choices, the most important being smoking. Smoking directly puts destructive particles into your lungs, greatly increasing your chances of developing COPD. This includes cigarettes, but also vaping, and marijuana. Inactivity, a poor diet, and jobs that expose you to particulate matter, like stone dust and pesticides, also contribute. The final risk factor is time. Lung capacity peaks in your early 20s and damage to the lungs from the above causes accumulates over time. So how do these things cause damage, and what can we do about it?
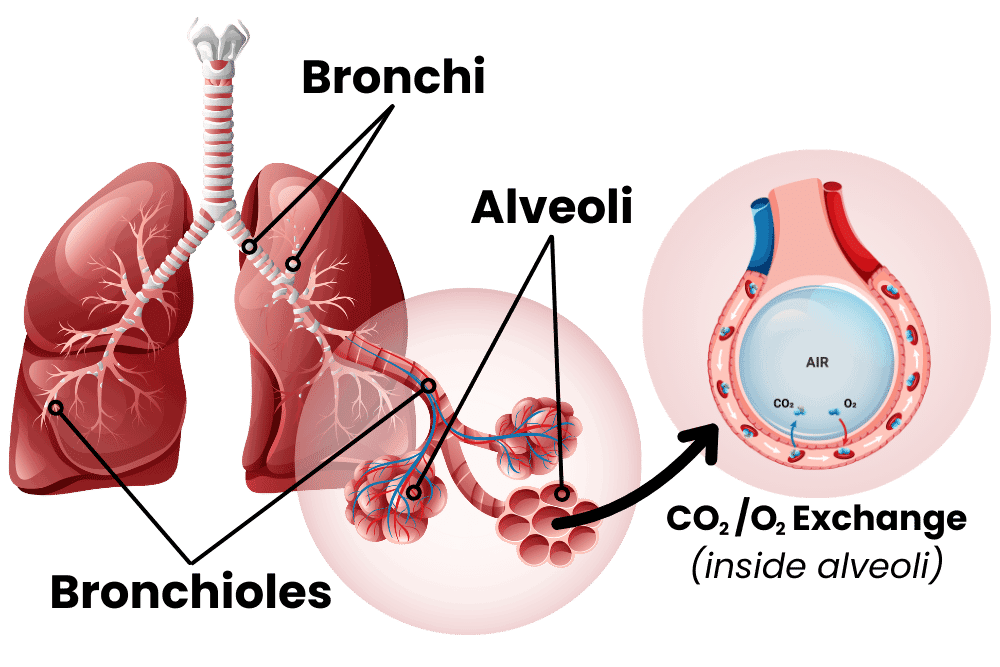
To understand COPD, let’s first inhale a little crash course on the lungs. I always see lungs drawn like they’re giant balloons, but they’re really more like sponges. The airway moves from the big throat to smaller and smaller fractal channels called bronchi and bronchioles until they reach the alveoli. These are teeny-tiny little balloons, and there are hundreds of millions of them in the lungs. These tiny sacs have thin walls and are the interface between air and blood, allowing for carbon dioxide to be exchanged for fresh oxygen. The tiny sacs provide a lot of surface area for this exchange to take place. Altogether, the inner surface of all the alveoli is called the lung parenchymal, and its surface area is close to the size of a tennis court! The lungs can’t expand on their own, so the smooth muscle of the lungs keeps bronchi and bronchioles from collapsing. When the lung is damaged over time, COPD may occur. This damage manifests in the airway, the alveoli, or both. The airway, made up of bronchi and bronchioles, can become inflamed, resulting in bronchitis (bronchi + itis, meaning inflammation of). The lungs have their own immune system, including a slimy mucus layer, but chronic insults to the lungs (like smoking for years and years) can degrade this system. With bronchitis, big and dangerous immune cells like macrophages, neutrophils, and lymphocytes may enter the lungs. These cells are good at removing invaders but can cause damage to surrounding tissue through inflammation. When the damage lasts for years, this chronic inflammation can narrow the airways, degrade tissue, and cause a thickening or scarring of lung tissue called fibrosis. The end result of all of this is increased resistance from the airway: it’s harder for the lungs to draw in air. Emphysema occurs when the lung parenchymal is damaged. Alveoli are destroyed, some of them combine into larger holes, and functional surface area is reduced. This reduces the lungs’ capacity and elasticity, making them less able to deflate. The combined effects of bronchitis and emphysema lower lung function – you can’t exchange as much carbon dioxide for oxygen. So what can we do to fix COPD? The first step is to stop the damage. Smokers with COPD should stop immediately. Quitting smoking can be extremely hard, especially as many smokers started in their teens when the brain was still cementing lifelong habits. You should also improve other modifiable lifestyle risks; increase exercise, make sure your diet is healthy, and try to reduce exposure to air pollution. Doctors recommend lowering the risks of exacerbating infections by getting vaccines for flu, RSV, COVID, pneumonia, and Tdap. Beyond these measures, pharmacology can provide relief. Medical treatments are generally added in a stepwise, increasing fashion to control symptoms and to reduce exacerbations with a minimum of side effects. The major available medications are usually lumped into bronchodilators and antimuscarinic drugs. Bronchodilators do just what it sounds like they do, they dilate (expand) the bronchi and bronchioles. Beta2 agonists are the archetypal bronchodilators, they change the function of lung muscle and widen airways. They can be short-acting beta-agonists (SABA) or long-acting (LABA). Antimuscarinic drugs are similar. They act on muscarinic receptors in smooth muscle. These receptors regulate bronchodilation, mucus secretion, and inflammation. There are short and long-acting muscarinic receptor antagonists (SAMA and LAMAs). On top of these, an inhaled corticosteroid (ICS) may help reduce inflammation. LABA medications may increase the effectiveness of ICS inflammation reduction. When a single medication fails to control symptoms or stop complications, a dual medication of LABA + ICS or LABA + LAMA may be prescribed. Mounting evidence is also showing that a triple medication of LABA + LAMA + ICS may provide advanced relief when a dual medication isn’t sufficient. If these combination medications pan out, those with COPD may be able to finally breathe a sigh of relief. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Adeloye, D., Chua, S., Lee, C., Basquill, C., Papana, A., Theodoratou, E., … & Global Health Epidemiology Reference Group (GHERG. (2015). Global and regional estimates of COPD prevalence: Systematic review and meta–analysis. Journal of global health, 5(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4693508/ Alagha, K., Palot, A., Sofalvi, T., Pahus, L., Gouitaa, M., Tummino, C., … & Chanez, P. Íp(2014). Long-acting muscarinic receptor antagonists for the treatment of chronic airway diseases. Therapeutic advances in chronic disease, 5(2), 85-98. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3926345/ GOLD, 2023 Global Initiative for Chronic Obstructive Lung Disease (GOLD). (2023). 2023 Report: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. https://goldcopd.org Rabe, K. F., Martinez, F. J., Ferguson, G. T., Wang, C., Singh, D., Wedzicha, J. A., … & Dorinsky, P. (2020). Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. New England Journal of Medicine, 383(1), 35-48. https://www.nejm.org/doi/10.1056/NEJMoa1916046 Suki, B., Stamenovic, D., & Hubmayr, R. (2011). Lung parenchymal mechanics. Comprehensive Physiology, 1(3), 1317. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3929318/ CDC & National Center for Health Statistics. (May 2, 2024). Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
Listen to the article here:
As an avid surfer, I occasionally hear concerns about shark attacks at the beach. Diving into the statistics of unprovoked shark attacks, I learned that they are astronomically unlikely. Deaths are even rarer, with only around one fatal shark attack per year in the U.S. So then what is the deadliest animal? Worldwide, scorpions kill a few thousand people annually, dogs around ten thousand annually, and snakes kill some 75,000 people a year! That’s a drop in the bucket compared to other humans, who kill around half a million people per year. But then there are mosquitoes. Mosquitoes kill more people than every other animal combined – including humans; something like 750,000 to 1 million people per year. Let’s get the buzz on why. Mosquitoes don’t kill us directly. At least not normally. Sometimes blood loss from mosquito bites can kill animals as big as cows, but this is an exception rather than the rule. Normally, mosquitoes kill people by acting as vectors, which transmit disease. The deadliest known disease in the history of the planet is malaria, and it is responsible for at least several billion deaths throughout history (the exact number is quite controversial, with estimates ranging from 5% – 50% of all people ever to live). Mosquitos also transmit dengue, yellow fever, chikungunya, zika, and more. The question then is… why? Why us in particular? Actually, only some mosquitoes like humans in particular. There are around 3,600 types of mosquito. Some species, like Aedes aegypti (a-ee-dees a-gyp-thai), hunt humans specifically for blood. Others target snakes, frogs, or birds. Many are generalists and hunt anything with blood. However, consuming blood is actually a rare occurrence in the life of a mosquito. For most of their lives mosquitoes are vegetarians. They eat plant nectar, fruits, and the sugary waste of aphids called honeydew. Mosquitoes pollinate flowers, like to eat apples and bananas, and wanna hang out for a nice long walk on the beach. Some mosquito species actually stay vegetarian their whole lives. In fact, male mosquitoes don’t consume our blood, it’s only females when they need to lay eggs. Fruit juice is nice, but – as every good vegan knows – you need to get your protein somehow. For mosquitoes, some species need the extra protein found in blood to help their young thrive. How mosquitoes actually locate a host is pretty complex. It’s easy to guess how a mosquito might find us by looking at what signals we give off. We breathe, we smell, we’re warm, we look like people, and we taste like humans. Each of these features attract mosquitoes from progressively shorter distances. Let’s move through how. People exhibit variations on all these areas (except for breathing). Our smells change, some of us wear insulating clothes, skin tones vary, and according to Dr. Hannibal Lecter, we taste different. Scientists have studied the variation between people and how many mosquitoes bite them in an effort to seek relief from mosquito bites. Mosquitoes tend to bite pregnant individuals more frequently and genetics play a role, but these factors are difficult to alter in many people. Instead, researchers tend to target our most modifiable attractant, smell. Our skin microbiome and genes affect our scent, but diet seems to as well – though not as much as many people claim. Randomized clinical trials have found no evidence that vitamin B, garlic, and green grapes affect mosquito bites. There is some preliminary evidence pointing to caffeine as a possible attractant. Studies have found evidence that eating bananas and drinking beer both increase mosquito interest. As stated before, having malaria makes you more attractive to mosquitoes. Unfortunately, you may have noticed that none of these reduce our attractiveness to mosquitoes. Bug spray containing DEET makes it more difficult for bugs to smell you and is recommended, but can be sticky, stinky, and unpleasant to use. Next-generation bug repellents may block multiple scents or even inhibit the cpA neurons directly! Physical barriers like long sleeves can help as long as they don’t overheat you. Really, the problem is best summarized in a paper by Van Breygel et al. (2015): For a human hoping to avoid being bitten by a mosquito, our results underscore a number of unfortunate realities. Even if it were possible to hold one’s breath indefinitely, another human breathing nearby, or several meters upwind, would create a CO2 plume that could lead mosquitoes close enough to you that they may lock on to your visual signature. The strongest defense is therefore to become invisible, or at least visually camouflaged. Even in this case, however, mosquitoes could still locate you by tracking the heat signature of your body provided they get close enough. The independent and iterative nature of the sensory-motor reflexes renders mosquitoes’ host seeking strategy annoyingly robust. The obvious reaction to this is to think “kill ‘em all!” Unfortunately, even this method fails. Insecticides have a nasty habit of prompting natural selection to favor bugs immune to them – and they manage to kill many innocent bugs in the process. Traps have limited effectiveness, can be expensive, and also manage to murder countless other ecologically important bugs. With this in mind, perhaps the solution to saving lives from the world’s deadliest animal isn’t in reducing our attractiveness (my mom tells me I’m very attractive), but in reducing our susceptibility to the diseases they carry. Across the globe, scientists are in various stages of research seeking vaccines for malaria, dengue, and other mosquito-borne diseases. If these manage to be successfully tested and distributed, maybe we won’t have anything to fear from mosquitoes after all! Except for the itching. And the annoyance. And the constant ankle biting. And that they like to fly at our eyeballs. And that they might literally take more blood out of us than those sharks everyone tells me to watch out for. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Associated Press. (September 9, 2020). Thick clouds of mosquitoes kill livestock after hurricane. https://apnews.com/article/horses-animals-insects-storms-hurricane-laura-fa0d05b046357864ad2f4bb952ff2e3e CDC Global Health Center. (April 8, 2024). Fighting the world’s deadliest animal. Centers for Disease and Control. https://www.cdc.gov/global-health/impact/fighting-the-worlds-deadliest-animal.html Brown, J. E., Evans, B. R., Zheng, W., Obas, V., Barrera-Martinez, L., Egizi, A., … & Powell, J. R. (2014). Human impacts have shaped historical and recent evolution in Aedes aegypti, the dengue and yellow fever mosquito. Evolution, 68(2), 514-525. https://academic.oup.com/evolut/article/68/2/514/6852391 Ellwanger, J. H., da Cruz Cardoso, J., & Chies, J. A. B. (2021). Variability in human attractiveness to mosquitoes. Current Research in Parasitology & Vector-borne Diseases, 1, 100058. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8906108/ U.S. Environmental Protection Agency. (September 25, 2023). Insect repellents: DEET. https://www.epa.gov/insect-repellents/deet Giraldo, D., Rankin-Turner, S., Corver, A., Tauxe, G. M., Gao, A. L., Jackson, D. M., … & McMeniman, C. J. (2023). Human scent guides mosquito thermotaxis and host selection under naturalistic conditions. Current Biology, 33(12), 2367-2382. https://www.cell.com/current-biology/abstract/S0960-9822(23)00532-8 Peach, D. A., & Gries, G. (2020). Mosquito phytophagy–sources exploited, ecological function, and evolutionary transition to haematophagy. Entomologia Experimentalis et Applicata, 168(2), 120-136. https://doi.org/10.1111/eea.12852 Potter, C. J. (2014). Stop the biting: targeting a mosquito’s sense of smell. Cell, 156(5), 878-881.https://www.sciencedirect.com/science/article/pii/S0092867414001585 Raji, J. I., & DeGennaro, M. (2017). Genetic analysis of mosquito detection of humans. Current opinion in insect science, 20, 34-38.https://www.sciencedirect.com/science/article/pii/S2214574517300342 Shen, H. H. (2017). How do mosquitoes smell us? The answers could help eradicate disease. Proceedings of the National Academy of Sciences, 114(9), 2096-2098 .https://www.pnas.org/doi/10.1073/pnas.1701738114 Tauxe, G. M., MacWilliam, D., Boyle, S. M., Guda, T., & Ray, A. (2013). Targeting a dual detector of skin and CO2 to modify mosquito host seeking. Cell, 155(6), 1365-1379. https://www.cell.com/cell/fulltext/S0092-8674(13)01426-8 Van Breugel, F., Riffell, J., Fairhall, A., & Dickinson, M. H. (2015). Mosquitoes use vision to associate odor plumes with thermal targets. Current Biology, 25(16), 2123-2129.https://www.sciencedirect.com/science/article/pii/S096098221500740X
Listen to the article here:
Last week we talked about the actions of the Nazis, which resulted in the World Medical Association’s Declaration of Helsinki. The declaration provides an ethical guideline for physicians engaging in research involving humans. It has since become a requirement in most medical research. Unfortunately, in America, a study that began seven years prior to World War II undermined this ideal. It wouldn’t be until the 1970s that this study was exposed, and America was faced with its own dark practice of human research. In 1932, doctors at the Tuskegee Institute (Now called Tuskegee University) started a fundamentally unethical experiment. The road to this study winds from good intentions to simple, terrible means. The historical context behind the study involves the Julius Rosenwald Fund, a wholly honorable philanthropic endeavor. This fund built schools in the South, funded Booker T. Washington to attend the Tuskegee Institute, and worked with the U.S. Public Health Service to provide medical services to the poorest Black Americans in the South. One of these medical service endeavors was providing syphilis treatment. Part of this effort involved cataloging the rate of syphilis in several areas. The great depression and Julius Rosenwald’s death brought much of this to a halt, and the syphilis project ended in 1932. Other scientists wanted to pick up where the Julius Rosenwald Fund left off. These scientists believed that different races experienced diseases differently. The new study would observe the ravages of untreated syphilis in Black populations. They already had the groundwork built. They had a large number of men with untreated syphilis, a nearby hospital at Tuskegee Institute, a bank of goodwill built by Rosenwald, and a store of trust in medical professionals and the U.S. Public Health Service. The scientists successfully exploited all of these. They intentionally coerced and deceived 400 Black Americans into their study. The study had no protocol, patients had no informed consent, and one of the major endpoints was to wait until patients died and then deceive their loved ones into allowing an autopsy. This alone is terrible, but it was – unfortunately – much worse. After the end of World War II, an effective treatment for syphilis became widely available: penicillin. The researchers didn’t provide this to their patients and, in fact, actively thwarted its use in this population. They convinced hospitals, government agencies, and even the U.S. military that the torturous observation of sick and dying people was more important than their health and well-being. This continued for 40 years and only ended in 1972 after the experiment started getting public attention and press. The Tuskegee study ended almost a decade after the Declaration of Helsinki and prompted the passage of the National Research Act and the creation of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. A group of 11 people spent four years developing the Belmont Report. Whereas the Declaration of Helsinki outlines ethical standards to follow, the Belmont Report gives specific guidelines and actionable procedures for determining the legitimacy of research involving human participants. It was initially incorporated into federal law in 1981 as the Protection of Human Subjects. The Belmont Report first outlines the difference between medical practice and research. The goal of practice is normal therapy with a reasonable chance of success, while the goal of research is to test a hypothesis and answer a question. Whereas practice follows the needs of the patient, research follows well-defined, written protocols. The Belmont Report maintains the same three ethical principles in the Declaration of Helsinki – Respect for Persons, Beneficence, and Justice. It then outlines the practical, actionable processes: Informed Consent, Risk/Benefit Assessment, and Subject Selection. Respect for Persons is the idea that most people can make their own choices, and those that can’t must be afforded special protection. These protections must be assessed by third parties, protect participants from harm, and be periodically reevaluated. The Belmont Report applies respect for persons as Informed Consent. Informed consent requires that before a study begins, all information, including the procedure, risks, etc. be clearly written and organized. It requires comprehension by all potential human participants of the above information. Patients cannot be enrolled if they do not understand the informed consent, and the information can’t be written in tiny print and put off to the side like a used car ad. This also means that vulnerable populations (those with limited comprehension, like children) must have extra protection, and third parties (like parents) must help determine comprehension. Finally, informed consent is only given if it is voluntary. This means no large sums of money, threats, or exaggerated promises can be used to coerce people into studies. This can make it more difficult to enroll patients but is critical to avoiding disasters like the Tuskegee syphilis study. Beneficence is the obligation to secure the well-being of patients and to do no harm. Researchers may not injure some people to help others. This is applied as Risk/Benefit Analysis. Under this concept, all benefits must be weighed against potential risks. Risks are a possibility of harm, and include the chance harm will occur and the severity of the harm. This may include things like pain from the site of an injection and must be clearly laid out in the informed consent. Risk/Benefit Analysis is done by researchers, but is overseen and double-checked by Institutional Review Boards (IRBs) – third party boards that oversee studies involving human participants. The Belmont Report lays out specific ways these IRBs assess the risks of a study. These are then weighed against benefits. Benefits are a positive change in health or welfare and are usually much clearer – the alleviation of symptoms from being in a medical study, for instance. Justice is an equal distribution of burdens and benefits across society. Further, justice demands that the groups that participate in research should be the ones that receive the benefits. The racially biased attitudes that formed the basis of the Tuskegee study are the prime example of a failure of justice. These groups were denied benefits, and researchers demanded they take the burdens. The Belmont Report applies justice by way of Selection of Subjects. On the individual level this means that all subjects get fair treatment: you can’t give UF fans all of the investigational medication and FSU fans all placebo, for instance. Societally, the selection of subjects should be done in ways that minimize risks, like choosing adults before children. Selection should be done as fairly as possible and should target the populations that will benefit from research. Unfortunately, the Tuskegee study has undermined trust in government and research in some communities for the past 80 years. From this historical tragedy have arisen solid, unambiguous rules for conducting human research. These ensure safety, oversight, and mitigation of risk so participating in clinical research is beneficial for the community. With the Belmont Report, communities can get access to new medications, find relief from symptoms, and help define their legacy to find possible cures for future generations. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: National Commission for the Protection of Human Subject of Biomedical and Behavior Research. (1977). U.S. Department of Health and Human Services. https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/read-the-belmont-report/index.html Baker, S. M., Brawley, O. W., & Marks, L. S. (2005). Effects of untreated syphilis in the negro male, 1932 to 1972: a closure comes to the Tuskegee study, 2004. Urology, 65(6), 1259-1262. https://doi.org/10.1016/j.urology.2004.10.023 Brandt, A. M. (1978). Racism and research: the case of the Tuskegee Syphilis Study. Hastings center report, 21-29. https://doi.org/10.2307/3561468 Gray, F. D. (1998). The Tuskegee syphilis study: The real story and beyond. NewSouth Books.
Listen to the article here:
In 1945-1946, after the conclusion of the Second World War, several Nazi German leaders and doctors stood trial for crimes against humanity, war crimes, and other atrocious crimes. One of the trials, the so-called Doctor’s Trial (U.S.A. v. Karl Brandt et al.), helped shape how we view and perform clinical research today. One of the major defenses in the Doctor’s Trial was a lack of international law or agreement against the horrible activities the Nazis were doing. To remedy this, the trial ruling (in which seven defendants were sentenced to death) gave an outline of “Permissible Medical Experiments.” This was called the Nuremberg Code and was later expanded by the World Medical Association into the Declaration of Helsinki. The Declaration of Helsinki, originally released in 1964, is the cornerstone of modern clinical research. The medical atrocities during the Holocaust showed that the unsaid rules of medicine needed to be said, printed, and widely distributed. The World Medical Association’s original Declaration of Helsinki has been revised seven times and has since grown by 300%. It concerns the ethical treatment of human participants in medical research. The foundational notions of the Declaration of Helsinki rest on the following two ideas: “The health of my patient will be my first consideration” and “A physician shall act in the patient’s best interest when providing medical care.” The fact that these were up for debate is wild to me, but thanks to the Declaration of Helsinki these are now universal statements. The rest of the Declaration of Helsinki has similar “this should be obvious” content but has been critical for ensuring the safe and ethical treatment of people in research. The document first states that human medicine must be tried in humans at some point. There are also stipulations about what must happen before a study can begin. A protocol must be written that outlines the entire study. An independent review board (IRB) must approve the protocol and any changes. Funding and results should be transparent and public. The document also outlines in broad terms how to do this with respect, beneficence, and justice. Respect comes from the assertion that individual people matter more than new knowledge. This is how we get concepts like informed consent – that all trial participants must have full knowledge of what they are getting into before signing up. Respect also states that patients must voluntarily sign up and be able to discontinue at any time. Further, special protections must be in place for vulnerable populations – like children, prisoners, and people with mentally disabilities. Beneficence is the concept of weighing benefits against risks. In medical research, the benefits must always outweigh the risks. Benefits must help the individual person, a population, or society. Risks must be minimized wherever possible. This is one reason you often see a long list of things that can exclude a person (like being pregnant) from a study: to minimize risks. Beneficence also mandates that studies must be stopped if the risks become too high – if an unintended side effect emerges, for instance. Justice is the concept that research should be for the benefit of everyone. Medications that would target a specific population should be researched in that population. If left-handed people made up 90% of smokers, for instance, then smoking cessation studies should aim to enroll mostly left-handed people. Justice also means groups should be fairly selected and that studies should help people who live where the studies take place. You shouldn’t test a pants-lengthening drug on people in Bermuda (for their Bermuda shorts) and refuse to sell it to them. Altogether, these seem like common-sense rules to have in place, but they need to be written. The Nazis claimed the ends justify the means – even though their end goals were abhorrent. In this world, however, there are no ends – only means. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Bošnjak, S. (2001). The declaration of Helsinki: The cornerstone of research ethics. Archive of Oncology, 9(3), 179-184. Nuremberg Trials Project (n.d.). NMT case 1. Harvard Law School. https://nuremberg.law.harvard.edu/nmt_1_intro Shrestha, B., & Dunn, L. (2019). The Declaration of Helsinki on medical research involving human subjects: a review of seventh revision. https://elibrary.nhrc.gov.np/handle/20.500.14356/1367 Taylor, T. (1955). Nuremberg Trials, The. Colum. L. Rev., 55, 488. https://www.jstor.org/stable/1119814?read-now=1&seq=38 United States Holocaust Memorial Museum, Washington, DC. (n.d.). The Nuremberg code. Holocaust Encyclopedia. Accessed 5/13/2024. https://encyclopedia.ushmm.org/content/en/article/the-nuremberg-code World Medical Association. (2013). World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Jama, 310(20), 2191-2194. https://jamanetwork.com/journals/jama/fullarticle/1760318/
Listen to the article here:
Diabetes is a widespread disease where the body cannot process sugars effectively. It has myriad effects on the body, including in the gut. Diabetes affects nearly every part of the gastrointestinal tract, from the throat to the anus. Diabetes is one of the most common causes of a condition called gastroparesis. Gastroparesis is from the Greek language. Gastro- means “stomach,” –paresis indicates a partial paralysis, so gastroparesis means a partial paralysis of the stomach; it empties food slowly. This condition is more likely to affect women than men, but there aren’t good numbers on how many people it affects in total. Symptoms of diabetes and gastroparesis may overlap but include feeling full, weight changes, nausea, vomiting, bloating, and diarrhea. Gastroparesis can lead to serious complications like malnutrition, decreased quality of life – including anxiety and depression, and significantly higher mortality. The effects of diabetes further exacerbate these complications. How diabetes actually affects stomach muscles is complex and fascinating. The digestive tract is lined with smooth muscle. Smooth muscle isn’t connected to bone and contracts in long, slow, low-energy waves. This is great for contracting blood vessels or moving food through the stomach and intestines. These are involuntary muscles, meaning we can’t consciously control them. In fact, the brain modulates the activity of gastrointestinal muscle, but it’s controlled by our “little brain” in the intestines! This little brain is made of around 500 million neurons and is called the enteric nervous system. The enteric nervous system is a distributed brain-like bunch of neurons and other cells spread throughout our abdomen that may be able to act independently of our big brain. It is responsible for getting the smooth muscle to contract rhythmically and in response to food. The enteric nervous system also includes cells that aren’t neurons. An important type is interstitial cells of Cajal (kuh-jaal). These are pacemaker cells that regularly generate electrical signals to coordinate muscle. The prominent players in the enteric nervous system, however, are neurons. Though neurons are electric, they communicate with other neurons by releasing neurotransmitters and receiving them in specialized receptors. These are often the same neurotransmitters we find in the brain, though they may have different functions. Dopamine is a great example. In the brain, dopamine receptors are part of the reward pathway, giving you feelings of pleasure and motivation. In the enteric nervous system, dopamine receptors act to suppress muscle movement. More dopamine in the brain makes you feel happy, but more dopamine in the gut restricts the movement of food. In diabetes, this can get all messed up. A key aspect of uncontrolled diabetes is the inability of the body to regulate blood sugar. This causes a few significant disturbances. Primary among these is neuron damage. Since the affected neurons are involuntary, we call this autonomic neuropathy. Autonomic neuropathy in the gastrointestinal tract can take the form of fewer neurons and ones that can’t communicate well because of damage. Diabetes can also lead to changes in the signaling pathways of smooth muscle and may destroy some of the pacemaking interstitial cells of Cajal. Together, these changes result in fewer smooth muscle contractions and a slower flow of food through the stomach and intestinal tract. The slow flow of food in gastroparesis can cause a feedback loop. Slow food is more likely to be mistaken for invaders, potentially causing inflammation. Even worse, the extra time in the digestive tract means there is more time for glucose, a major sugar, to get absorbed – increasing blood sugar and making the symptoms of diabetes worse. So, what can be done with diabetic gastroparesis? The first step is lifestyle alteration. Smaller and more frequent meals may help alleviate symptoms. Increasing noncarbonated liquids and decreasing fat and fiber may also help. Monitoring nutrient levels and electrolytes is critical. Beyond this, few medications are currently available. The most prominent are dopamine D2 receptor antagonists; meaning they inhibit the effect of dopamine. Metoclopramide (meh-tow-klow-pruh-mide) inhibits dopamine and mimics serotonin. It is effective at increasing the speed of emptying. It can cross the blood-brain barrier, however, causing unintended side effects in the brain. Domperidone (daam-peh-ruh-down) is another dopamine receptor antagonist. It doesn’t cross into the brain but can affect the heart, slowing the time it takes to recharge between beats. This medication is not approved in the United States, though it’s been approved in several other countries for decades. Clinical research is currently looking into new medications that may provide the same dopamine receptor inhibition as metoclopramide and domperidone but without the ability to affect the brain or heart! With the help of clinical volunteers, diabetic gastroparesis may pass quicker than we expected! At the time of writing this article, clinical research for diabetic gastroparesis is enrolling at our Nature Coast Clinical Research – Inverness office. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Aswath, G. S., Foris, L. A., Ashwath, A. K., & Patel, K. (2017). Diabetic Gastroparesis. https://www.ncbi.nlm.nih.gov/books/NBK430794/ Bharucha, A. E., Kudva, Y. C., & Prichard, D. O. (2019). Diabetic gastroparesis. Endocrine reviews, 40(5), 1318-1352. https://academic.oup.com/edrv/article/40/5/1318/5487986?login=true Isola, S., Hussain, A., Dua, A., Singh, K., & Adams, N. (2018). Metoclopramide. https://www.ncbi.nlm.nih.gov/books/NBK519517/ Puoti, M. G., Assa, A., Benninga, M., Broekaert, I. J., Carpi, F. J. M., Saccomani, M. D., … & Borrelli, O. (2023). Drugs in focus: Domperidone. Journal of pediatric gastroenterology and nutrition, 77(2), e13-e22. DOI: 10.1097/MPG.0000000000003822 Sanders, K. M., Koh, S. D., Ro, S., & Ward, S. M. (2012). Regulation of gastrointestinal motility—insights from smooth muscle biology. Nature reviews Gastroenterology & hepatology, 9(11), 633-645. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4793911/ Sugumar, A., Singh, A., & Pasricha, P. J. (2008). A systematic review of the efficacy of domperidone for the treatment of diabetic gastroparesis. Clinical gastroenterology and hepatology, 6(7), 726-733. https://www.cghjournal.org/article/S1542-3565(08)00241-3/fulltext Tonini, M., Cipollina, L., Poluzzi, E., Crema, F., Corazza, G. R., & De Ponti, F. (2004). Clinical implications of enteric and central D2 receptor blockade by antidopaminergic gastrointestinal prokinetics. Alimentary pharmacology & therapeutics, 19(4), 379-390. doi: 10.1111/j.1365-2036.2004.01867.x Uranga-Ocio, J. A., Bastús-Díez, S., Delkáder-Palacios, D., García-Cristóbal, N., Leal-García, M. Á., & Abalo, R. (2015). Enteric neuropathy associated to diabetes mellitus. https://digital.csic.es/handle/10261/241840 Yarandi, S. S., & Srinivasan, S. (2014). Diabetic gastrointestinal motility disorders and the role of enteric nervous system: current status and future directions. Neurogastroenterology & Motility, 26(5), 611-624. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4104990/
Listen to the article here:
Breathing has been described by top scientists as “important” for some reason. Unfortunately, some of us have trouble breathing at night, which is… less than ideal. Obstructive sleep apnea (OSA) is a condition where the airway is periodically blocked while sleeping, leading to sleep disruptions. The word apnea comes from the Greek language. The prefix a– means “not” and –pnea comes from the word for breath, the same root as the word “pneumatic.” OSA is very common, with around one billion people suffering from the condition worldwide. Most people are unaware they have OSA because the breathing interruptions occur when sleeping. Regardless, OSA can cause people to snore, wake up at night, and have sleep that isn’t restful. This can lead to complications with cardiovascular and mental health, quality of life, and excessive sleepiness – which makes driving more dangerous. So how does breathing work, why does the airway get blocked with obstructive sleep apnea, and is there anything we can do about it? Breathing is actually a pretty complex operation. Normally, breathing out is mostly an act of relaxing, but breathing in is a highly coordinated effort. Muscles in the diaphragm and chest contract to open the lungs and create a vacuum. The upper airway consists of the respiratory tract from the nose to above the vocal cords. This unique part of the body processes both food and air, requiring elasticity and flexibility to accomplish these competing tasks. It also produces speech sounds, chewing, sneezing, etc. The muscles that coordinate these tasks need to be contracted when breathing in for the airway to remain open. In OSA, the upper airway gets blocked. When we lie down the fluid that pools in our legs flows up to the rest of the body, causing it to swell. When we sleep, the brain may not keep the throat muscles firm, causing a partial collapse of the throat. This is exacerbated when lying on the back, as the tongue and jaw fall into the airway. Alone, none of these would cause OSA. A partial blocking of the airway frequently results in snoring as bits of the throat flap in the breeze. OSA occurs when the changes we experience during sleep accompany structural damage to the upper airway. This damage can take many forms: a jaw that is small or set back in the throat, enlarged adenoid glands, and shifting bone structure. Additionally, increased adipose (fat) tissue in the neck can narrow the airway. Other risks include being male, obese, older, pregnant, and sleeping on the back. Some substances can increase the risk of OSA, including alcohol, cigarettes, sedatives, and hypnotics like benzodiazepines. These risk factors cause the throat to narrow or the brain to relax the jaw (or both) which causes the airway to temporarily collapse. Instead of pulling air into the lungs, the vacuum pulls the throat together. The body doesn’t get enough oxygen, and trouble increases from there. So what can be done? A lot, actually! The first step is a diagnostic test. A nighttime in-laboratory sleep test called polysomnography is the go-to test, but home and portable sleep tests exist as well. Guidelines and directions must be carefully followed on portable kits to ensure accurate findings. If you do have OSA, the remedies vary widely. First, it’s a good idea to abstain from things that exacerbate OSA; like drinking and smoking. Second, sleeping on the side may provide some relief in mild cases. Beyond this, medical professionals may look into treating related disorders like asthma and heart failure. A sleep specialist may recommend or prescribe a Continuous Positive Airway Pressure (CPAP) machine, which pushes air into the throat instead of relying on the lungs to pull it in. These are highly effective but have low adherence, with around 50% of patients using the machines for less than 3 hours a night after the first month. In more severe cases, a specialist may recommend an oral appliance and/or surgery to physically change the structure of the airway. For many people, the solution to OSA may be to expand the airway by losing weight. This can be easier said than done, and clinical trials are looking into the effects of medications that induce weight loss for their ability to also tackle OSA. With luck, these new routes of treatment will let those with OSA breathe a little easier at night. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Choudhury, N., & Deshmukh, P. (2023). Obstructive Sleep Apnea in Adults and Ear, Nose, and Throat (ENT) Health: A Narrative Review. Cureus, 15(10). doi.org/10.7759/cureus.47637 Del Negro, C. A., Funk, G. D., & Feldman, J. L. (2018). Breathing matters. Nature Reviews Neuroscience, 19(6), 351-367. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6636643/ Eckert, D. J., & Malhotra, A. (2008). Pathophysiology of adult obstructive sleep apnea. Proceedings of the American thoracic society, 5(2), 144-153. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2628457/ Otis, A. B., Fenn, W. O., & Rahn, H. (1950). Mechanics of breathing in man. Journal of applied physiology, 2(11), 592-607. Downloaded from journals.physiology.org/journal/jappl (073.035.112.088) on April 30, 2024 Sankri-Tarbichi, A. G. (2012). Obstructive sleep apnea-hypopnea syndrome: Etiology and diagnosis. Avicenna Journal of Medicine, 2(01), 3-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3507069/ Slowik, J. M., Sankari, A., & Collen, J. F. (2022). Obstructive sleep apnea. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459252/
Listen to the article here:
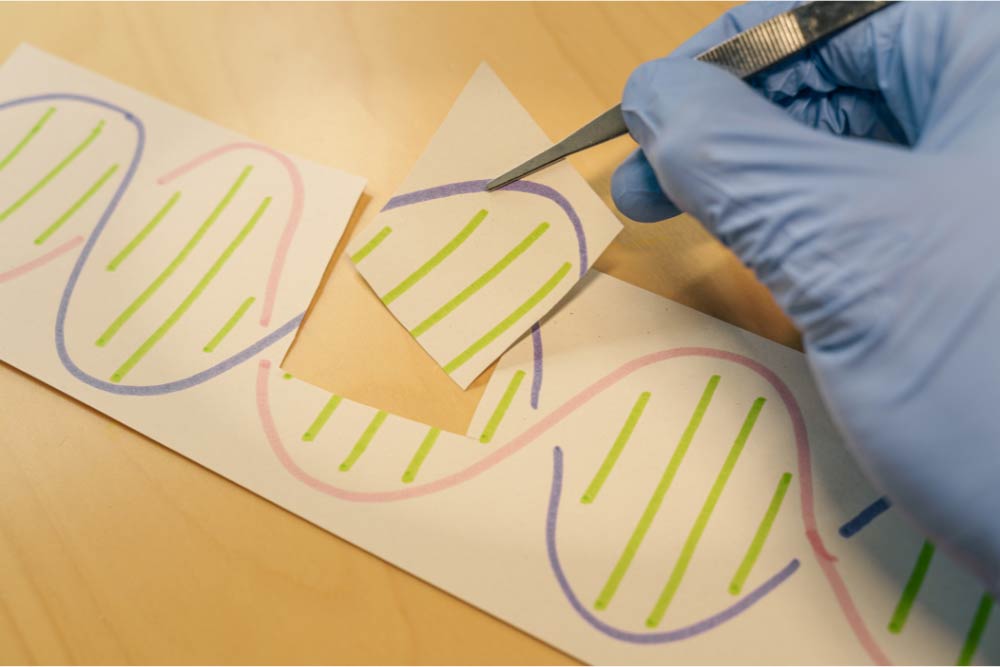
When we think of an animal, we generally think of a single creature with a unique DNA code. A human starts as a single fertilized egg cell with the combined genetic code from our parents. By the time we’re walking and talking, however, we’ve already transformed into a superorganism. If you were to count the number of cells that make you up, only half would be human. Mature red blood cells lack a nucleus, so if we count only cells with nuclei, we’re only about 10% human. Going further, if we count all the genetic material in our body, only about 1% of it is human. Genetically, we’re 99% nonhuman. So then, what are we? Bacteria. We’re primarily bacteria. These bacteria live with us our whole lives. They live on our skin, in our hair, on our eyelashes, and in our gut. The bacteria that live in the digestive tract, along with the relatively minuscule amounts of viruses, archaea, and yeasts, make up the gut microbiome. The gut microbiome is incredible. It establishes itself until around age two. It changes in response to the food we eat, diseases we get, medications we take (especially antibiotics), and our hygiene. We eat around 60 tons of food in our lives, and the gut microbiome has a hand in all of it. We usually think of bacteria (and viruses, etc) as parasitic (doing damage). The reality is the gut microbiome is truly symbiotic, we need it as much as it needs us. The gut microbiome performs many tasks for us. It shapes the human cells and the mucus that lines our gut, strengthening it. It protects us from infections, keeps our cells together in a tight barrier, and communicates with the immune system. Microbiome cells outcompete other, destructive bacteria. They can also release bacteriocins (bacteria-targeting toxins) that destroy dangerous bacteria. The microbiome is so stellar it helps us even when it’s just eating. The gut microbiome breaks down foods we can’t process, like dietary fiber. Through the process of fermentation, it uses this food to make vitamins, minerals, etc. As an example: we can’t make vitamin B12 at all in our cells; we rely on microorganisms to make it for us! Finally, the gut microbiome makes short-chain fatty acids. Short-chain fatty acids are the primary energy source for the human cells that line the intestine. They also increase insulin sensitivity and mediate immune regulation, inflammation, and other body processes. Unfortunately, the gut microbiome can get out of whack, and issues like ulcerative colitis – an inflammatory bowel disease – can occur. To understand what can go wrong, let’s first investigate a healthy gut microbiome. The colony of colon bacteria is unique in everyone. A healthy microbiome has three qualities: high diversity, high richness, and high stability. Diversity is just what it sounds like: the total number of different species present. Richness is the balance between species; having roughly equivalent numbers of bacteria from each. Stability is the consistency of finding the same types and numbers of organisms over time. So what does a disruption in the balance of the gut microbiome look like? Loss of diversity, overgrowth of some types of organisms, and changes to the composition of the gut microbiome over time. The degradation of diversity, richness, or stability is called dysbiosis. One cause of dysbiosis is antibiotics. They are designed to kill bacteria, which is bad news for the gut bacteria. Antibiotics frequently lead to a redistribution of gut microbiota. Other things that can cause dysbiosis include hygiene, infection, and smoking. The most important, however, is diet. All of the food we eat travels through the gut. In the western world, our diets aren’t always built to cultivate a healthy gut microbiome. Much of our food is built for shelf stability and is made using enzymes or chemicals instead of bacteria. We tend to eat more animal fats and proteins and fewer plant fibers than indigenous populations. To top this off, we eat refined sugar. Like, a LOT of refined sugar. Around 50 to 100 pounds of refined sugar per year. I’m not a nutrition expert, but I am a cookie expert, and that’s way too many cookies. When the microbiome is in a state of dysbiosis, it can’t perform its helpful functions. The mucus layer is reduced, bacteria can’t interact with the immune and inflammation systems, and the gut is more permeable to undesirable substances. On top of this, short-chain fatty acid production decreases, making it more difficult for the human cells lining the gut. This loss of function is linked to diseases like ulcerative colitis. The exact causes of ulcerative colitis are unknown, but scientists think it is related to the gut microbiome. Ulcerative colitis is a chronic inflammatory disease with periods of high and low activity. Inflammation leads to painful ulcers along the colon and rectum. So what can we do when the gut is out of whack? This is still a relatively new area of research, so there are many questions we have to answer. Our best solutions so far are food and feces. The importance of food to the gut microbiome should be obvious by now. Foods high in dietary fibers from plants are needed for gut bacteria to survive and thrive. The role of bacteria derived from human feces is still being developed. Fecal transplantation is a fascinating, but not-for-the-dinner-table line of study. The basic idea is that doctors would transfer some of the gut microbiome from a healthy person to a sick one, perhaps someone with ulcerative colitis. These bacteria would hopefully colonize and outcompete whatever is disrupting the sick microbiome, restoring diversity, richness, and stability. Focusing on the symbiotic relationship we share with our individual microbiome will revolutionize our approach to healthcare. Clinical trials may pave the way forward for treatments that support our human cells and our microbiome, nurturing the microbial communities vital to our survival and well-being as a superorganism. Also, don’t forget to eat your veggies. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Bengmark, S. (1998). Ecological control of the gastrointestinal tract. The role of probiotic flora. Gut, 42(1), 2-7. https://doi.org/10.1136/gut.42.1.2 Fan, Y., & Pedersen, O. (2021). Gut microbiota in human metabolic health and disease. Nature Reviews Microbiology, 19(1), 55-71. https://doi.org/10.1038/s41579-020-0433-9 Gomaa, E. Z. (2020). Human gut microbiota/microbiome in health and diseases: a review. Antonie Van Leeuwenhoek, 113(12), 2019-2040. https://link.springer.com/article/10.1007/s10482-020-01474-7 LeBlanc, J. F., Segal, J. P., de Campos Braz, L. M., & Hart, A. L. (2021). The microbiome as a therapy in pouchitis and ulcerative colitis. Nutrients, 13(6), 1780. https://doi.org/10.3390/nu13061780 Sender, R., Fuchs, S., & Milo, R. (2016). Revised estimates for the number of human and bacteria cells in the body. PLoS biology, 14(8), e1002533. https://doi.org/10.1371/journal.pbio.1002533 Świrkosz, G., Szczygieł, A., Logoń, K., Wrześniewska, M., & Gomułka, K. (2023). The Role of the Microbiome in the Pathogenesis and Treatment of Ulcerative Colitis—A Literature Review. Biomedicines, 11(12), 3144. https://doi.org/10.3390/biomedicines11123144 Tan, J., McKenzie, C., Potamitis, M., Thorburn, A. N., Mackay, C. R., & Macia, L. (2014). The role of short-chain fatty acids in health and disease. Advances in immunology, 121, 91-119. https://doi.org/10.1016/b978-0-12-800100-4.00003-9 The Human Microbiome Project Consortium. (2021). Structure, function and diversity of the healthy human microbiome. Nature 486, 207–214. https://www.nature.com/articles/nature11234 Thursby, E., & Juge, N. (2017). Introduction to the human gut microbiota. Biochemical journal, 474(11), 1823-1836. https://portlandpress.com/biochemj/article/474/11/1823/49429 Xiong, R. G., Zhou, D. D., Wu, S. X., Huang, S. Y., Saimaiti, A., Yang, Z. J., … & Li, H. B. (2022). Health benefits and side effects of short-chain fatty acids. Foods, 11(18), 2863. https://doi.org/10.3390%2Ffoods11182863 Young, V. B., & Schmidt, T. M. (2008). Overview of the gastrointestinal microbiota. Advances in experimental medicine and biology, 635, 29–40. https://doi.org/10.1007/978-0-387-09550-9_3
Listen to the article here:
High blood pressure is amazingly prevalent, affecting nearly half of all Americans. It’s a major risk factor for heart attack, stroke, kidney failure, eye damage, and more. Unfortunately, this condition remains highly prevalent despite the numerous medications designed to treat it. For many patients, adhering to medications can be difficult, and for others, some medicines are not effective in reducing blood pressure levels. But what if there were a way to lower blood pressure at the source, the heart? First, let’s examine how the heart relates to blood pressure. It might seem obvious, but it’s actually quite complex. The heart draws blood in and pushes it out with each beat. The amount of blood pumped is called the stroke volume. A good stroke volume helps to ensure the heart has enough blood pressure to deliver oxygen throughout the body. A healthy heart will pump out around 50-70% of the total volume of blood. This means there remains some unpumped fluid in the heart chambers after pumping is complete. When the next heartbeat comes, the heart muscle has to stretch enough to accommodate this unpumped blood. This extra blood increases our blood pressure because of the Frank-Starling law of the heart. The Frank-Starling law of the heart is over 100 years old and states that the amount our heart muscles stretch before pumping scales with the force they deliver when pumping. Think of a rubber band. If you stretch it a little, it’ll flop back in place. If you stretch a rubber band a lot, almost to its breaking point, it’ll snap back so hard as to leave a welt on your skin. The heart is similar; extra blood in the heart before pumping increases the pressure of each beat and maintains our blood pressure. If there were a way to lower the amount of blood in the chamber after beating, it follows that blood pressure may be lowered. Note that just the pressure would be lowered. The stroke volume would (ideally) remain the same. But how could we do this? For most people, we don’t have any way of convincing the heart to empty more effectively. For a select few, however, the hardware may already be in place. Pacemakers are amazing technology that has helped countless people whose hearts aren’t working properly. Over a million pacemakers are implanted every year worldwide and help people with arrhythmias. Arrhythmias are conditions that involve irregular heartbeat. Pacemakers are surgically implanted devices that send small amounts of electricity where they are needed in the heart. Heart muscles are triggered by this little zap and beat in response to it. Pacemaker rhythms can be customized for several types of conditions, and can even be programmed after being implanted to adapt to changing patient conditions. This is where a pacemaker’s ability to help with high blood pressure is theorized. By customizing how a pacemaker fires, it is possible to cause the heart to release more of its contents and lower the amount of blood remaining in the heart before pumping. According to the Frank-Starling law of the heart, this should result in lower blood pressure (indeed, early clinical trials show this to be the case). Finally, we have to make sure changes to our blood pressure bypass the sympathetic nervous system. This pathway, also called the “fight or flight” pathway, helps ensure the body is awake, alert, and alive. Integral to this system are receptors that sense our blood pressure. If the sympathetic nervous system senses a prolonged drop in blood pressure, it kicks in to correct this. This is a critical system that keeps us from constantly fainting but can be problematic when trying to lower blood pressure. A clever workaround being investigated is to have a pacemaker lower the blood pressure intermittently. It runs the chamber-emptying algorithm for short periods of time. This may help bypass our sympathetic nervous responses. If clinical trials bear out, pacemakers may be able to change not just the pace of the heart, but the pressure too! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Centers for Disease Control and Prevention. (2023). Facts about hypertension. U.S. Department of Health & Human Services. https://www.cdc.gov/bloodpressure/facts.htm Mond, H. G., & Proclemer, A. (2011). The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009–a World Society of Arrhythmia’s project. Pacing and clinical electrophysiology : PACE, 34(8), 1013–1027. https://doi.org/10.1111/j.1540-8159.2011.03150.x Kalarus, Z., Merkely, B., Neužil, P., Grabowski, M., Mitkowski, P., Marinskis, G., … & Kuck, K. H. (2021). Pacemaker‐Based Cardiac Neuromodulation Therapy in Patients With Hypertension: A Pilot Study. Journal of the American Heart Association, 10(16), e020492. https://www.ahajournals.org/doi/full/10.1161/JAHA.120.020492 Mitchell, L.B. (2023). Cardiac pacemakers. Merck Manual, Professional Version. https://www.merckmanuals.com/professional/cardiovascular-disorders/overview-of-arrhythmias-and-conduction-disorders/cardiac-pacemakers Neuzil, P., Merkely, B., Erglis, A., Marinskis, G., de Groot, J. R., Schmidinger, H., … & Kuck, K. H. (2017). Pacemaker‐mediated programmable hypertension control therapy. Journal of the American Heart Association, 6(12), e006974. https://www.ahajournals.org/doi/full/10.1161/JAHA.117.006974 Sequeira, V., & van der Velden, J. (2015). Historical perspective on heart function: the Frank–Starling Law. Biophysical reviews, 7, 421-447. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5418489
Listen to the article here:
It’s spring, which means lots of sneezing, sweets, and sunlight! Of those three, sunlight is probably the healthiest, so let’s shine a light on what sunlight does in the body and why we need it. First, the sun is vital for keeping the planet habitable. Without the sun, we would all die very fast as oxygen would solidify on the surface, and we’d be unable to breathe. Beyond being vital to life, sunlight is used by the skin to produce Vitamin D! Vitamin D is actually a collection of very similar molecules called calciferols. These are fat-soluble steroid hormones that are used throughout the body. Vitamin D deficiency is a worldwide problem, and affects at least ⅓ of Americans. It is linked to complications in bones, kidneys, heart, and brain, as well as to diabetes, immune system issues, obesity, and poor pregnancy outcomes. Though indications of this deficiency seem robust, the solutions are anything but. Unfortunately, the effects of supplemental vitamin D, and therefore sunlight, are grossly understudied. Trial after trial after trial (check the extensive references list) shows that supplemental vitamin D – and in some cases supplemental light – does not have a significant effect on measurable outcomes for patients. These trials consistently find that the levels of circulating vitamin D in the bloodstream are increased, but symptoms are unaffected. The only results I could find from randomized, placebo-controlled clinical trials showing actual benefits to patients were for those with sickle-cell disease and in reducing respiratory infections in elderly patients. This is counter to “common knowledge” and to the assumed knowledge found in several research papers. Observational studies, where scientists look at populations, find a myriad of problems associated with vitamin D and sunlight deficiency. Let’s try to illuminate why clinical trials haven’t found benefits when giving supplemental vitamin D. The answer is likely that the problems that cause vitamin D deficiency aren’t solved by supplementation! Vitamin D production starts in the skin, then goes to the liver and kidneys before the body can use it. The symptoms associated with low levels of vitamin D may not improve if there are underlying liver or kidney issues, though those conditions can hinder the production of Vitamin D. Further, observational studies look at a population and investigate the correlations between items. This can tell us things that may be associated with each other but does not indicate that one thing is causing the other. An example would be looking at the availability of toilet paper and used car prices over the last 10 years. In 2020 toilet paper was unavailable and used car prices soared! This wasn’t because we needed toilet paper to run our used cars or anything; there was a pandemic disrupting supply chains! In the case of vitamin D deficiency, the lack of vitamin D is probably the effect of not going outside! If a mental disorder like depression keeps people indoors, this would lower the vitamin D they produce, not the other way around. On top of this, it is very difficult for scientists to isolate sunlight (and therefore vitamin D) from exercise. People who stay inside and never see the sun are, on average, less active. This can lead to some of the problems we associate with vitamin D deficiency, including bone issues, obesity, diabetes, and heart problems. In these cases vitamin D deficiency is more a canary in the coal mine than the smoke of a fire. So, what can we take away from this? First and most importantly is that in all of these clinical trials supplemental vitamin D has been found to be safe. If vitamin D helps you with an issue, there is nothing wrong with continuing your care. Always consult with your doctor before making changes to your medication. Second, clinical trials are vital to our medical system! Observational studies are no substitute for actual experimentation in a placebo-controlled, randomized trial. The common knowledge is that sunlight and vitamin D are good for us. This is true, but it’s best to start at the source, the sun (if you can), rather than supplementing after the fact. We should spend more time outside in the nice weather, but remember your sunscreen. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Aranow, C., Kamen, D. L., Dall’Era, M., Massarotti, E. M., Mackay, M. C., Koumpouras, F., … & Diamond, B. (2015). Randomized, double‐blind, placebo‐controlled trial of the effect of vitamin D3 on the interferon signature in patients with systemic lupus erythematosus. Arthritis & rheumatology, 67(7), 1848-1857. https://doi.org/10.1002/art.39108 Burns, A. C., Saxena, R., Vetter, C., Phillips, A. J., Lane, J. M., & Cain, S. W. (2021). Time spent in outdoor light is associated with mood, sleep, and circadian rhythm-related outcomes: a cross-sectional and longitudinal study in over 400,000 UK Biobank participants. Journal of affective disorders, 295, 347-352. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8892387/ Eckard, A. R., O’Riordan, M. A., Rosebush, J. C., Lee, S. T., Habib, J. G., Ruff, J. H., … & McComsey, G. A. (2018). Vitamin D supplementation decreases immune activation and exhaustion in HIV-1-infected youth. Antiviral therapy, 23(4), 315-324. https://doi.org/10.3851/imp3199 Guralnik, J. M., Sternberg, A. L., Mitchell, C. M., Blackford, A. L., Schrack, J., Wanigatunga, A. A., … & STURDY Collaborative Research Group. (2022). Effects of vitamin D on physical function: results from the STURDY trial. The Journals of Gerontology: Series A, 77(8), 1585-1592. https://doi.org/10.1093/gerona/glab379 Ginde, A. A., Blatchford, P., Breese, K., Zarrabi, L., Linnebur, S. A., Wallace, J. I., & Schwartz, R. S. (2017). High‐dose monthly vitamin D for prevention of acute respiratory infection in older long‐term care residents: a randomized clinical trial. Journal of the American Geriatrics Society, 65(3), 496-503. https://pubmed.ncbi.nlm.nih.gov/27861708/ Hansen, K. E., Johnson, R. E., Chambers, K. R., Johnson, M. G., Lemon, C. C., Vo, T. N., & Marvdashti, S. (2015). Treatment of Vitamin D Insufficiency in Postmenopausal Women: A Randomized Clinical Trial. JAMA internal medicine, 175(10), 1612–1621. https://doi.org/10.1001/jamainternmed.2015.3874 Huiberts, L. M., & Smolders, K. C. (2021). Effects of vitamin D on mood and sleep in the healthy population: Interpretations from the serotonergic pathway. Sleep Medicine Reviews, 55, 101379. https://www.sciencedirect.com/science/article/pii/S1087079220301222 Javed, A., Kullo, I. J., Balagopal, P. B., & Kumar, S. (2016). Effect of vitamin D3 treatment on endothelial function in obese adolescents. Pediatric obesity, 11(4), 279-284. https://onlinelibrary.wiley.com/doi/10.1111/ijpo.12059 Juraschek, S. P., Miller III, E. R., Wanigatunga, A. A., Schrack, J. A., Michos, E. D., Mitchell, C. M., … & Appel, L. J. (2022). Effects of vitamin D supplementation on orthostatic hypotension: results from the STURDY trial. American journal of hypertension, 35(2), 192-199. https://doi.org/10.1093/ajh/hpab147 Karsy, M., Guan, J., Eli, I., Brock, A. A., Menacho, S. T., & Park, M. S. (2019). The effect of supplementation of vitamin D in neurocritical care patients: RandomizEd Clinical TrIal oF hYpovitaminosis D (RECTIFY). Journal of neurosurgery, 1–10. Advance online publication. https://doi.org/10.3171/2018.11.JNS182713 Michos, E. D., Kalyani, R. R., Blackford, A. L., Sternberg, A. L., Mitchell, C. M., Juraschek, S. P., … & Appel, L. J. (2022). The relationship of falls with achieved 25-Hydroxyvitamin D levels from vitamin D supplementation: the STURDY trial. Journal of the Endocrine Society, 6(6), bvac065. https://doi.org/10.1210/jendso/bvac065 Okereke, O. I., Reynolds, C. F., Mischoulon, D., Chang, G., Vyas, C. M., Cook, N. R., … & Manson, J. E. (2020). Effect of long-term vitamin D3 supplementation vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. Jama, 324(5), 471-480. https://jamanetwork.com/journals/jama/fullarticle/2768978 Osunkwo, I., Ziegler, T. R., Alvarez, J., McCracken, C., Cherry, K., Osunkwo, C. E., … & Tangpricha, V. (2012). High dose vitamin D therapy for chronic pain in children and adolescents with sickle cell disease: results of a randomized double blind pilot study. British journal of haematology, 159(2), 211-215. https://onlinelibrary.wiley.com/doi/abs/10.1111/bjh.12019 Øverland, S., Woicik, W., Sikora, L., Whittaker, K., Heli, H., Skjelkvåle, F. S., … & Colman, I. (2020). Seasonality and symptoms of depression: A systematic review of the literature. Epidemiology and psychiatric sciences, 29, e31. https://www.cambridge.org/core/journals/epidemiology-and-psychiatric-sciences/article/seasonality-and-symptoms-of-depression-a-systematic-review-of-the-literature/375F49B0149E903EFBDEDF9D53431B15 Palacios, C., & Gonzalez, L. (2014). Is vitamin D deficiency a major global public health problem?. The Journal of steroid biochemistry and molecular biology, 144, 138-145. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4018438/ Ponda, M. P., Liang, Y., Kim, J., Hutt, R., Dowd, K., Gilleaudeau, P., Sullivan-Whalen, M. M., Rodrick, T., Kim, D. J., Barash, I., Lowes, M. A., & Breslow, J. L. (2017). A randomized clinical trial in vitamin D-deficient adults comparing replenishment with oral vitamin D3 with narrow-band UV type B light: effects on cholesterol and the transcriptional profiles of skin and blood. The American journal of clinical nutrition, 105(5), 1230–1238. https://doi.org/10.3945/ajcn.116.150367 Rorie, A., Goldner, W. S., Lyden, E., & Poole, J. A. (2014). Beneficial role for supplemental vitamin D3 treatment in chronic urticaria: áaárandomized study. Annals of allergy, asthma & immunology, 112(4), 376-382. https://www.annallergy.org/article/S1081-1206(14)00012-X/abstract Sadock, B.J., Sadock, V.A., & Ruiz, P. (2017). Comprehensive textbook of psychiatry (Vol. 1/2). Sadock, B.J., Sadock, V.A., & Ruiz, P. (Eds.). Philadelphia: Lippincott Williams & Wilkins. Sokol, S. I., Srinivas, V., Crandall, J. P., Kim, M., Tellides, G., Lebastchi, A., … & Alderman, M. H. (2012). The effects of vitamin D repletion on endothelial function and inflammation in patients with coronary artery disease. Vascular medicine, 17(6), 394-404. https://journals.sagepub.com/doi/10.1177/1358863X12466709 Shaffer, J. A., Edmondson, D., Wasson, L. T., Falzon, L., Homma, K., Ezeokoli, N., … & Davidson, K. W. (2014). Vitamin D supplementation for depressive symptoms: a systematic review and meta-analysis of randomized controlled trials. Psychosomatic medicine, 76(3), 190-196. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4008710/ Simha, V., Mahmood, M., Ansari, M., Spellman, C. W., & Shah, P. (2012). Effect of vitamin D replacement on insulin sensitivity in subjects with vitamin D deficiency. Journal of investigative medicine, 60(8), 1214-1218. https://doi.org/10.2310/jim.0b013e3182747c06 Sokol, S. I., Srinivas, V., Crandall, J. P., Kim, M., Tellides, G., Lebastchi, A., … & Alderman, M. H. (2012). The effects of vitamin D repletion on endothelial function and inflammation in patients with coronary artery disease. Vascular medicine, 17(6), 394-404. https://doi.org/10.1177/1358863×12466709 Wei, W., Shary, J. R., Garrett-Mayer, E., Anderson, B., Forestieri, N. E., Hollis, B. W., & Wagner, C. L. (2017). Bone mineral density during pregnancy in women participating in a randomized controlled trial of vitamin D supplementation. The American Journal of Clinical Nutrition, 106(6), 1422-1430. https://doi.org/10.3945/ajcn.116.140459 Winthorst, W. H., Bos, E. H., Roest, A. M., & de Jonge, P. (2020). Seasonality of mood and affect in a large general population sample. Plos one, 15(9), e0239033. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0239033 Wirz-Justice, A., Skene, D. J., & Münch, M. (2021). The relevance of daylight for humans. Biochemical pharmacology, 191, 114304. https://www.sciencedirect.com/science/article/pii/S0006295220305402 Zahoor, I., & Haq, E. (2017). Vitamin D and multiple sclerosis: An update. Exon Publications, 71-84. https://www.ncbi.nlm.nih.gov/books/NBK470154/
Listen to the article here:
The body is as amazing as it is complex. Consider the thyroid, this tiny gland sits in your neck, just under the Adam’s apple (larynx), and is butterfly-shaped (technically, thyroid comes from the Greek word for an oblong shield, but it’s butterfly season, and I haven’t used a Greek shield in a hot minute.) It’s unassuming, easy to miss, and affects nearly every cell in the body. The thyroid is part of the endocrine system, which is responsible for producing and releasing hormones that regulate countless bodily functions. The endocrine system is a messenger system of interwebbed feedback loops that regulate how the body metabolizes food products into energy, cellular materials, and waste. Disruptions in this system can have enormous downstream effects, as with the thyroid.
The thyroid is part of the hypothalamus-pituitary-thyroid axis. The hypothalamus is in the brain. When it senses low levels of thyroid hormones, it tells the pituitary gland (at the base of the brain) to release Thyroid-stimulating hormone (TSH). This, predictably, stimulates the thyroid to produce more hormones. Doctors monitor TSH levels when checking on thyroid function. TSH activates the thyroid, which produces Thyroxine (tetraiodothyronine, or T4) and Triiodothyronine (T3). These names are long and complicated, but the presence of “iodo” in the middle provides a clue that iodine is a key part of these chemicals. Stay tuned for more on that later. The thyroid also produces calcitonin, which can regulate calcium levels. T4 and T3 are the hormones monitored by the hypothalamus: if it detects enough in the blood, it tells the pituitary gland to lower TSH production. Together, measuring the levels of TSH, T4, and T3 can give a good idea of how the thyroid is performing. Surprisingly, the thyroid produces only about 20% of the body’s T3, the majority is derived from T4 which has been delivered to body tissue! You can think of T4 as a long-lasting store of T3, though it also has some effect on specific cells. T3 is a big deal, it has metabolic effects on basically all cells and promotes protein production. Strangely, 99% of all T3 and T4 are bound in proteins and unable to activate cell receptors. The unbound 1% is called free T3 (and free T4) and is what’s responsible for the metabolic effects. When the thyroid is disrupted all sorts of things can go wrong. People who have an underproduction of thyroid hormones have hypothyroidism. Hypo– means low, or under, thyroid indicates the thyroid, and –ism means a condition of. Hypothyroidism is a condition where the thyroid underproduces hormones. Hypothyroidism affects between 2-11% of the adult US population. The primary risk factor is age, with those over sixty having higher rates of hypothyroidism. It is 20 times as prevalent in women. Worldwide, the highest cause of hypothyroidism is low iodine intake, which restricts T4 and T3 production. Here in the US we get plenty of iodine in our diets, so the highest cause here is autoimmune inflammation, a condition called Hashimoto’s disease. The next highest cause of hypothyroidism is treatment for hyperthyroidism – when the thyroid is overactive. This makes intuitive sense, as getting the balance exactly perfect is nearly impossible. In rare cases, the hypothalamus or pituitary gland may malfunction. The causes of hypothyroidism can be widespread, and so can the effects. When tissues can’t get enough T3, all sorts of problems arise. Common symptoms include fatigue, weight gain, changes to hair and skin, sensitivity to cold, and mental changes to mood and memory. Several patients experience no symptoms, and several patients have comorbidities (such as other autoimmune inflammation), making isolating symptoms and causes difficult. Untreated hypothyroidism can lead to heart problems and swelling of the thyroid, which is called a goiter. So what can be done? Is there any hope? It should be no surprise that the solution to hypothyroidism is to take supplemental T4 and/or T3. In ye olden days (the 1950’s) the solution to hypothyroidism was to consume dried and prepared sections of animal thyroid – which would otherwise go to waste anyway. This can still be found under several names: desiccated thyroid, thyroid extract, Armour Thyroid, Thyroid USP, natural thyroid, and more. In the 1960’s, levothyroxine – synthetic T4 – was developed. A diagnosis of hypothyroidism may include low T4 and T3 levels, along with elevated TSH. Levothyroxine has been the standard treatment since the 1960’s and can bring hormone levels back in line. Unfortunately, a significant amount of patients do not find symptomatic relief from levothyroxine. It is thought that even though T4 levels are being raised, T3 may not be reaching the tissue. Perhaps the feedback loop isn’t complete. To compensate for this, some doctors have been prescribing T3 along with levothyroxine, with mixed results. Researchers have also been studying if the past solution, animal thyroid, may be the future solution. Thyroid extract generally results in lower free T4 and more free T3. With luck (and clinical trials!) we can find solutions to keep the butterfly in our throats flying high and functioning majestically. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Biondi, B., & Wartofsky, L. (2014). Treatment with thyroid hormone. Endocrine reviews, 35(3), 433-512. https://academic.oup.com/edrv/article/35/3/433/2354656 Boucai. L., (2024). Overview of thyroid function. Merck Manual, Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/hypothyroidism Boucai. L., (2024). Hypothyroidism. Merck Manual, Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/hypothyroidism Hegedüs, L., Bianco, A. C., Jonklaas, J., Pearce, S. H., Weetman, A. P., & Perros, P. (2022). Primary hypothyroidism and quality of life. Nature Reviews Endocrinology, 18(4), 230-242. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8930682/ Wyne, K. L., Nair, L., Schneiderman, C. P., Pinsky, B., Antunez Flores, O., Guo, D., … & Tessnow, A. H. (2023). Hypothyroidism prevalence in the United States: a retrospective study combining national health and nutrition examination survey and claims data, 2009–2019. Journal of the Endocrine Society, 7(1), bvac172. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9706417/
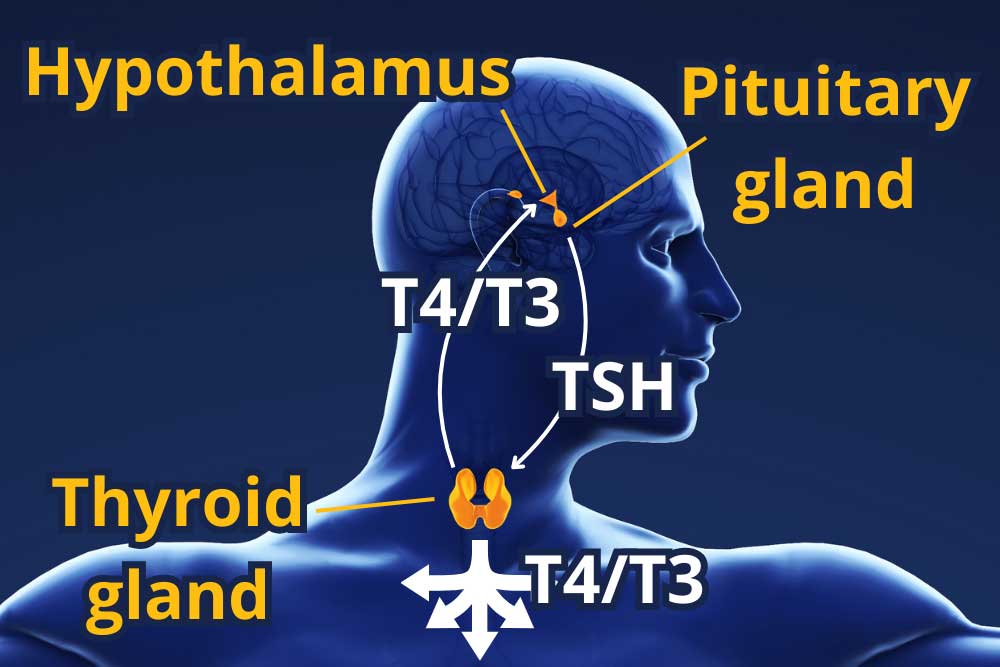
Listen to the article here:
We’ve all been there: we finally ask out the total hottie we’ve been crushing on for months, only for them to reply with “…who are you?” Oof and ow. Hands tremble, eyes water, we turn away in shame, and our heart literally breaks in half. This is very dangerous! The heart actually works best when it’s all in one piece, pumping blood, and not when it’s in many pieces crying.
Scientists have long looked for ways to mend a broken heart. The classic adage “time heals all wounds” has been the primary standard of care, but that has been deemed “very boring” by experts. Other researchers have looked into things like “sad music,” “eating,” and “partying.” In spite of these classical treatments, over the course of someone’s life, there is a nearly 100% chance they will experience hurt feelings! Clearly, a new approach is needed. Previous methods of dealing with heartbreak have all been focused on the mental state; our psychological health. Now research scientists have been looking into physically reassembling the heart. Initial attempts at welding and gluing failed. Researchers went back to first principles to find the proper adhesive. Then, Dr. Jimmy Scientist – who was having an HVAC system installed in his house – looked up what a duct was. The first Google result says a duct is “a bodily tube or vessel.” The heart is a pump, sure, but it still has blood flow through it, which sorta makes it a duct. Using the axiom of “well technically…” scientists recently announced a new way to fix a broken heart: duct tape!
Using duct tape to fix a broken heart is not an easy process. Taping it all back together requires open heart surgery which has been described as “ouchie” and “yucky.” On top of this, the tape doesn’t stick if the heart is all wet and bloody, so they have to drain all the blood out of you first, which can make you light-headed. Then surgeons have to find most (at least a few) of the little broken pieces and tape it all together. At the end of the procedure, a really good doctor will even remember to put the blood back in the body. So how does this work? A healthy heart pumps blood using the power of squishy-wishy. This blood reaches your whole body, including the brain. Some scientists suspect the brain might actually be a vampire because it really likes blood. In fact, the brain drinks ~2 ½ cups of blood every minute, which has been described as “radical” and “totally metal.” The brain is happy when it drinks this blood, and that makes you happy. When the heart is all leaky and broken, however, the brain can’t get enough blood. It gets angry and starts fluttering its bat wings or whatever. This can wobble your tear ducts, causing them to leak, and also makes your feelings hurt.
Duct tape keeps the heart watertight (bloodtight?!?) and gives it a chance to squish-wish blood up to your endraculated brain. With luck, we’ll be able to bounce back from heartbreak with speed. So if you experience heartbreak before the next April Fool’s, consider the duct tape method: all it takes is some open-heart surgery, a roll of adhesive tape, and a surgeon with no scruples. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: No.

Listen to the article here:
We all do things for our parents. Some of us make them a card for their birthday, call them to say hello, or discover key mechanisms behind how the body metabolizes sugar in an attempt to save them from diabetes. Falling into that last category is the first American woman to win a Nobel Prize, Dr. Gerty Cori. She was born to a Jewish family in Prague in 1896. She became a doctor, got married, and worked in research at Carolinen Children’s Hospital. Gerty and her husband, Carl, collaborated and published multiple papers. Central Europe became challenging for Jewish people during the interwar period. She immigrated to the USA with her husband in the 1920s and naturalized in 1928. Her father was diagnosed with diabetes, and it’s said that’s where she got her inspiration. America in the first part of the 20th century was a tough place to be a female researcher. Gerty Cori’s husband was offered prestigious positions that were denied to Gerty based on her gender. Carl Cori would not stop collaborating with his wife and refused positions where Gerty was not welcome. They eventually were hired at Washington University in St. Louis, though Gerty was given a token salary 1/10th of what Carl made. There, Gerty and Carl collaborated and investigated how sugar was broken down and stored in the body. It was said that Gerty had the ideas, and together the husband and wife team made breakthroughs. This culminated in their description of how the body delivers energy to muscles during intense exercise in what came to be called the Cori Cycle. The Cori Cycle is essential to our understanding of how the liver and muscles work together. Our muscles need energy to do anything and everything. Normally, sugar in the form of glucose is broken down using oxygen, releasing energy. During prolonged and/or intense exercise, we can’t get enough oxygen to the muscles fast enough, and they have to produce energy without oxygen. To do this they convert glucose to pyruvate to lactate. Lactate is released into the blood, where it could cause damage if not for the liver. Gerty Cori and her husband’s experiments found that the liver regenerates glucose from the extra lactate. The liver uses more energy to make the glucose than the muscles can generate from it without oxygen, so the Cori Cycle is the shifting of the energy production from the muscles to the liver. Because of this and other critical work illuminating how the body metabolizes glucose, Gerty and her husband shared the 1947 Nobel Prize in Physiology and Medicine, making Gerty the first American woman to win the prize. Earlier that year, Gerty was also finally offered a full professorship at Washington University. She continued her work on glucose metabolism and spent time investigating enzymes and hormones. Her work would later be critical to our understanding of how glucose is regulated through the body, giving targets for diabetes medications. This Women’s History Month, as we honor the remarkable women who have impacted our world, let’s recognize the pioneering spirit of the first American woman to win a Nobel Prize in Physiology or Medicine. Her groundbreaking work laid the foundation for our understanding and treatment of diabetes. We can draw on her inspiration to make our parents proud and continue the legacy of progress and compassion. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: National Center for Biotechnology Information (2024). PubChem Pathway Summary for Pathway WP1946, Cori cycle, Source: WikiPathways. Retrieved March 19, 2024 from https://pubchem.ncbi.nlm.nih.gov/pathway/WikiPathways:WP1946. Washington University School of Medicine. (2004). Gerty Theresa Cori. Bernard Becker Medical Library. https://beckerexhibits.wustl.edu/mowihsp/bios/cori.htm Ginsberg, J. (2010). Carl and Gerty Cori and Carbohydrate Metabolism. National Historic Chemical Landmark. https://www.acs.org/education/whatischemistry/landmarks/carbohydratemetabolism.html Gerty Cori – Biographical. (1964). Nobel Lectures, Physiology or Medicine 1942-1962. Elsevier Publishing Company. https://www.nobelprize.org/prizes/medicine/1947/cori-gt/biographical/
Listen to the article here:
I’ve been watching horror films lately, so before we get into the main topic of lipoproteins let’s talk about blood. Blood is watery and kind of gross but very useful. I like to think of the bloodstream as a highway we use to transport nutrients, cells, molecules, water, and waste to and from all the cells in the body. One problem with blood is that it can’t transport things that don’t dissolve in it very well. Fats, also called lipids, don’t dissolve in water, a lesson I think we all learned with the old oil and water demonstration from elementary school. Because of this, the body bundles lipids into little packages that can dissolve in watery blood. These packages combine water-repelling lipids with special proteins that organize them so they can flow through the blood. These lipid-protein packages are called lipoproteins. They have more functions than just transport, but that’s the one we’re focusing on today. Lipoproteins aren’t just determined by their size, however. Connected to the lipoproteins are other special proteins called apolipoproteins (apo– meaning “next to” or “away”). These determine how lipoproteins form, act, are recognized, and are broken down. One dangerous lipoprotein variant is apolipoprotein (a), usually shortened to apo(a). When this attaches to an LDL-like particle, it is called Lp(a). Since the names are important and the letter “a” is common in this space, it is usually pronounced “Lp little a.” Lp(a) is bad news. When apo(a) attaches to an LDL, everything changes. The density of Lp(a) changes and it is more likely to clog the bloodstream. High amounts of low-density lipoproteins (including Lp(a)) can cause a lot of damage to the cardiovascular system, increasing the chances of serious cardiovascular events like cardiovascular disease, heart attack, and stroke. Even worse, the body can’t break down Lp(a) the same way it does LDL, so the problems of high “bad” cholesterol are compounded. Because of this, classic methods of controlling cholesterol – lifestyle changes like diet and exercise, statins, and other medication typically have no effect on Lp(a) levels! High Lp(a) is a serious health problem, affecting around 20% of people. Levels of Lp(a) in the bloodstream can vary up to 1000x from person to person! The highest levels are seen in Black and South Asian populations. As stated earlier, Lp(a) levels are unaffected by normal risk factors. Instead, Lp(a) is genetically controlled. If your parents have elevated Lp(a), it is likely you will too. The problem is one of several genetic mutations that affect the amount of Lp(a) created. As we discovered earlier, Lp(a) doesn’t break down like normal LDL, so levels are primarily determined by how much is produced. So what can we do if we have high Lp(a)? As unintuitive as it sounds, diet and exercise are still good options! This isn’t because they affect Lp(a) levels, but because a healthy lifestyle can help protect your heart. Medications that protect the cardiovascular system may also be protective against high Lp(a) levels. Currently, in extreme cases, some patients may undergo a process called lipoprotein apheresis. This is where the blood is removed from the body and lipoproteins are physically separated from the blood before it is returned to the body, just like a good horror movie! Clinical trials are investigating methods of enhancing the body’s ability to break down Lp(a) or disrupt the production of Lp(a). Production may be targeted by disrupting the body’s ability to produce apo(a)! Consider joining a research study to help find new treatment options for high Lp(a). Also, with Lp(a) day approaching on March 24th, impress all your friends with your new pedantic vocabulary. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Biggerstaff, K. D., & Wooten, J. S. (2004). Understanding lipoproteins as transporters of cholesterol and other lipids. Advances in physiology education, 28(3), 105-106. https://journals.physiology.org/doi/full/10.1152/advan.00048.2003 Devaraj, S., Semaan, J. R., & Jialal, I. (2019). Biochemistry, apolipoprotein B. https://europepmc.org/article/NBK/nbk538139 Feingold, K. R. (2024). Introduction to lipids and lipoproteins. Endotext [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK305896/ Kamstrup, P. R., Neely, R. D. G., Nissen, S., Landmesser, U., Haghikia, A., Costa-Scharplatz, M., … & Nordestgaard, B. G. (2024). Lipoprotein (a) and cardiovascular disease: sifting the evidence to guide future research. European Journal of Preventive Cardiology, zwae032. https://academic.oup.com/eurjpc/advance-article/doi/10.1093/eurjpc/zwae032/7585314 Koschinsky, M. L., Stroes, E. S., & Kronenberg, F. (2023). Daring to dream: Targeting lipoprotein (a) as a causal and risk-enhancing factor. Pharmacological Research, 106843. https://www.sciencedirect.com/science/article/pii/S1043661823001998 Lampsas, S., Xenou, M., Oikonomou, E., Pantelidis, P., Lysandrou, A., Sarantos, S., … & Siasos, G. (2023). Lipoprotein (a) in Atherosclerotic Diseases: From Pathophysiology to Diagnosis and Treatment. Molecules, 28(3), 969. https://www.mdpi.com/1420-3049/28/3/969 Schmidt, K., Noureen, A., Kronenberg, F., & Utermann, G. (2016). Structure, function, and genetics of lipoprotein (a). Journal of lipid research, 57(8), 1339-1359. https://www.jlr.org/article/S0022-2275(20)35208-1/fulltext
Lipoproteins are very neat. The outside is a membrane very similar to a human cell. The inside is a mix of lipids, including triglycerides and cholesterol, and the proteins hold everything together. Lipoproteins travel through the bloodstream, carrying important lipids to cells all over the body. They can be sorted by size and “density,” but density is defined differently here, more like buoyancy. Imagine a pot of water. Olive oil is almost entirely made of lipids, and if you pour it into the pot of water it floats on the surface; it’s low-density. A steak contains a lot of fatty lipids, but there’s also a ton of protein in steak. Toss it in a pot of water and it sinks (and becomes gross); it’s high-density. Lipoprotein density is more about the ratio of lipid to protein. Even more fascinating is that the ratio of lipid to protein can change over time! A very low-density lipoprotein (VLDL) will deliver triglycerides (a type of lipid) from the liver to cells, lose some density, and may become an intermediate-density lipoprotein (IDL). These are proportionally higher in cholesterol. An IDL may deliver more lipids to become a low-density lipoprotein (LDL). LDL is the primary transporter of cholesterol through the body and delivers it to cells, which use cholesterol for some essential purposes, including maintaining the membrane that surrounds cells. High-density lipoproteins (HDL) work in reverse. They transport cholesterol from the cells back to the liver, getting larger (and lower in density) as they pick up more material.Listen to the article here:
I remember my introduction to puberty, my real introduction. It wasn’t a growth spurt, a voice change, or new body hair. It was a big. fat. zit. Right on the face. I was lucky, only getting a few zits here and there, but they still managed to kill my confidence. Unfortunately, it can be much, much worse for many people. Acne affects hundreds of millions of people worldwide and millions in the United States alone. Though most (85%) people experience acne in adolescence, nearly half of adults in their twenties have the condition. Beyond a simple zit here or there, acne can cause grease, lesions, and permanent scarring to the face and upper body. Acne can be graded based on the severity as mild, moderate, or severe. This can have serious negative impacts on mental health and quality of life. To really get under the skin of what’s going on with acne and what to do about it we first have to understand where and how it happens. Acne arises in the sebaceous gland. Sebaceous comes from Latin and shares its root word with soap. These glands produce an oily fat called sebum that coats our hair and skin and helps keep them from drying out. Instead of being gross, they are super helpful. The gland itself is embedded in the skin with a hair follicle, where hair is made. Together, these make up a pilosebaceous unit (Latin for hair-grease). Along with producing oils, the sebaceous gland also has the ability to sense its surroundings. It detects and responds to changes on the skin and hormonal changes in the body. Unfortunately, they can be confused and cause acne.
There are many causes of acne, but they can be roughly divided into four main factors: increased sebum, obstruction of the pilosebaceous unit, colonization by a bacterium, and an inflammatory response. Increased sebum is when too much of the oily, waxy fat is produced. This is usually called androgen-mediated sebogenesis, which gives a clue. The issue is an imbalance of hormones known as androgens. These are a type of steroid that can cause the sebaceous gland to produce too much sebum, which can clog the pilosebaceous unit. This brings us to obstruction of the pilosebaceous unit. Most of the machinery of the pilosebaceous unit is located in the middle layer of skin, and it squeezes out of a small pore at the top. This pore can get clogged by sebum and hair components. A small clog is called a microcomedo. The micro– is there because the skin still looks and feels normal. If the buildup continues, there is swelling and we get a full comedo (plural comedones). This is the zit, a clogged pilosebaceous unit. Side note: the comedo can be fully covered (closed) or exposed to air (open). When covered, skin pigments are preserved and we get a whitehead. When open, oxygen causes discoloration and darkening of the sebum, leading to a blackhead. But why does the buildup start? What’s causing this excess production? Surprisingly, the culprit has to do with the skin microbiome! This includes large amounts of (mostly helpful) bacteria that live on and in the top few layers of the skin. With acne, the little guy in question is named cutibacterium acnes, formerly called propionibacterium acnes. This bacteria is everywhere and lives happily without oxygen inside your pilosebaceous unit your whole life. It usually regulates the stability of the sebaceous gland. There are multiple strains of cutibacterium acnes (c. acnes), and some are worse than others. On the surfaces of the bacteria are proteins that vary by strain and conditions around the sebaceous gland. These can help it survive and can fight other bacteria. In some instances, these proteins can attach to the parts of the pilosebaceous unit that sense its environment. In acne-causing strains of c. acnes, the proteins activate receptors that regulate inflammatory responses. These strains are more likely to be dominant when the skin microbiome is out of whack and/or the pilosebaceous unit is producing too much sebum. The problem with c. acnes, then, isn’t the bacteria itself, but destructive strains and a skewed skin microbiome. This brings us to the last factor contributing to acne: inflammation. Inflammation is the body’s response to dangerous invaders. It is responsive and quick but can have trouble learning from its mistakes. With acne, the inflammation system is activated by rogue c. acnes strains and attacks enemies that aren’t there. This results in the reddening and swelling typical of a zit. So, what can be done about acne? With the enormous number of people who get acne and the very public nature, there are a lot of treatments with varying results. Skin cleansers have inconsistent data showing efficacy. The first medical lines of defense are topical agents. Retinoids, derived from vitamin A, bind to skin cells and promote extra skin cell production, which helps clear sebaceous ducts and microcomedones. Benzoyl peroxide is cheap and effective, generating killer free radicals that enter the pilosebaceous unit and kill c. acnes indiscriminately. Topical antibiotics can be effective at combating rogue c. acnes, but improper or excessive use can create antibiotic resistance, an increasing problem with acne. The second lines of defense are systemic agents that affect the whole body. These include medications that suppress androgens, oral antibiotics, and systemic retinoids. Since they are systemic, side effects are typically more severe than with topical treatments, but they can be used to treat moderate-to-severe acne. But what if there were another way? On the very verge of research is a c. acnes vaccine! An effective vaccine would target just the dangerous strains of the bacteria and would hopefully provide lasting protection. With luck, future generations can be introduced to puberty with parental embarrassment instead of acne! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Barbieri, J. S., Wanat, K., & Seykora, J. (2014). Skin: basic structure and function. https://www.sciencedirect.com/referencework/9780123864574/pathobiology-of-human-disease Das, S., & Reynolds, R. V. (2014). Recent advances in acne pathogenesis: implications for therapy. American journal of clinical dermatology, 15, 479-488. https://link.springer.com/article/10.1007/s40257-014-0099-z Del Rosso, J. Q., & Kircik, L. (2024). The cutaneous effects of androgens and androgen-mediated sebum production and their pathophysiologic and therapeutic importance in acne vulgaris. Journal of Dermatological Treatment, 35(1), 2298878. https://www.tandfonline.com/doi/full/10.1080/09546634.2023.2298878 Dréno, B., Pécastaings, S., Corvec, S., Veraldi, S., Khammari, A., & Roques, C. (2018). Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: a brief look at the latest updates. Journal of the European Academy of Dermatology and Venereology, 32, 5-14. https://doi.org/10.1111/jdv.15043 Mayslich, C., Grange, P. A., Castela, M., Marcelin, A. G., Calvez, V., & Dupin, N. (2022). Characterization of a Cutibacterium acnes Camp Factor 1-Related Peptide as a New TLR-2 Modulator in In Vitro and Ex Vivo Models of Inflammation. International Journal of Molecular Sciences, 23(9), 5065. https://doi.org/10.3390%2Fijms23095065 Mayslich, C., Grange, P. A., & Dupin, N. (2021). Cutibacterium acnes as an opportunistic pathogen: An update of its virulence-associated factors. Microorganisms, 9(2), 303.
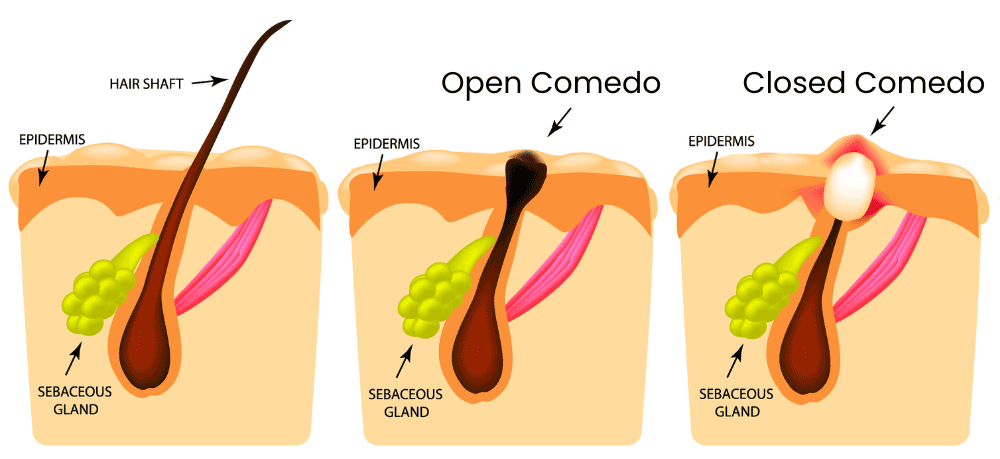
Listen to the article here:
Most of us have two kidneys. They are fist-sized and shaped like, um, kidney beans. The kidneys filter blood, but it’s more complicated than it sounds. They filter all the blood in the body several times a day. Kidneys differentiate between proteins, cells, minerals, acids, salts, and water. They regulate the amount of small particles to filter out or retain, and they release hormones to regulate blood pressure, red blood cell count, and some aspects of bone growth. To do this, each kidney is packed with tiny filtering units called nephrons (from the Greek word for kidney). Blood goes into these units, where it is separated and filtered by a structure called a glomerulus (from the Latin word for “ball of thread”). The filter has three layers which allow progressively smaller items through. The endothelium blocks cells and other large items. The glomerular basement membrane blocks proteins. The narrowest filter is called the epithelium and is made of special cells called podocytes (from the Greek word for foot). These look like octopi and use their many “legs” to form slits which regulate what gets through. Water, sodium, minerals, and acids are all separated from the blood. The nephrons sense the levels of these items and excrete excess amounts (along with waste products) into the urine. The pressure across the filter heavily influences filtering, so the kidneys have a system to regulate the blood pressure in the nephrons. Unfortunately, when kidneys are deformed, damaged, or otherwise can’t filter for a prolonged period we are subject to chronic kidney disease. Chronic kidney disease (CKD) is an enormous problem around the world. At least 13% of the global population (including 37 million Americans) live with chronic kidney disease. It is defined as an abnormality in structure or function for at least three months and is a big driver of cardiovascular disease. In the early stages, people may not have any symptoms; in fact, only around 5% of people with early CKD are aware they have the disease. Advanced CKD presents with myriad debilitating symptoms, including pain in the chest, changes in appetite and urination, headaches and fatigue, shortness of breath, skin issues, concentration issues, and more. Unfiltered blood can increase the amount of inflammation throughout the body. On top of all this is the most dangerous effect: damage to the cardiovascular system. When the kidneys fail to filter effectively, blood clots become more common, blood pressure may change, and the heart and vascular systems suffer. So what causes this to happen? Since chronic kidney disease is diagnosed based on kidney function and not cause, there are many potential culprits, and each patient will have different circumstances. Most risks can be divided into modifiable and non-modifiable. Modifiable risks may be managed through lifestyle or medication. One-third of people with diabetes have CKD. Diabetes may come with excessive glucose in the blood, which damages the blood vessels in the kidneys. High blood pressure, high cholesterol, obesity, and metabolic syndrome are other significant modifiable risk factors. On top of these, heart disease can lead to renal failure (which unfortunately then leads back to more heart disease). Non-modifiable risks include age, family history, and ethnicity. Let’s go a little deeper. When CKD is diagnosed or staged for severity, doctors look at the kidneys’ output. They may measure the amount of albumin, a component of blood, in the urine. High levels (over 30 milligrams in 24 hours) indicate issues. They may also try to measure or estimate the glomerular filtration rate (GFR). The average American starts with a healthy GFR of around 118 milliliters of blood each minute (mL/min), but someone with CKD filters fewer than 60 mL/min. This is the total amount of blood that is filtered per minute. It can be conceptualized as the filtration rate of a single nephron times the total number of nephrons. GFR gives a good indication of what goes wrong in CKD: the number of nephrons decreases significantly. Before we’re born, we have all the nephrons we’ll ever get – around one million per kidney. This is more than we need, and a person with healthy renal (Latin for kidney) function could donate literally half of them without suffering ill effects. We tend to lose nephrons over our lives, but the rest take up the slack. As nephrons are destroyed, the amount that each one filters has to increase. They try to grow and compensate, and they are often successful. With CKD, the compensation fails, and nephrons suffer compounding damage. High blood pressure in the kidneys can cause the filter to let in improper substances. It can also cause the podocytes to detach and clog the nephron. So what can we do? Despite a lot of effort, we have no way to clean the filters or regenerate nephrons (though scientists are trying!). Current best practice is to mitigate the risks posed to other parts of the body, especially the cardiovascular system. Anticoagulants are used to stop clotting in the bloodstream. These come with the unintended side effect of making bleeds worse, so new anticoagulants that target things like FXI are being investigated to make the blood vessels less prone to clots. Other solutions include mitigating inflammation, reducing the effects of excess albumin, and managing medications and complications that may cause a feedback loop with renal distress, like blood pressure and cardiovascular risks. Clinical trials targeting CKD are currently enrolling, so let’s give unfiltered thanks to our kidneys! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Evans, M., Lewis, R. D., Morgan, A. R., Whyte, M. B., Hanif, W., Bain, S. C., … & Strain, W. D. (2022). A narrative review of chronic kidney disease in clinical practice: current challenges and future perspectives. Advances in therapy, 39(1), 33-43. https://pubmed.ncbi.nlm.nih.gov/34739697/ Chen, T. K., Knicely, D. H., & Grams, M. E. (2019). Chronic kidney disease diagnosis and management: a review. Jama, 322(13), 1294-1304. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7015670/ Lin, L., Tan, W., Pan, X., Tian, E., Wu, Z., & Yang, J. (2022). Metabolic syndrome-related kidney injury: A review and update. Frontiers in Endocrinology, 13, 904001. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.904001/full National institute of Diabetes and Digestive and Kidney Diseases. National Institutes of Health. (October, 2016). Chronic Kidney Disease. U.S. Department of Health and Human Services https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd Puy, C., Rigg, R. A., & McCarty, O. J. (2016). The hemostatic role of factor XI. Thrombosis research, 141, S8-S11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6135087/ Romagnani, P., Remuzzi, G., Glassock, R., Levin, A., Jager, K. J., Tonelli, M., … & Anders, H. J. (2017). Chronic kidney disease. Nature reviews Disease primers, 3(1), 1-24. https://www.nature.com/articles/nrdp201788
Listen to the article here:
180 years ago, a doctor in the Austrian Empire conducted a radical experiment that has saved millions of children but cost him his life. This shocking, ground-breaking experiment involved doctors washing their hands. I know, I know, it sounds ridiculous, but doctors not only didn’t wash their hands back then, they were opposed to the very idea so much that the researching doctor was institutionalized and beaten to death. In this article, we’ll explore the history of handwashing, how they came up with the experiment, why people weren’t washing their hands in the first place, why the experiment worked, and how modern hand washing works. Then, we’ll dive into some nitty-gritty science. Handwashing is old. Like, it’s really old. We have good evidence of soap from nearly 3000 years ago. Handwashing as a ritual before meals is in Abrahamic religious texts. It was recorded in ancient Egyptian and Greek civilizations and is even practiced by raccoons. But this was superficial handwashing, mostly meant to get rid of visible dirtiness because we hadn’t discovered germs yet. Instead, ideas of how disease spread were based on things like miasma – the stinkiness of a dirty thing. Ignaz Semmelweis was a physician who, in the 1860s, got a residency in a maternity ward. In those days things were separated by gender, so there were two clinics. One was attended by male doctors and one by female midwives. Dr. Semmelweis noted that people died in the male-run clinic at a rate 300% higher than in the midwife-run clinic. He was appalled and wrote that women would have better outcomes giving birth in the street than in the hospital. The primary disease causing all the deaths was childbed fever, now known as (pew-er-per-al) puerperal fever. Luckily, Dr. Semmelweis had a shocking (shocking!) insight. He theorized that perhaps the fact that the doctors would do autopsies before going to the maternity ward was causing some of the “cadaverous particles” to infect the patients. He got this idea when a fellow doctor cut himself during an autopsy and subsequently died of childbed fever. Dr. Semmelweis concluded that doctors should wash their hands in chlorinated water upon entering the maternity clinic! Within a year the death rate plummeted from ~10% to under 2%. Unfortunately, doctors were reluctant to change their ways. The theory that doctors could be killing their patients was seen as offensive and came with the implication that doctors were unclean, which went against the class system of the era. He was reluctant to release his findings, but when he did they were dismissed and his reputation was ruined. In his book Die Aetiologie, der Begriff und die Prophylaxis des Kindbettfiebers, he is racked with guilt. He was committed to an insane asylum where he was beaten to death by the orderlies within weeks under suspicious circumstances. It would be decades before germ theory gave an explanation for Semmelweis’s findings and brought them back into the public consciousness. He would never know how many millions of children and mothers he saved. In Dr. Semmelweis’s day, they used chlorinated water to wash their hands. Let’s dive into modern-day hand washing. How does washing hands work? Why do we need to wash our hands, even if they look clean? Are there better ways to wash hands? Is hand sanitizer just as good? To start, let’s look at the skin as an immune organ. The skin is awesome. It’s our biggest organ and is the primary defense against invading germs; the tiny microorganisms like bacteria, fungi, and viruses. The skin has three major defense mechanisms. Our immune cells fight organisms that get too close for comfort and our skin hardens and sloughs off, taking bacteria and viruses with it. Before either of those, potential attackers have to deal with the skin microbiome. It turns out our skin isn’t just a cool canvas for tattoos but is an entire ecosystem for thousands and millions and billions of teeny little friends that make a living harvesting our sweat or whatever. Three important genera of bacteria take up the bulk of what we call the resident flora: cutibacterium, staphylococcus, and corynebacterium. These three coat our skin and enhance the immune protection skin gives us. They are commensal organisms, which is kind of like the mob. We give them food and shelter, and they promise to (mostly) do us no harm. They are called “residents” because they live with us our whole lives. They colonize our skin, making it hard for other invaders (called transient flora) to get a foothold. The defense mechanisms they have for themselves work well against the transient flora. In addition, they break down cholesterols we emit into free fatty acids which keep our skin a little acidic, killing invaders. They tend to reside deeper in the skin layers than transient bacteria, are less likely to cause infection, and are harder to remove. This is exactly where handwashing shines. Transient flora, like MRSA, multidrug-resistant gram-negative bacteria, Vancomycin-resistant Enterococci, and “cadaverous particles” tend to be closer to the outer layers of skin and are easier to remove. Effective hand-washing removes the transient flora but keeps the residents intact. Even more effective than just soap and water are antibacterials. These attack the transients in creative ways, degrading the cell walls, DNA, and proteins. Hand sanitizer is effective at destroying many bacteria and can be applied frequently and without a sink. So next time you wash your hands between visiting the morgue and the maternity ward, think of Dr. Semmelweis and thank him for his experimental vision! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Boyce, J. M. (2021). Hand hygiene, an update. Infectious Disease Clinics, 35(3), 553-573. https://doi.org/10.1016/j.idc.2021.04.003 Edmonds-Wilson, S. L., Nurinova, N. I., Zapka, C. A., Fierer, N., & Wilson, M. (2015). Review of human hand microbiome research. Journal of dermatological science, 80(1), 3-12. https://www.sciencedirect.com/science/article/pii/S0923181115300268 Skowron, K., Bauza-Kaszewska, J., Kraszewska, Z., Wiktorczyk-Kapischke, N., Grudlewska-Buda, K., Kwiecińska-Piróg, J., … & Gospodarek-Komkowska, E. (2021). Human skin microbiome: Impact of intrinsic and extrinsic factors on skin microbiota. Microorganisms, 9(3), 543. https://doi.org/10.3390/microorganisms9030543 Semrnelweis, I. (1861). Die Aetiologie, der Begriff und die Prophylaxis des Kindbettfiebers, C. A. Hartleben’s Verlag-Expedition, Translated by K. Codell Carter. Madison, 1983 https://archive.org/details/b28064045 Widmer, A. F. (2000). Replace hand washing with use of a waterless alcohol hand rub?. Clinical infectious diseases, 31(1), 136-143. https://academic.oup.com/cid/article/31/1/136/317796
Listen to the article here:
Alzheimer’s Dementia, often shortened to AD, is abjectly terrible. People with the disease lose memories, language, and the ability to function by themselves. It was first described over a hundred years ago by Dr. Alzheimer, and there has been startlingly little progress in treating the disease since. Alzheimer’s disease is a dementia characterized by two kinds of brain deposits: amyloid plaques and tau tangles. It’s the most common type of dementia. Dr. Alzheimer also noticed the distinct presence of extra cholesterol in the brain, which we will return to. We have few medications that are approved to help with Alzheimer’s. Even these don’t cure the disease but instead slow its progress. This indicates a fundamental lack of a good model for how the disease starts or progresses. The first big hypothesis for Alzheimer’s was the cholinergic hypothesis; that there is a paucity of a neurotransmitter called acetylcholine causing the damage. Unfortunately, drugs that increase acetylcholine don’t stop the disease progression. The second big hypothesis, the one that is currently in vogue, is the amyloid cascade hypothesis. According to this theory an amyloid precursor known as amyloid beta (Aβ) is the cause of Alzheimer’s. This makes a lot of sense, as Aβ is the main component of amyloid plaques and people with a genetic predisposition to make extra Aβ tend to get Alzheimer’s (called familial Alzheimer’s). There are a few inconsistencies in this hypothesis: the distribution of Aβ doesn’t match how bad the disease is, and risk factors that increase Aβ don’t match those of Alzheimer’s. To make matters worse, in spite of decades of research, over 99% of clinical research studies targeting Aβ have failed to bring a medication to market.1 Enter the Lipid Invasion Model. This is a new hypothesis developed in 2021 to explain the root cause of Alzheimer’s dementia. The basic idea is that the barrier between the brain and the rest of the body degrades, which allows cholesterols and free fatty acids to “invade” the brain and cause damage. The less basic idea is the rest of this article. To begin, let’s discuss the barrier between the brain and the body, aptly called the Blood Brain Barrier. The barrier is made up of the blood vessels of the brain. These are special blood vessels with unique properties. The cells that make up the walls of the blood vessels, called epithelial cells, are joined together with tight junctions that keep small charged particles from getting past. These epithelial cells are dotted with special transporters that only let in certain nutrients. Other brain cells called pericytes and astrocytes surround the epithelial cells (on the brain side) and keep out stragglers. This allows the brain to maintain the environmental conditions that it needs to function. Instead of letting a free flow of blood to cells, the blood brain barrier only lets in specific amounts of specific nutrients. One of the key items that is restricted by the blood brain barrier is lipids. “Lipids” is another name for fats. In the body they perform several vital functions, and in the brain they are critical. Even though the brain is only 2% of the body’s weight, it contains nearly a ¼ of the body’s cholesterol. It uses this for cell repair, creating synapses (learning), releasing communication particles, and for coating neurons to increase the speed of thought. The two lipids relevant to this discussion are cholesterol and free fatty acids. These are energy-dense particles that don’t dissolve in watery liquids like blood. Instead, they need to hitch a ride to be transported through the bloodstream. In the brain, cholesterols and free fatty acids must be transported in small, dense, protein-rich particles called lipoproteins. In the body, lipoproteins come in many different sizes (including low-density lipoproteins, known as LDL). In addition, free fatty acids can be transported in a different protein called albumin. Part of the blood brain barrier’s job is to keep these two systems of transporting lipids separate. The Lipid Invasion Model postulates that this separation system fails. When this happens the brain can’t handle the extra lipids. Free fatty acids in particular have a detrimental effect. They cause oxidative stress that can result in cell damage and change the energy regulation of neurons, causing problems, and activating immune receptors causing an inflammatory response. Inflammation can result in astrocyte cells producing extra cholesterol, making the problem worse. On top of this, excess lipids in the brain are thought to limit the ability of neurons to grow and cause the amnesia typical of Alzheimer’s. Finally, excessive lipids may cause the brain to create amyloid beta, the precursor to the stereotypical amyloid plaques. So what goes wrong with the blood brain barrier? Scientists think the barrier degrades over time. Those tight junctions loosen, the transporters let in too many items, or items of the wrong type, and different proteins on the surface of epithelial cells disrupt the barrier. Additionally, microbleeds in the brain let unrestricted blood flow through and interact without the epithelial cells’ consent. The barrier lets the wrong type of materials cross, including lipids. In Alzheimer’s patients, we see free fatty acids and non-brain-native lipoproteins (including the risky APOE4) spread through the brain. The risk factors for blood brain barrier damage are eerily similar to those of Alzheimer’s dementia: So what can we do with this new hypothesis? The most important step is to research it! I need to reiterate that this is only a hypothesis. It’s still only a few years old, and there is no experimental data verifying the veracity of this very vivacious version of Alzheimer’s. There is some early evidence the lipid invasion model may have merit; people on lipid-lowering statin medication have significantly lower rates of Alzheimer’s. If experimentation verifies the hypothesis, we may see new methods of targeting Alzheimer’s, hopefully with a much higher success rate! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Chaves, J. C., Dando, S. J., White, A. R., & Oikari, L. E. (2023). Blood-brain barrier transporters: An overview of function, dysfunction in Alzheimer’s disease and strategies for treatment. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease, 166967. https://eprints.qut.edu.au/244794/1/151230849.pdf 1Cummings, J. L., Morstorf, T., & Zhong, K. (2014). Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimer’s research & therapy, 6(4), 1-7. https://alzres.biomedcentral.com/articles/10.1186/alzrt269?_ga=2.232085279.1814812906.1525132800-565150820.1525132800 Hu, Z. L., Yuan, Y. Q., Tong, Z., Liao, M. Q., Yuan, S. L., Jian, Y., … & Liu, W. F. (2023). Reexamining the Causes and Effects of Cholesterol Deposition in the Brains of Patients with Alzheimer’s Disease. Molecular Neurobiology, 60(12), 6852-6868. https://link.springer.com/article/10.1007/s12035-023-03529-y Jick, H. Z. G. L., Zornberg, G. L., Jick, S. S., Seshadri, S., & Drachman, D. A. (2000). Statins and the risk of dementia. The Lancet, 356(9242), 1627-1631. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(00)03155-X/abstract Rudge, J. D. A. (2022). A new hypothesis for Alzheimer’s disease: The lipid invasion model. Journal of Alzheimer’s Disease Reports, 6(1), 129-161. https://content.iospress.com/articles/journal-of-alzheimers-disease-reports/adr210299 Rudge, J. D. A. (2023). The Lipid Invasion Model: Growing Evidence for This New Explanation of Alzheimer’s Disease. Journal of Alzheimer’s Disease, (Preprint), 1-14.https://content.iospress.com/articles/journal-of-alzheimers-disease/jad221175#ref007 Wang, H., Kulas, J. A., Higginbotham, H., Kovacs, M. A., Ferris, H. A., & Hansen, S. B. (2022). Regulation of neuroinflammation by astrocyte-derived cholesterol. bioRxiv, 2022-12. https://doi.org/10.1101/2022.12.12.520161 Xiong, H., Callaghan, D., Jones, A., Walker, D. G., Lue, L. F., Beach, T. G., … & Zhang, W. (2008). Cholesterol retention in Alzheimer’s brain is responsible for high β-and γ-secretase activities and Aβ production. Neurobiology of disease, 29(3), 422-437. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2720683/
Scroll down to listen to this article.
Listen to the article here:
If there’s one thing I learned in elementary school… well, it was probably how to read. But if there’s one thing I learned every year around this time, it’s that Valentine’s Day isn’t just for lovers but for friends and classmates, too. Valentine’s Day is the time of year we celebrate the most special people in our lives – and it’s a good time to investigate the health effects of love and social relationships. Love is a curious word. I love my wife and child, but also my cats, parents, siblings, friends, cookies, pizza, and ice cream. While some of my loves are potentially dangerous (or so my blood pressure tells me), my love of friends, family, and community might keep me alive – or at least balance the carbs. Studies have shown that maintaining social relationships can lower the rate of all-cause mortality: love literally increases your lifespan. This has been suspected for centuries and can be seen anecdotally in extreme examples with hermits, but it has been causally validated in recent years. Multiple studies in several countries have found that those with healthy social relationships are around half as likely to die over a given time span than isolated people. These relationships included marriage, contact with friends and family, and participation in communities like church, and other formal and informal groups. But how could our social lives affect our health? And what is the scientific definition of love anyway? Love is… hard to define. One of the best ways to describe love is as a motivation system. It’s not only an emotion because it lasts much longer and shapes how we act over long periods of time. Instead, it’s the part of our personality that recognizes our need for social relationships to survive and reproduce. A skillful lone person can survive in the wilderness or on a deserted island for a while, but they will have trouble if they break an arm or try to have children without anyone else around. We need each other, and one of the parts that ensures we will act prosocially is love. So what’s that look like inside the brain? Experiments show that a brain on love has a few hallmarks. The brain activates the reward system and parts of the cortex (medial insula, anterior cingulate cortex, hippocampus). The reward system encourages us to keep loving others and boosts dopamine, which makes us feel good, raises our desire, and acts in an almost addictive way similar to cocaine. The brain also lowers the activation of the amygdala, which is responsible for fear, the sympathetic “fight or flight” response, and chemicals like cortisol. Love also deactivates parts of the brain associated with social judgment, assessing other people’s intentions, and “negative emotions” like sadness. Serotonin is also suppressed, which may lead to obsessive symptoms similar to OCD. Love is both addictive and obsessive! Two hormones are released by the hypothalamus: oxytocin and vasopressin. Oxytocin is known as the “love hormone” and increases attachment and bonding. It’s released in romantic love and during childbirth. It is thought to help mothers bond with babies. Vasopressin also increases bonding and attachment while affecting blood pressure and the kidneys. This gives a clue as to how love can be healthy. In most developed nations (including the USA), the biggest causes of death aren’t from infectious diseases but from chronic ones. Diseases like heart disease are exacerbated by stress and stress hormones like cortisol and those of the sympathetic nervous system. Studies have shown that animals with social relationships have fewer ulcers and neurotic conditions and have lower blood pressure. Social support is able to mitigate stress and its negative effects. Love also has positive effects on the big picture of how we run our lives, giving us meaning, coherence, and promoting healthy behaviors like self-improvement and getting enough sleep (after college at least). So this Valentine’s Day, tell those around you that you love them. Appreciate the relationships and communities you are a part of and activate those obsessive and addictive parts of your brain on something healthy. It’s elementary, really. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Cuzzo, B., Padala, S. A., & Lappin, S. L. (2023). Physiology, vasopressin. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK526069/ House, J. S., Landis, K. R., & Umberson, D. (1988). Social relationships and health. Science, 241(4865), 540-545. https://www.researchgate.net/profile/Debra-Umberson/publication/19756223_Social_Relationships_and_Health/links/00b495220b128b3aec000000/Social-Relationships-and-Health.pdf Seshadri, K. G. (2016). The neuroendocrinology of love. Indian journal of endocrinology and metabolism, 20(4), 558. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4911849/ Zeki, S. (2007). The neurobiology of love. FEBS letters, 581(14), 2575-2579. https://www.sciencedirect.com/science/article/pii/S0014579307004875
Scroll down to listen to this article.
Listen to the article here:
I have two cats. They seem pretty smart, there’s definitely something going on in their minds. Unfortunately, I can’t see inside their thoughts, so it is hard for me to know just how capable they really are. Weirdly, this isn’t just a problem with cats, but people too. Many of us have the ability to talk, type, sign, or draw, but even with our most precise communication methods, it is impossible to find out what’s actually going on up there. The modern form of this problem was clearly explained in the 1960’s by the founders of cognitive psychology, the study of how people think. Cognition is a challenging field to study because even with imaging technologies that can look inside the brain, like MRIs and CAT scans, we can’t ever really know how a person is thinking. We can study the inputs and outputs, we can study how neurons fire, and we can look at the overall state of the brain, but the individual subjective experience escapes us. An example of subjective experience is color. Our experiences of color can be altered by external factors like tinted sunglasses, cataracts, and eye deformities, but we can also change it just by staring at a bright color for a long time, being out in the sun and coming inside, or even through the language we use to describe colors! Cognition is an interesting area of study but has real-world consequences. One of the challenges with the complexity of cognition and our subjective experience is gauging the presence and severity of mental decline. Unlike diabetes, where we can measure the amount of glucose in the blood, with mental decline and dementia, we have to rely on tests of cognition to measure how well or poorly someone performs cognitive tasks. The benchmark Mini Mental State Exam (MMSE) is the most widely used tool. MMSE is a relatively short (5-15 minute), untimed set of 20 questions that measure 11 domains of cognition: The MMSE can be repeated to track changes over time. The test alone is not a diagnostic tool; a low score does not confirm mental decline and further testing would be needed. Further, age and education level can also lead to lower scores. A high score, however, is unlikely in patients with dementia. This makes the MMSE a great tool for screening patients and quickly assessing patients who fear they may be slipping cognitively. Now, they need to make one for cats based on meows and mice. ENCORE Research Group provides complimentary Mini Mental State Examinations (MMSE) at designated research locations for individuals over the age of 60 who are worried about experiencing memory loss beyond what is considered age-appropriate. Those locations include: Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Yoo, S. G. K., Chung, G. S., Bahendeka, S. K., Sibai, A. M., Damasceno, A., Farzadfar, F., … & Flood, D. (2023). Aspirin for Secondary Prevention of Cardiovascular Disease in 51 Low-, Middle-, and High-Income Countries. JAMA, 330(8), 715-724. https://doi.org/10.1001/jama.2023.12905 Esenwa, C., & Gutierrez, J. (2015). Secondary stroke prevention: challenges and solutions. Vascular health and risk management, 437-450. http://dx.doi.org/10.2147/VHRM.S63791 American Heart Association News. (April 4, 2019). Proactive steps can reduce chances of second heart attack. American Heart Association. https://www.heart.org/en/news/2019/04/04/proactive-steps-can-reduce-chances-of-second-heart-attack American Heart Association. (2022). 5 ways to lower your risk of a second heart attack. American Heart Association. https://www.heart.org/-/media/files/health-topics/heart-attack/5-ways-to-lower-your-risk-of-second-heart-attack-infographic.pdf Karlin, R., Wojcik, S., Kang, S. (2024). Preventing a second heart attack. University of Rochester Medical Center Rochester. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=56&contentid=2446 de Jong, M., van der Worp, H. B., van der Graaf, Y., Visseren, F. L., & Westerink, J. (2017). Pioglitazone and the secondary prevention of cardiovascular disease. A meta-analysis of randomized-controlled trials. Cardiovascular diabetology, 16(1), 1-11 .https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5644073/
Scroll down to listen to this article.
Jacksonville Center for Clinical Research (904) 730-0166
Fleming Island Center for Clinical Research (904) 621-0390Listen to the article here:
One of the most important tasks for researchers is to make sure the experiment we are running is accurately assessing the intended variable. Because of this, each study has specific inclusion and exclusion criteria, which determine who can qualify to participate. An example would be needing a diagnosis of severe asthma for a study testing a new asthma medication. Usually, criteria include age, relevant medical diagnoses or histories, and exclude major health events such as cancer, heart attack, or stroke. Recently (as of the writing of this article), however, we have seen a notable uptick in the number of cardiovascular studies that allow or even require a previous heart attack or stroke as an inclusion criterion. This is because there are several medications or devices being studied that hope to lower the recurrence of these events. Heart attack and stroke are often two sides of the same coin. In both cases, blood flow to part of the organ is lowered or stopped, and the affected tissue is damaged or dies. You might be familiar with the term Major Adverse Cardiovascular Event (MACE), which encompasses various cardiovascular issues, including heart attack and stroke. Most people survive their first incident, but 20-25% of people have more than one. According to the American Heart Association, about 1 in 5 people who have had a heart attack will suffer from (or experience) a second one within five years. Each heart attack or stroke comes with a chance of lowered quality of life, disability, or death, so preventing further events is critical. One of the biggest problems with preventing a second heart attack or stroke is the myriad of causes of these conditions. Any prolonged insult to the cardiovascular system can lead to a heart attack or stroke. The risks, then, include a sedentary lifestyle, poor diet, obesity or excess weight (especially around the midsection), high blood pressure, high cholesterol, uncontrolled diabetes, smoking, stress, alcohol, and drugs. The solutions to these disparate causes can also spread far and wide. For this reason, the two most important ways to reduce the risk of a second heart attack or stroke are to talk to a medical professional and take prescribed medications. A medical professional can look at the underlying condition of individuals and determine which factors likely had the biggest impact. They may recommend cardiac rehabilitation and specific medications to address underlying conditions and prevent recurrence. Targeting specific, relevant causes with medications, such as anticoagulants like warfarin, antiplatelets like aspirin, and cholesterol-lowering medications like statins, can reduce the risk of resurgence by up to 70%! Doctors may also recommend medications to help with diabetes or blood pressure and/or surgical procedures to fix structural problems with the cardiovascular system. Managing the risk factors that caused the first heart attack or stroke can reduce the likelihood of a second (or third). On top of this, changes to lifestyle and diet can have a significant impact, lowering the chance of a second event by almost a third. Add a reduction in smoking, alcohol, and drugs for an even greater effect. Beyond standard medical advice, two additional interventions may help. The first is support. Family, friends, and others who have experienced heart attacks and strokes can help make the recovery process more bearable and lower anxiety and stress (which are risk factors in themselves!). Finally, clinical trials may help. Indeed, the inclusion of previous heart attacks or strokes in clinical research inclusion criteria indicates an increased recognition that indirect influence can induce repeated injury to the heart and brain. In short, research studies are looking at new ways to lower the incidence of a second heart attack or stroke by targeting underlying conditions with new medications and new methods of treatment. This is invariably a great idea. Only YOU (and your doctor (and maybe a clinical research coordinator)) can prevent secondary strokes and heart attacks. At the time of this writing, ENCORE Research Sites have several studies for people who have had a previous heart attack or stroke. Call your local office to explore research options for you. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Yoo, S. G. K., Chung, G. S., Bahendeka, S. K., Sibai, A. M., Damasceno, A., Farzadfar, F., … & Flood, D. (2023). Aspirin for Secondary Prevention of Cardiovascular Disease in 51 Low-, Middle-, and High-Income Countries. JAMA, 330(8), 715-724. https://doi.org/10.1001/jama.2023.12905 Esenwa, C., & Gutierrez, J. (2015). Secondary stroke prevention: challenges and solutions. Vascular health and risk management, 437-450. http://dx.doi.org/10.2147/VHRM.S63791 American Heart Association News. (April 4, 2019). Proactive steps can reduce chances of second heart attack. American Heart Association. https://www.heart.org/en/news/2019/04/04/proactive-steps-can-reduce-chances-of-second-heart-attack American Heart Association. (2022). 5 ways to lower your risk of a second heart attack. American Heart Association. https://www.heart.org/-/media/files/health-topics/heart-attack/5-ways-to-lower-your-risk-of-second-heart-attack-infographic.pdf Karlin, R., Wojcik, S., Kang, S. (2024). Preventing a second heart attack. University of Rochester Medical Center Rochester. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=56&contentid=2446 de Jong, M., van der Worp, H. B., van der Graaf, Y., Visseren, F. L., & Westerink, J. (2017). Pioglitazone and the secondary prevention of cardiovascular disease. A meta-analysis of randomized-controlled trials. Cardiovascular diabetology, 16(1), 1-11 .https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5644073/
Scroll down to listen to this article.
Listen to the article here:
The immune system is awesome, but overwhelming. It’s filled with billions of cells and quintillions of proteins. There are neutrophils, dendritic cells, antibodies, B cells, macrophages, lymphoid cells, lymphocytes, the complement system, and more! Instead of trying to understand the whole thing, let’s narrow our focus down to just one type of cell, the T cell, and just one variant, T-helper 17, or Th17. T-cells are a type of white blood cell and are about the size of a red blood cell. They are adaptive, which means they change in response to threats. These cells start as virgin (or naïve) cells and transform into a specialized version when danger is detected. T-cells can be divided into two parts: killers and helpers. Killers are good at killing other (hopefully bad) cells, while helpers activate other cells and amplify immune responses. The cell we’re focusing on, Th17, is a type of helper cell, but a special one. Th17 was first identified in 2005, but scientists have rapidly learned loads about it. It is particularly good at helping the body fight unusual attackers like fungi and certain bacteria. When activated, it releases a powerful signaling chemical that increases inflammation and recruits other white blood cells, telling them to come and fight. In addition, it can assist in tightening the spaces between our border cells to keep invaders out. When the body detects unknown particles, cells release signaling molecules. When a T-helper cell encounters the right mix of these molecules, it transforms into the rallying Th17 captain which sounds the alarm. Unfortunately, all that shimmers is not silver. Th17 can certainly be useful in some circumstances, but it can be dangerous when activated by the wrong signals. In many of these cases, Th17 cells tell white blood cells to go nuts and attack anything that moves (or doesn’t move), but without a clear opponent, they just attack whatever’s around and cause an autoimmune response. Th17 has been implicated in diseases like experimental autoimmune encephalomyelitis (EAE), arthritis, and inflammatory bowel diseases (IBD) like Ulcerative Colitis. Let’s look at ulcerative colitis as an example. Ulcerative colitis is an inflammatory bowel disease where the immune system attacks benign bacteria or food particles. The causes aren’t clear, but part of the problem is a thinning of the mucus and separation of border cells that line the intestines. Many signaling molecules called interleukins (abbreviated IL-) are released in the disease state, including three important ones for Th17. These are IL-1β, IL-6, and IL-23 (write this down for the quiz at the end). The first two activate Th17, and that’s when IL-23 can turn it into a problem. In the presence of IL-23, Th17 sends wild signals and can cause the autoimmune problems listed above, including ulcerative colitis. Also, remember how Th17 helps tighten the spaces between border cells? It turns out that in the presence of IL-23 this function doesn’t work properly and the borders stay open, letting in more particles that the body attacks with inflammation. Scientists have been trying to find ways to solve the problems caused by Th17 since long before it was even known to exist. In the past, a treatment for something like ulcerative colitis might have been limited to restricting your diet. Currently, anti-inflammatory medications, steroids, and/or surgeries are used. Those are all big solutions bound to affect many other parts of the body and immune system. Now that Th17 has been identified as an occasional dirty traitor, researchers are instead targeting this specific cell to hopefully stop it from being activated incorrectly. With luck, we can help the T-helper cell to help us instead of unhelping us. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Kałużna, A., Olczyk, P., & Komosińska-Vassev, K. (2022). The role of innate and adaptive immune cells in the pathogenesis and development of the inflammatory response in ulcerative colitis. Journal of clinical medicine, 11(2), 400. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8780689/ Sender, R., Weiss, Y., Navon, Y., Milo, I., Azulay, N., Keren, L., … & Milo, R. (2023). The total mass, number, and distribution of immune cells in the human body. Proceedings of the National Academy of Sciences, 120(44), e2308511120. https://doi.org/10.1073/pnas.2308511120 Tesmer, L. A., Lundy, S. K., Sarkar, S., & Fox, D. A. (2008). Th17 cells in human disease. Immunological reviews, 223(1), 87-113. https://doi.org/10.1111/j.1600-065X.2008.00628.x Wu, B., & Wan, Y. (2020). Molecular control of pathogenic Th17 cells in autoimmune diseases. International immunopharmacology, 80, 106187. https://doi.org/10.1016/j.intimp.2020.106187
Scroll down to listen to this article.
Listen to the article here:
Heart failure is when the heart doesn’t pump enough blood throughout the body. This doesn’t mean instant death, but the body starts wearing out around the edges. People with heart failure might feel short of breath and tired because there’s not enough oxygen reaching the brain and cells. Ankles and lower extremities might start swelling because the heart is unable to pull all of the blood up out of our legs. Sufferers understandably have trouble exercising. So what’s going on? Can anything be done about it? Heart failure is an enormous problem. Tens of millions of people worldwide suffer from it, including at least 6 million Americans. It is the most common cause of hospitalization for adults over 65, and causes many repeat hospitalizations. Heart Failure severely reduces the quality of life, and comes with a high mortality rate. The causes of heart failure are numerous and can be difficult to identify; anything that impairs the heart’s ability to pump or deliver oxygen can be a contributing factor. Risk factors include: To understand how these conditions may contribute to heart failure, we should first dive wholeheartedly into how the heart works. The heart is a muscle. It squeezes about once a second in a coordinated fashion. This squeezing pushes blood to and from the lungs, and to and from the body. We generally don’t get new heart muscle cells as adults. Instead, in order to react to changes in the needs of the body the heart cells themselves can grow (enlarge), as can the structure around and between the cells. A healthy heart may get stronger and more efficient in response to exercise or pregnancy A weakened heart, on the other hand, might change its structure by enlarging in response to stress, hormone changes, inflammation, and/or the risk factors listed above. These changes can result in a reduction of the amount of capillaries that supply the heart with blood, as well as fibrosis, chemical changes, and changes in the metabolism and organization of heart cells. But why would the heart do this? Is it rebelling against us? Is it something I said? The heart loves us with its whole… self. It changes because it is trying its hardest and can’t manage to do it alone. When the heart senses it isn’t functioning properly, it may undergo cardiac hypertrophy. Cardiac is Greek (and Latin (and French)) for heart. Hyper- indicates an excessive amount, and -trophy is from the Greek word for nourishment, which in this case means growth. Cardiac hypertrophy is the excessive thickening or lengthening (or both) of the heart muscle. In pathological heart disease, scientists think this is initially an adaptive response. The heart attempts to compensate for dysfunction by increasing the size of the heart tissue. This works for a bit, right up until it doesn’t. Eventually, blood vessels can no longer reach all of the heart tissue. As a result, important chemicals like nitrous oxide are not produced and delivered to cells, connective tissue grows and stiffens, hormones get out of balance, and damaging inflammation occurs. These maladaptive signs of heart failure give evidence as to why it’s so dangerous. Each of these responses to a stressed heart can also cause damage and restructuring of the heart. Inflammation is a great example. Consistent inflammatory chemicals in the body can spur the heart into a stress response that results in structural changes, which in turn may cause inflammation that spreads to other parts of the body. Similarly we can look at hormones like angiotensin, which regulate blood pressure by affecting how narrow your blood vessels are. An excess of angiotensin can narrow blood vessels and cause the heart to work harder, leading to thickening of the tissue. However, when the stiff tissue doesn’t pump blood efficiently the body responds by releasing more angiotensin in an attempt to help blood move through the body. Regardless of the initial cause, when the heart can’t keep up with the demands of the body, heart failure occurs. So what can be done? Luckily, this problem has attracted some of the best minds on the planet (like our very own Dr. Michael Koren). Standard treatments aim to improve the quality of life and heart function in patients while reducing the incidence of hospitalization and mortality. Four classes of medications make up the standard of care (SOC) for heart failure: These SOC medications, though effective in many patients, are not perfect. While they tend to target and counteract the effects of wayward hormones, they do not address underlying heart dysfunction or the changes to heart structure occurring beneath it all. There are many new medications that target a host of new mechanisms for fighting the scourge of heart failure. These include targeting the inflammation pathways or simulating the effects of relaxin. Relaxin is a natural hormone with many effects, including recycling extra structural material in the heart and increasing the efficiency of heart muscle at the tissue level. With luck (and the help of excellent, well-read volunteers like yourself), we can turn heart failure into heart success. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Groenewegen, A., Rutten, F. H., Mosterd, A., & Hoes, A. W. (2020). Epidemiology of heart failure. European journal of heart failure, 22(8), 1342-1356. https://doi.org/10.1002/ejhf.1858 Lopaschuk, G. D., & Verma, S. (2020). Mechanisms of cardiovascular benefits of sodium glucose co-transporter 2 (SGLT2) inhibitors: a state-of-the-art review. Basic to Translational Science, 5(6), 632-644. https://doi.org/10.1016%2Fj.jacbts.2020.02.004 Murphy, S. P., Kakkar, R., McCarthy, C. P., & Januzzi Jr, J. L. (2020). Inflammation in heart failure: JACC state-of-the-art review. Journal of the American College of Cardiology, 75(11), 1324-1340. https://doi.org/10.1016/j.jacc.2020.01.014 Pandey, K. N. (2008). Emerging roles of natriuretic peptides and their receptors in pathophysiology of hypertension and cardiovascular regulation. Journal of the American Society of Hypertension, 2(4), 210-226. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2739409/ Shimizu, I., & Minamino, T. (2016). Physiological and pathological cardiac hypertrophy. Journal of molecular and cellular cardiology, 97, 245-262. https://doi.org/10.1016/j.yjmcc.2016.06.001 Xie, Y., Wei, Y., Li, D., Pu, J., Ding, H., & Zhang, X. (2022). Mechanisms of SGLT2 inhibitors in heart failure and their clinical value. Journal of Cardiovascular Pharmacology, 10-1097. https://doi.org/10.1097/FJC.0000000000001380
Scroll down to listen to this article.
Listen to the article here:
Last month, the US Food and Drug Administration approved two gene-editing therapies to treat sickle cell disease. This made national news in a way few drug approvals have, but why? What’s the big deal, and why should we care? Sickle cell disease is an inherited genetic disease affecting around half a million babies globally every year. People affected by sickle cell disease have genes that create malformed red blood cells that carry oxygen. These malformed cells become curved like a crescent moon (or a sickle), which results in poor oxygen delivery. Even worse, the curved cells can clump together into clots, which restrict blood flow and cause pain, organ damage, and/or death. Because it is genetic and there has been no known cure, it ranks consistently within the top 20 deaths of children. The disease is most prevalent in people of African descent, and globally the highest concentration of sufferers is in sub-Saharan Africa. Sickle cell disease is a result of problems with genetic mutation and malformed cells, which makes it very hard to target with traditional medicine. In spite of this, innovative researchers have developed two promising treatments for sickle cell disease. These use our own cells to help cure the disease – instead of an oral, topical, or injected medication. These are both gene therapies, where the genetic code of the patient is altered. This is an understandably touchy topic. Gene-editing is different from other medical procedures in that it may be inherited: your genes are passed to your children after all! The benefit of starting gene therapy with sickle cell disease is that we are starting with mutated genes. The mutated sickle-cell-creating genes will already be passed to any children, so fixing the mutations is likely to have better outcomes. I think of it like CPR. With CPR, you are starting with a person who isn’t breathing and has no circulation; you can’t really get any worse than that. With sickle cell gene therapy, as long as the gene-editing tools are specific and target the correct genes it is hard to do worse than one of the top killers of children worldwide. So what are the therapies that were approved? The first, Lyfgenia, is a gene-additive therapy. It uses a modified virus that can’t reproduce to infect cells and add new DNA. The virus, a lentivirus, delivers special RNA to the cells, which our cells incorporate into the DNA strand when they copy it. This genetic code tells the cells to make a different kind of hemoglobin – the protein in red blood cells that carries oxygen. This hemoglobin is a particular type that prevents sticking to the walls of bloodstreams. Note that viruses already deliver RNA that gets encoded into our genes all the time. A 2022 study looked at a protein and found that almost 10% of the human genome may be from viruses. The second therapy, Casgevy, is gene-editing in the most fundamental way. It uses a technology called CRISPR/Cas9 to cut and change pieces of our DNA. While our DNA may be around 10% viral, bacteria have much smaller genomes, and viral insertion of new DNA is a proportionally bigger problem. To combat this, some bacteria have a gene-editing system that can find and remove bits of wayward code. This system was adapted by very smart scientists into a gene-editing tool we can use to find and correct mutations in our genetic code. The process is pretty intense. Blood stem cells are removed from the body, then the CRISPR-Cas9 system edits them outside the body. The modified cells are reinserted into the bone marrow, where they will reproduce and turn into everyday functioning red blood cells. This is mind-blowing. Of course, there is controversy surrounding these therapies. One of the biggest is really unrelated to sickle cell disease, but instead to the very idea of gene-editing. This use of gene therapy in sickle-cell is hard to contest: we’re starting with mutated DNA in blood cells that can kill children. The what-ifs about adding new functionality like laser eyes or super strength get a lot of press and can make us question what it means to be human at a fundamental level. The second big problem is inequality. Could gene-editing be used to make a two-tiered system of wealthy people with great eyesight and perfect skill while poor people suffer? It very much looks like that, as Lyfgenia and Casgevy are both amazingly expensive, somewhere between 2-3 million dollars for treatment. But then, if we can permanently stop sickle cell for a person and all of their descendants, it may be worth it. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Food and Drug Administration. (December 8, 2023). FDA Approves First Gene Therapies to Treat Patients with Sickle Cell Disease https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease Milone, M. C., & O’Doherty, U. (2018). Clinical use of lentiviral vectors. Leukemia, 32(7), 1529-1541. https://www.nature.com/articles/s41375-018-0106-0 Frank, J. A., Singh, M., Cullen, H. B., Kirou, R. A., Benkaddour-Boumzaouad, M., Cortes, J. L., … & Feschotte, C. (2022). Evolution and antiviral activity of a human protein of retroviral origin. Science, 378(6618), 422-428. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10542854/ Thomson, A. M., McHugh, T. A., Oron, A. P., Teply, C., Lonberg, N., Tella, V. V., … & Hay, S. I. (2023). Global, regional, and national prevalence and mortality burden of sickle cell disease, 2000–2021: a systematic analysis from the Global Burden of Disease Study 2021. The Lancet Haematology. https://www.thelancet.com/journals/lanhae/article/PIIS2352-3026(23)00118-7/fulltext
Scroll down to listen to this article.
Listen to the article here:
This year has been exciting for clinical research. Our ENCORE sites completed 65 clinical trials (studies), and the FDA approved 66 new medications and vaccines nationwide. There is a long time between when a research organization or site, such as ours, completes a study and when a medication is ready for FDA review. Out of the 66 new medications or vaccines that were approved this year, ENCORE sites conducted seven of those clinical trials. That means all of you fantastic research volunteers helped get seven new medications or vaccines to market! In this article, we’ll review this year’s approvals and what they mean. Three new vaccines that received FDA approval this year had trials at ENCORE sites. Arexvy and Abrysvo were both approved for the treatment of Respiratory Syncytial Virus (RSV) in adults. This disease hospitalizes 177 thousand adults over 65 each year and causes over ten thousand deaths. Arexvy was the first vaccine approved against RSV in adults, and Abrysvo is intended for both prevention and treatment of RSV and is approved for use in pregnant women. Arexvy was studied at the Westside Center for Clinical Research and Abrysvo at Nature Coast Clinical Research – Crystal River. Ixchiq is the world’s first vaccine to be approved for Chikungunya. Chikungunya is spread to people by infected mosquitoes and causes fevers and joint pain. St. Johns Center for Clinical Research participated in two phase III clinical trials for Ixchiq. Two more ENCORE-researched medications approved this year were the first of their kind. Vowst has become the first medication to become FDA-approved for the treatment of C. difficile, also known as C. diff. C. difficile is a major health threat and causes colon inflammation. ENCORE Borland Groover Clinical Research investigated Vowst in the ECOSPOR trials. Veozah (fezolinetant) is the first non-hormonal treatment for moderate to severe vasomotor symptoms in women with menopause. These symptoms include hot flashes and night sweats, and Veozah targets the temperature centers of the brain to help with these symptoms. Three ENCORE research sites participated in the SKYLIGHT trials to investigate Veozah, Fleming Island Center for Clinical Research, St. Johns Center for Clinical Research, and Nature Coast Clinical Research – Crystal River. Two medications were approved, which may help with established diseases. Rinvoq (upadacitinib) is a daily pill for those with Crohn’s disease, an autoimmune disorder. Rinvoqwas the first oral treatment for Crohn’s disease to be approved. It was studied at ENCORE Borland Groover Clinical Research. Inpefa (sotagliflozin) has been approved as a daily pill to reduce cardiovascular death, hospitalization, and urgent heart failure by 33% in patients with heart failure. It was studied at the Jacksonville Center for Clinical Research. We at ENCORE Research Group are very excited about a year of amazing approvals. It validates the hard work and effort of all of our research staff and doctors, and – most importantly – it goes to show just how important our patient volunteers are! With the help of these heroes, we have new and effective options to help with six different diseases. Many thanks to everyone who has participated in any of our clinical trials, and we’ll see you next year!
References: Abbvie. (18 May, 2023). U.S. FDA Approves RINVOQ® (upadacitinib) as a Once-Daily Pill for Moderately to Severely Active Crohn’s Disease in Adults. https://news.abbvie.com/news/press-releases/us-fda-approves-rinvoq-upadacitinib-as-once-daily-pill-for-moderately-to-severely-active-crohns-disease-in-adults.htm Astellas. (13 May, 2023). Astellas’ VEOZAHTM (fezolinetant) Approved by U.S. FDA for Treatment of Vasomotor Symptoms Due to Menopause. https://www.astellas.com/en/system/files/news/2023-05/20230513_en_1.pdf GSK plc. (3 May, 2023). US FDA approves GSK’s Arexvy, the world’s first respiratory syncytial virus (RSV) vaccine for older adults. https://www.gsk.com/en-gb/media/press-releases/us-fda-approves-gsk-s-arexvy-the-world-s-first-respiratory-syncytial-virus-rsv-vaccine-for-older-adults/ Lexicon Pharmaceuticals. (26 May, 2023). Lexicon Announces FDA Approval of INPEFA™ (Sotagliflozin) for Treatment of Heart Failure. https://www.lexpharma.com/media-center/news/2023-05-26-lexicon-announces-fda-approval-of-inpefa-sotagliflozin-for-treatment-of-heart-failure Schneider, M., Narciso-Abraham, M., Hadl, S., McMahon, R., Toepfer, S., Fuchs, U., … & Wressnigg, N. (2023). Safety and immunogenicity of a single-shot live-attenuated chikungunya vaccine: a double-blind, multicentre, randomised, placebo-controlled, phase 3 trial. The Lancet. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)00641-4/fulltext Seres Therapeutics, Nestle Health Science. (26 April, 2023). Seres Therapeutics and Nestlé Health Science Announce FDA Approval of VOWST™ (fecal microbiota spores, live-brpk) for Prevention of Recurrence of C. difficile Infection in Adults Following Antibacterial Treatment for Recurrent CDI. https://www.nestlehealthscience.us/stories/seres-therapeutics-and-nestle-health-science-announce-fda-approval-vowst Velena SE. (10 November, 2023). Valneva Announces U.S. FDA Approval of World’s First Chikungunya Vaccine, IXCHIQ®. https://valneva.com/wp-content/uploads/2023/11/2023_11_10_BLA_Approval_PR_EN_Final_.pdf U.S. Food & Drug Administration. (27 November, 2023). 2023 Biological License Application Approvals. https://www.fda.gov/vaccines-blood-biologics/development-approval-process-cber/2023-biological-license-application-approvals U.S. Food & Drug Administration. (19 December, 2023). Novel Drug Approvals for 2023. https://www.fda.gov/drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products/novel-drug-approvals-2023
Scroll down to listen to this article.
Listen to the article here:
The holidays are a time for giving. We give gifts, hugs, support, unsolicited advice, and time. Of those, time can make the most significant difference to society at large if we provide it in the form of volunteering. Over 1 in 4 Americans volunteer their time. To count as volunteering, one has to freely choose to do the activity (no getting volun-told) and it should be altruistic. There are different categories of volunteering broken down into self-oriented and other-oriented. Self-oriented volunteering involves some kind of personal benefit, like potential career advancement. Other-oriented volunteering is instead focused on helping others in areas like health, education, religious groups, and youth development. Regardless of the category, any volunteering is good volunteering. Anyone who volunteers knows that besides helping others, it also gives you a warm fuzzy feeling inside, but did you know that fuzzy feeling might help keep you alive? Before we get into studies and possible health benefits, we must cover caveats. Studying the effects of volunteering on the body and brain is hard. You literally can’t force people to volunteer, so most of our information comes from observational studies. This is where researchers will follow people over time and compare those who volunteer to those who don’t. This can give us some great data, but it’s hard to know if volunteering is the cause or the effect. A senior citizen with a painful condition who works 60 hours a week will probably volunteer less than a healthy retiree (clinical research tries to mitigate these needs by providing compensation for time and travel to help make volunteering easier). Good studies therefore compare people with similar health, economic, and other factors in an attempt to isolate any effects volunteering has. With that in mind, volunteering seems to be associated with great outcomes. It appears to be associated with improvements in depression and life satisfaction. In a 14-year study of those above 60, a 2016 study found a reduced risk of cognitive decline due to volunteering. Most amazingly, a 2013 meta-analysis, which looked at the results of 40 other studies, found a 22% reduction in death! Even when taken with a McDonald’s french fry of salt, these results are very promising. But what’s going on to make this happen? There are no definite answers, but three suspected ones: How can we gain these benefits? By volunteering, of course! Food banks, schools, refugee services, and youth development programs can always use volunteers. The internet is a great place to look for opportunities to grow your social networks and help others. Clinical research is another great way to volunteer. One of the biggest draws for clinical research volunteers is knowing that the medicines they help research can help future generations. Today’s trials can help pave the way for medications and procedures that may persist into the future. This holiday season, if you can, volunteer and give the gift that keeps on giving. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: a meta-analytic review. PLoS medicine, 7(7), e1000316. https://doi.org/10.1371/journal.pmed.1000316 Infurna, F. J., Okun, M. A., & Grimm, K. J. (2016). Volunteering is associated with lower risk of cognitive impairment. Journal of the American Geriatrics Society, 64(11), 2263-2269. https://doi.org/10.1111/jgs.14398 Jenkinson, C. E., Dickens, A. P., Jones, K., Thompson-Coon, J., Taylor, R. S., Rogers, M., … & Richards, S. H. (2013). Is volunteering a public health intervention? A systematic review and meta-analysis of the health and survival of volunteers. BMC public health, 13(1), 1-10. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-773?TB_iframe=true Kwon, S. J., van Hoorn, J., Do, K. T., Burroughs, M., & Telzer, E. H. (2023). Neural representation of donating time and money. Journal of Neuroscience, 43(36), 6297-6305. https://doi.org/10.1523/JNEUROSCI.0480-23.2023 Webster, N. J., Ajrouch, K. J., & Antonucci, T. C. (2021). Volunteering and health: The role of social network change. Social Science & Medicine, 285, 114274. https://doi.org/10.1016/j.socscimed.2021.114274
Scroll down to listen to this article.
Listen to the article here:
Fats are necessary for survival. In the body, we call them lipids. They are needed to build the borders of our cells, create molecules and hormones, coat important neurons in the brain, protect and insulate our organs, store energy between meals, and perform many other vital functions. Lipids are fats, which don’t play well with water; think Spongebob and Squidward (or oil and water). Lipids need to be transported through the bloodstream by proteins. Lipids attach to these proteins to make lipoproteins (lipid + protein). Triglycerides are the most common type of lipid found in the body. They are used as energy for muscles and are stored in fat cells. They are transported in very low-density lipoproteins (VLDL), intermediate-density lipoproteins (IDL), and gut-produced chylomicrons. Cholesterols are needed for parts of our cells and are some of the building blocks of hormones, bile acids, and enzymes. Important types of cholesterol lipoproteins include low-density lipoproteins (LDL), high-density lipoproteins (HDL), and Lipoprotein(a) (Lp(a)). Our body stays healthy in part by maintaining a healthy balance of these lipids and lipoproteins. Keeping the balance of lipids is critical to our health. When it is out of whack, we experience dyslipidemia. Dys– meaning “bad,” lipid- indicating the lipids, or fats, and -emia meaning “presence in blood”. Dyslipidemia, or bad lipid presence in blood, is when the lipids in the blood are out of balance. This condition is unsettlingly common — one of every three American adults 20 years or older has dyslipidemia. Any imbalance falls under this description, but the most common and dangerous types in the USA are high LDL cholesterol, low HDL cholesterol, and high triglycerides. The prefix hyper- means “high,” so high cholesterol is called hypercholesterolemia (high cholesterol presence in blood); high triglycerides are hypertriglyceridemia (high triglyceride presence in blood); and a combination of both is simply called combined dyslipidemia. Some people suffer from hypolipidemia (low lipid presence in the blood), but it is much rarer in the USA. Because dyslipidemia is defined and diagnosed with a blood test, the underlying causes can vary, unlike conditions such as sickle cell anemia or chicken pox. Primary causes are genetic, where you inherit a risk factor. This might look like elevated Lp(a) levels, which are heavily influenced by genetics. Secondary causes are anything that may alter lipid levels, including diabetes, obesity, an unhealthy diet high in triglycerides, and lack of exercise. Regardless of the cause, the effects can be deadly. The biggest, most obvious problem is atherosclerotic cardiovascular disease (ASCVD), when cholesterols, fats, and other materials build up on the inside of our blood vessels. These buildups, called plaques, can block blood flow to the heart, brain, or other parts of the body, potentially causing heart attack, stroke, and/or pain in the body and limbs. With these outcomes in mind, solutions are critical. As with almost every non-infectious disease, some of the best methods for preventing complications are a healthy lifestyle. A diet high in vegetables, fruits, and whole grains may help. Keeping calorie counts low and moderate-to-vigorous exercise is also recommended, if possible. Beyond lifestyle, medications have helped many people. Statins like Lipitor are typically the first line of defense. They are the most widely prescribed class of drugs in the world, though not everyone can tolerate them. They inhibit an enzyme called HMG-CoA reductase. Statins can lower LDL levels by slowing the cholesterol-making process. PCSK9 is another important enzyme in the creation of cholesterol. PCSK9 inhibitors target this enzyme to help reduce cholesterol if statins aren’t working. Bempedoic acid and icosapent ethyl may also help reduce the amount of cholesterol the liver makes. Ezetimibe (uh·zeh·tuh·mibe) reduces the amount of cholesterol absorbed. Beyond lowering lipid levels, other medications may help reduce the risk of cardiovascular disease. Finally, if medications aren’t tolerated or effective enough, blood plasma can be removed, cleaned outside the body, and pumped back in using a process called plasmapheresis. Fats may be necessary for survival, but too many in the bloodstream can be deadly. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Berberich, A. J., & Hegele, R. A. (2022). A modern approach to dyslipidemia. Endocrine Reviews, 43(4), 611-653. https://academic.oup.com/edrv/article/43/4/611/6408399?login=true Feingold, K. R. (2015). Introduction to lipids and lipoproteins. https://www.ncbi.nlm.nih.gov/books/NBK305896/ Pappan, N., & Rehman, A. (2023). Dyslipidemia. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560891/ Pokhrel, B., Yuet, W. C., & Levine, S. N. (2017). PCSK9 inhibitors.https://www.ncbi.nlm.nih.gov/books/NBK448100/
Scroll down to listen to this article.
Listen to the article here:
Type 2 Diabetes is a worldwide growing pandemic. Globally, around 425 million people have type 2 diabetes; that’s more than the entire US population. Almost 10% of Americans have type 2 diabetes, which is characterized by the body’s inability to regulate blood sugar (glucose). Uncontrolled high blood glucose levels can have severe long-term effects, impacting the cardiovascular system, brain function, and overall mortality. Because of the increased dangers associated with diabetes, there are a myriad of medications that target this disease. Unfortunately, these can be difficult to adhere to and usually require a daily activity like a pill, blood strip testing, and/or exercise. The more intensive and difficult these steps are (for instance, taking three pills a day vs one), the less likely people will be able to follow through. Additionally, though the medications can effectively reduce blood sugar levels and the risk of complications, they do not target the underlying disease. Medications may need to be increased or changed if the disease progresses. So, what is the underlying disease profile? The big picture causes of type 2 diabetes include genetics, diet, exercise, and overall weight. Inside the body, these risk factors and habits manifest as cellular changes. The most significant change that takes place is called insulin resistance. Insulin is an important hormone that helps your body manage blood sugar; when cells are resistant to insulin, they can’t adequately respond to high blood sugar. This is the key indicator of type 2 diabetes. Many medications attempt to correct insulin resistance by replicating or replacing chemicals involved in the insulin pathway – including insulin itself in advanced cases. These have been a significant boon to many patients, but what if we could go deeper? One of the changes many people see is in the intestines. The part of the intestines connected to the stomach is called the duodenum. The duodenum is short but important. It regulates the release of hormones like glucagon-like peptide-1 (GLP-1) and gastric inhibitory peptide (GIP), both disrupted in insulin resistance. Scientists have found evidence that people with type 2 diabetes have increased duodenum tissue; a process called hypertrophy. Tissue removal in these patients may positively affect type 2 diabetes. One of the most successful therapies for type 2 diabetes is bariatric (weight loss) surgery that bypasses some or all of the duodenum. These surgeries have been shown to have an immediate and long-lasting effect on people with diabetes. Studies have found that A1C levels, which measure blood sugar, are completely back to normal range in patients who have had these surgeries at a rate five times higher than people on medication alone. It is thought that by bypassing or removing the duodenum, the hypertrophic cells stop interfering with the insulin process, and insulin resistance decreases or is outright reversed! Also, since surgery is a one-time deal, the adherence problems of pills and other daily activities are reduced or eliminated. Unfortunately, surgery is invasive, intensive, painful, and somewhat risky (10-20% have complications). Additionally, removing parts of the duodenum can result in malabsorption of nutrients. To solve this, researchers have devised a new investigative procedure for tackling type 2 diabetes. Instead of cutting the body open and removing, adding, or rearranging the intestinal tract, a new approach called the Revita system is being tested. This system revolves around a catheter that moves into the duodenum and ablates, or removes, the top layer of hypertrophic duodenum tissue. Early studies have shown that by targeting just the hypertrophic tissue, the duodenum will heal and retain its function while blood sugar normalizes. This is an exciting potential alternative to normal bariatric surgery for people with type 2 diabetes. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Cummings, D. E., Overduin, J., & Foster-Schubert, K. E. (2004). Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. The Journal of Clinical Endocrinology & Metabolism, 89(6), 2608-2615. https://academic.oup.com/jcem/article/89/6/2608/2870294 Jacobsen, S. H., Olesen, S. C., Dirksen, C., Jørgensen, N. B., Bojsen-Møller, K. N., Kielgast, U., … & Madsbad, S. (2012). Changes in gastrointestinal hormone responses, insulin sensitivity, and beta-cell function within 2 weeks after gastric bypass in non-diabetic subjects. Obesity surgery, 22, 1084-1096. https://link.springer.com/article/10.1007/s11695-012-0621-4 Rubino, F., Forgione, A., Cummings, D. E., Vix, M., Gnuli, D., Mingrone, G., … & Marescaux, J. (2006). The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Annals of surgery, 244(5), 741. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856597/ Rubino, F. (2008). Is type 2 diabetes an operable intestinal disease? A provocative yet reasonable hypothesis. Diabetes care, 31(Supplement_2), S290-S296. https://doi.org/10.2337/dc08-s271 Schauer, P. R., Bhatt, D. L., Kirwan, J. P., Wolski, K., Aminian, A., Brethauer, S. A., … & Kashyap, S. R. (2017). Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. New England Journal of Medicine, 376(7), 641-651. https://www.nejm.org/doi/full/10.1056/nejmoa1600869 Theodorakis, M. J., Carlson, O., Michopoulos, S., Doyle, M. E., Juhaszova, M., Petraki, K., & Egan, J. M. (2006). Human duodenal enteroendocrine cells: source of both incretin peptides, GLP-1 and GIP. American Journal of Physiology-Endocrinology and Metabolism, 290(3), E550-E559. https://journals.physiology.org/doi/full/10.1152/ajpendo.00326.2004 Wickremesekera, K., Miller, G., Naotunne, T. D., Knowles, G., & Stubbs, R. S. (2005). Loss of insulin resistance after Roux-en-Y gastric bypass surgery: a time course study. Obesity surgery, 15(4), 474-481. https://link.springer.com/article/10.1381/0960892053723402 van Baar, A. C., Holleman, F., Crenier, L., Haidry, R., Magee, C., Hopkins, D., … & Bergman, J. J. (2020). Endoscopic duodenal mucosal resurfacing for the treatment of type 2 diabetes mellitus: one year results from the first international, open-label, prospective, multicentre study. Gut, 69(2), 295-303. https://gut.bmj.com/content/69/2/295.abstract
Scroll down to listen to this article.
Listen to the article here:
This article was requested by an ENCORE community member. We do not currently have a study enrolling for this topic. The immune system is huge, complex, critical for life, and dangerous. It is good for us, protecting us by fighting infections and cancer; but there is a dark side: the inflammation it uses to fight can cause damage, it can overreact to cause autoimmune diseases, and its vigilance against invaders is what makes organ transplants difficult. The immune system is specialized in destroying cells and viruses. One of the most important features of the immune system is its ability to differentiate between cells we want and cells we don’t (including cancer cells!). However, when things go wrong, they can go very wrong. This may happen with autoimmune diseases like lupus or rheumatoid arthritis. Things may also go wrong when the immune system attacks transplanted organs; like a heart or liver. In these cases, we turn to immunosuppressant drugs. These do just what their name implies: they suppress the immune system. How they actually go about suppressing is very complicated, and requires a quick look at the immune system in general.
A very, VERY simplified version of the immune system and how it responds over time
The immune system can be divided into two major pieces, the innate and adaptive immune systems. There is overlap, as some cells have multiple functions. The innate immune system is made of cells that attack any invader they sense. These get activated immediately when we have infections or wounds and are like big, blunt weapons in their killing. The innate immune system includes monocytes, mast cells, macrophages, neutrophils, and eosinophils. These white blood cells ingest and eat perceived threats and cause inflammation. Inflammation helps bring in the complement system, a horde of mindless proteins that aim to attack invaders. If infections are not stopped immediately, dendritic cells activate the adaptive immune system. This is made up of T cells, B cells (including plasma cells), and antibodies. Throughout all this, cytokines like interferon and interleukin modify the immune system and are used for communication. Immunosuppressant drugs tend to target either the immune system at large or specific aspects of it, like T cells.
-mab Monoclonal antibody A quick guide to what the endings of some drugs mean
T cells are special cells that detect, remember, and fight against invaders. When they misidentify healthy cells as invaders, things get out of control quickly. Certain medications, like cyclosporin, tacrolimus, and voclosporin target the T cell’s ability to detect “dangerous” particles – like a transplanted organ. Others, such as Abatacept and Belatacept downregulate the ability of T cells to respond effectively. These tend to cause high blood pressure and associated problems. B cells are critical for producing deadly antibodies. They also act as memory cells to ensure future infections are dealt with quickly. The two ways to deal with wayward B cells are by destroying them or limiting their ability to differentiate. Rituximab, ocrelizumab, ofatumumab, and veltuzumab target B cells for destruction, while bortezomib targets specialized plasma cells that spew antibodies at a rate of 2000 per second. By lowering the number of B cells they cause less autoimmune damage. Targeting B cell differentiation limits their functionality with medications like belimumab and atacicept, but comes at the expense of reducing some cell signals and possible pneumonia. Free-floating proteins are critically important to the immune system. The complement system is composed of quintillions (!!!) of tiny proteins that act autonomously to hamper invaders. Eculizumab targets a specific protein that helps activate the destructive powers of the complement system. Cytokines are different but equally important proteins. They are the communication particles used by the immune system. Corticosteroids are broad immunosuppressant anti-inflammatory drugs. They reduce the activity of the immune system, slow fluid flow that causes inflammation, interfere with cytokines, and inhibit immune cell production. They can be effective, but the effects are not specific to the immune system and can cause problems with “virtually every system in the body” (Barshes, 2004). Major side effects include bone problems like osteoporosis, skin changes, obesity, diabetes, and neurologic changes. Advanced medications like basiliximab, anikara, and rilonacept target only specific cytokines, with hopefully reduced side effects that may be flu-like. Finally, two medication classes reduce B and T cell counts through unique mechanisms. Polyclonal antibody immune globulins are additional antibodies that are given at high doses. These seem to overwhelm the immune system, depleting white blood cell counts and keeping it from attacking itself. These are potent but come with severe side effects that feel like getting sick: hives, fever, headaches, and even heart attacks. Alemtuzumab is a medication that targets proteins found outside B and T cells and targets them for death. This has the expected side effects of fever, nausea, etc. Each class of medication targets a different part of the immune system. This means some may be more useful in some situations, and some may not work at all in some instances. Please note that all medications should be discussed with a medical professional who is aware of your unique medical history; don’t make medical choices based on an internet article! Further, we’ve mentioned some of the bigger, or more general side effects of these medications, but each has many more that should be considered before use. We’ve also left off the most important side effect of all: these suppress the immune system! Patients on these medications are more prone to infection, cancers, and dangerous particles in the body. They are dangerous and should not be taken lightly. Instead, prudence demands that taking an immunosuppressant medication be weighed against the alternative. In the case of a critical organ transplant, like a heart, it’s a no-brainer. Each situation is unique and should be discussed with your medical team. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Barshes, N. R., Goodpastor, S. E., & Goss, J. A. (2004). Pharmacologic immunosuppression. Front Biosci, 9(1-3), 411-420. https://doi.org/10.2741/1249 Claeys, E., & Vermeire, K. (2019). Immunosuppressive drugs in organ transplantation to prevent allograft rejection: Mode of action and side effects. Journal of immunological sciences, 3(4). https://immunologyresearchjournal.com/articles/immunosuppressive-drugs-in-organ-transplantation-to-prevent-allograft-rejection-mode-of-action-and-side-effects.pdf Dettmer, P. (2021). Immune: A journey into the mysterious system that keeps you alive. Random House. Nicholson, L. B. (2016). The immune system. Essays in biochemistry, 60(3), 275-301. https://portlandpress.com/essaysbiochem/article/60/3/275/78223/The-immune-system Wiseman, A. C. (2016). Immunosuppressive medications. Clinical journal of the American Society of Nephrology: CJASN, 11(2), 332. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4741049/
Scroll down to listen to this article.
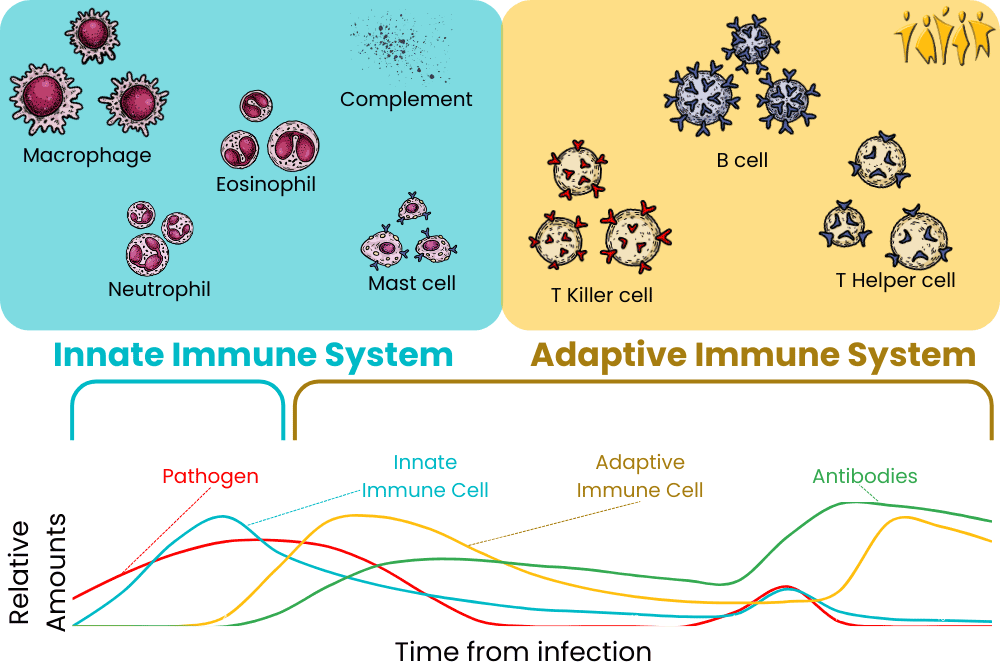
-cept Targets receptor molecules
-mib Inhibits protein breakdown mechanismsListen to the article here:
Low back pain affects some 60-90% of people at some point in their lives. Most cases resolve within a few months, but sometimes, a more sinister condition lies underneath. When the cause of pain is nerve root irritation, the condition is called lumbosacral radiculopathy. Lumbosacral describes where this pain occurs: in the lumbar (lumbo- lower back) and –sacral (back of the hip) area. This is part of the spinal cord and contains the nerves that control and sense pain in the hips and legs. Radiculopathy describes the problem. Radiculo- comes from the Greek radix, indicating the root of the nerve. Pathy is from the Greek patheia and means suffering or pain. Together, it is clear what lumbosacral radiculopathy is: lower back pain originating from a nerve root. Though low back pain is common, lumbosacral radiculopathy affects only around 3-5% of the population. It is more common in males, but occupation plays a bigger role than sex.
Lumbosacral radiculopathy is defined through the presentation of pain and where it is located. This presentation is usually back pain but may radiate into the legs. People describe the pain as electric, burning, and/or sharp. Untreated, it can affect sleep, mood, and your ability to function. In general, the nerve root is aggravated through either compression or inflammation, but the underlying causes are diverse. Degenerative spine conditions, including disc herniation, spondylolisthesis, and spinal stenosis, cause lumbosacral radiculopathy when nerves are physically crushed or pinched by parts of the spinal column. Injury and tumors can also cause parts of the nerve to be pinched. Alternatively, the nerve root can become inflamed from infection, vascular conditions, and injury. Before we move into treatments, it is important to understand how nerves work. A nerve is a cell or group of cells called neurons that communicate information through electricity. Individual cells gather information from one end and fire an “action potential.” This is an electrical and physical event. Cells open special holes called ion channels that let charged particles (usually sodium and calcium) into the cell. Some ion channels are activated by mechanical stress, proteins, and chemical neurotransmitters, but many are activated by electricity! When enough charged ions cross the channels, other electricity-dependent ion channels start rapidly opening, letting in a rush of charged particles and causing the whole cell to “fire.” At the distant end of the neuron, chemical neurotransmitters are released, and the signal can move to other cells.
An illustration of a neuron opening ion channels and firing an action potential
Treatments for lumbosacral radiculopathy vary widely but can be grouped into conservative (non-surgical) and surgical. Initial conservative treatments include exercises, education, and NSAID anti-inflammatory medications like ibuprofen. More intensive therapies may consist of antidepressants and anticonvulsants, which modify how the neurons communicate. Other than injected steroids, these are all systemic treatments, meaning they affect the whole body and can come with a host of side effects. Surgical therapy options are invasive and can come with risks as well as pain. The “gold standard” surgery is a laminectomy with discectomy, where parts of the vertebrae and disc are removed. This has been shown to be safe, but improvements to symptoms and function – especially in the long term – are dubious. The goal in most lumbosacral radiculopathy cases is to stay with conservative treatments as long as possible. Luckily, scientists are always on the prowl for new treatments. Remember the ion channels? It turns out not all ion channels are created equal. One type of ion channel, NaV 1.8, transports the common ion sodium. This channel is only found in peripheral pain neurons – like those that may be aggravated in lumbosacral radiculopathy. This ion channel has been shown to be necessary for pain neurons to fire their action potential. Medications that can shut down this ion channel may be able to relieve the symptoms of lumbosacral radiculopathy, hopefully without wide-ranging side effects. Ridiculous as it sounds, relief for lumbosacral radiculopathy may be near. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Alexander, C. E., & Varacallo, M. (2017). Lumbosacral radiculopathy. https://europepmc.org/article/nbk/nbk430837 Berry, J. A., Elia, C., Saini, H. S., & Miulli, D. E. (2019). A review of lumbar radiculopathy, diagnosis, and treatment. Cureus, 11(10). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6858271/ Clark, R., Weber, R. P., & Kahwati, L. (2020). Surgical management of lumbar radiculopathy: a systematic review. Journal of general internal medicine, 35, 855-864. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7080952/ Hsu, P. S., Armon, C., & Levin, K. (2017). Acute lumbosacral radiculopathy: Pathophysiology, clinical features, and diagnosis. Waltham, MA: UpToDate Inc. https://www.ncbi.nlm.nih.gov/books/NBK430837/ Kuijer, P. P. F., Verbeek, J. H., Seidler, A., Ellegast, R., Hulshof, C. T., Frings-Dresen, M. H., & Van der Molen, H. F. (2018). Work-relatedness of lumbosacral radiculopathy syndrome: review and dose-response meta-analysis. Neurology, 91(12), 558-564. https://doi.org/10.1212/01.wnl.0000544322.26939.09 Renganathan, M., Cummins, T. R., & Waxman, S. G. (2001). Contribution of Nav1. 8 sodium channels to action potential electrogenesis in DRG neurons. Journal of neurophysiology, 86(2), 629-640.https://journals.physiology.org/doi/full/10.1152/jn.2001.86.2.629
Scroll down to listen to this article.
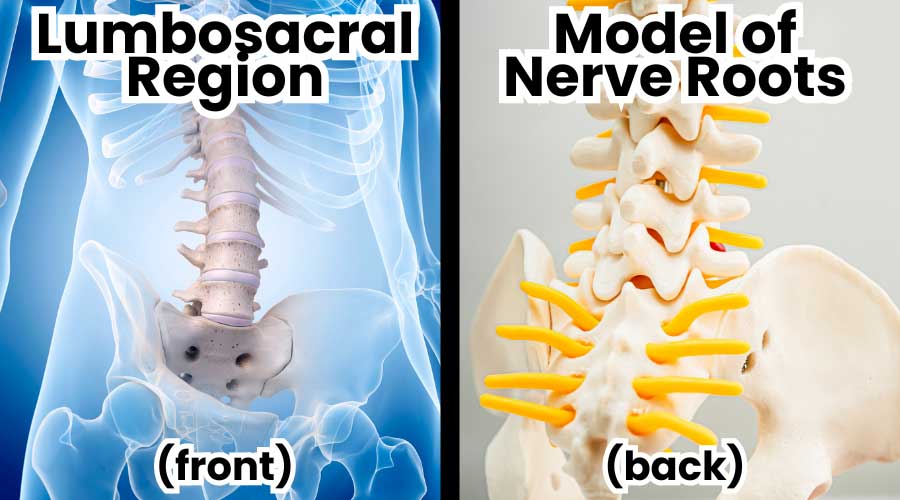
Listen to the article here:
Previously, we explored how the character trait of gratitude can have long-lasting impacts on our health and well-being. Unfortunately, character traits are internal and can be hard to change. Thankfully, scientists are a creative lot and have been working for decades attempting to find out how to increase gratitude. Note that the following methods are still experimental; positive results have been found, but the sample sizes have been relatively small. These interventions have shown increased psychological well-being in the form of increased happiness and satisfaction, as well as fewer depressive symptoms in adults. Please note that this is not a substitute for professional psychological or medical help! Instead, these are interventions that may have positive effects when adhered to. The interventions are: Gratitude journaling, Gratitude letters, Mental subtraction, and Experiential consumption. Gratitude journaling is easy and effective; you just write down things you are thankful for. Various methods have been studied, including the amount (3-5 things) and the frequency (daily or weekly) of journaling. The most effective method I’ve seen is to write three things you are grateful for that happened on the same day. Generally, people wrote a sentence or two about each event. Keeping it limited to daily events helps keep this task from becoming stale. In addition, writing the causes of those events seems to help make the results long-lasting. In one study, a week of gratitude journaling led to increased measures of happiness for the next six months. The idea behind gratitude journaling is that by focusing on the positives, we reinforce those mental pathways and make it more likely that we think about positive things. Gratitude letters are a little more intense than gratitude journaling. In this task, participants write a letter to someone who has been particularly kind to them but hasn’t been properly thanked before. Ideally, the letter should be hand-delivered for maximum effect. By showing gratitude to others, participants had higher scores associated with gratitude themselves. This one is a particularly tactile activity, which may be helpful to some. The effects of this intervention were shown to last over a month on average. Mental subtraction is an interesting intervention. In this activity, participants imagined and wrote about a positive event that occurred in their lives and what their lives would be like had the event never taken place. Alternatively, participants were asked to describe how a positive event was surprising to them, forcing them to think of ways it may not have occurred. This was shown to have positive effects on people’s mental state. By looking at the ways things may not have occurred, it might make people more grateful that they occurred at all. Experiential consumption is an interesting “intervention.” When looking at habits of what people buy, scientists have found that spending money on experiences (trips, music events, etc.) seems to increase people’s happiness and gratitude more than buying tangible items (furniture, clothes, etc.).The thinking behind why experiences may be beneficial is that they are more personal and intrinsic. Experiences are less likely to be compared to others, more likely to be incorporated into who you are, and more likely to be social. Material items are easy to compare to others and unlikely to make lasting impacts on how you see yourself. In addition, ownership is defined as exclusive use, making it an inherently antisocial state. These methods of increasing our gratitude may not be the end-all of increasing our happiness, but they are a good start. We have a few tips to increase the success rate of these interventions. First, a desire for self-improvement helps a lot. If you want to be more thankful this season, it will make each of these tasks easier. Second, expectations matter. The benefits of these interventions may not change your life, but they are pretty sure to improve how you feel about it; plus, they are basically no-risk (unless your experiential consumption is skydiving). Finally, it is easier to follow through on engaging activities. Things like writing the causes of a thankful event may help keep things engaging and fun, making you more likely to complete the task. Feel free to modify these as needed to keep yourself engaged and having fun with them. Hopefully, these ideas help increase your gratitude this Thanksgiving season. Thank you, as always, for reading! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Allen, S. (2018). The science of gratitude (pp. 1217948920-1544632649). Conshohocken, PA: John Templeton Foundation. https://ggsc.berkeley.edu/images/uploads/GGSC-JTF_White_Paper-Gratitude-FINAL.pdf Dickens, L. R. (2017). Using gratitude to promote positive change: A series of meta-analyses investigating the effectiveness of gratitude interventions. Basic and Applied Social Psychology, 39(4), 193-208. https://www.tandfonline.com/doi/full/10.1080/01973533.2017.1323638 Enmons, R. A., & McCullough, M. E. (2003). Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality and Social Psychology, 84(2), 377-389. Geraghty, A. W., Wood, A. M., & Hyland, M. E. (2010). Attrition from self-directed interventions: Investigating the relationship between psychological predictors, intervention content and dropout from a body dissatisfaction intervention. Social science & medicine, 71(1), 30-37. https://doi.org/10.1016/j.socscimed.2010.03.007 Kaczmarek, L. D., Kashdan, T. B., Kleiman, E. M., Baczkowski, B., Enko, J., Siebers, A., … & Baran, B. (2013). Who self-initiates gratitude interventions in daily life? An examination of intentions, curiosity, depressive symptoms, and life satisfaction. Personality and Individual Differences, 55(7), 805-810. https://doi.org/10.1016/j.paid.2013.06.013 Koo, M., Algoe, S. B., Wilson, T. D., & Gilbert, D. T. (2008). It’s a wonderful life: Mentally subtracting positive events improves people’s affective states, contrary to their affective forecasts. Journal of personality and social psychology, 95(5), 1217. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2746912/ Renshaw, T. L., & Olinger Steeves, R. M. (2016). What good is gratitude in youth and schools? A systematic review and meta‐analysis of correlates and intervention outcomes. Psychology in the Schools, 53(3), 286-305. https://onlinelibrary.wiley.com/doi/10.1002/pits.21903 Seligman, M. E., Steen, T. A., Park, N., & Peterson, C. (2005). Positive psychology progress: empirical validation of interventions. American psychologist, 60(5), 410. https://doi.org/10.1037/0003-066X.60.5.410 Walker, J., Kumar, A., & Gilovich, T. (2016). Cultivating gratitude and giving through experiential consumption. Emotion, 16(8), 1126. https://doi.org/10.1037/emo0000242
Scroll down to listen to this article.
Listen to the article here:
Clinical research has many benefits. There are the obvious ones, like a stipend for time and travel and the potential benefits of an investigational medication, but also more esoteric benefits, like increased quality of care, attention from medical staff, and knowledge about the conditions people face. We recently had a chance to talk with one of our repeat patients, Brendle, who will walk us through her clinical research experience and why she keeps signing up for more studies. “I’ve learned so much,” she stated. One of the big benefits of clinical research is the knowledge gained through experience. Brendle said “Dr. Koren explains things so well.” Not only do patients get access to podcasts from Dr. Michael Koren and articles from our knowledgeable staff, but they also get a lot of direct face-to-face time with medical professionals and support staff. Transparency is key in clinical research, so we spend a lot of time talking through the full medical history of every patient. We also make sure everyone understands the science, risks, benefits, and process of a trial before enrolling. We typically schedule an hour or two for patients to talk through medical history, medications, and the specifics of a clinical trial before enrolling. Compare this to a typical doctor’s visit with a wait time of 15-30 minutes and only 10-20 minutes of time with a doctor and it’s easy to see why people like Brendle enjoy the clinical trial experience so much. Imagine how many complications could be avoided if primary care practices were able to spend an hour with each patient before prescribing a new medication! Of course, medications and procedures are the major benefit most people think of when it comes to clinical research. Participants rank risks and benefits as the most important information before participating. The importance of understanding the potential risks of investigational medications or procedures should not be taken lightly. We ensure that patients are given the information needed to make well-informed decisions. Obviously, potential benefits are different in every study. Registry studies only collect information, and the benefit is in drug development down the road (and compensation). Phase 3 studies, in contrast, can have long-lasting effects on biological markers of health. Brendle notes, “when I first came here, my Ejection Fraction (EF) was only 10%. Now it’s up!” This information is exactly what we want to know for statistical analysis, but the real-world consequences can be even better. Brendle continues, “I could only go from the bed to the couch and back, but now I can do much more.” Amazingly, it’s possible that benefits like this may be realized even when a patient is given a placebo. Not only is the placebo effect real, but the increased attention from doctors and medical staff makes sure we catch any health changes as soon as they happen. Brendle finished up her chat with us saying “This is the best experience. I am thankful to get into studies.” We are very thankful for patients like Brendle – and you, dear reader – who help push science forward by volunteering for clinical trials! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Business Wire, (March 22, 2018). 9th annual vitals wait time report released https://www.businesswire.com/news/home/20180322005683/en/9th-Annual-Vitals-Wait-Time-Report-Released CISCRP, (2021). Perceptions and insights study 2021. https://www.ciscrp.org/services/research-services/perceptions-and-insights-study/ Tai‐Seale, M., McGuire, T. G., & Zhang, W. (2007). Time allocation in primary care office visits. Health services research, 42(5), 1871-1894. https://doi.org/10.1111%2Fj.1475-6773.2006.00689.x
Scroll down to listen to this article.
Listen to the article here:
The long-dead philosopher Cicero once said, “There is no quality I would rather have, and be thought to have, than gratitude. For it is not only the greatest virtue, but is the mother of all the rest.” Gratitude is when we are thankful and appreciate kindness, people, and the world around us. It goes beyond a quick emotion. When we get a thoughtful or meaningful gift, it makes us happy, but that feeling may only stay with us short term. The long-term nature of gratitude is what makes it powerful. Simple appreciation can change into a general mood, and with enough gratitude, our personality can change (hopefully for the better). If we live a life choosing gratitude, we feel happy when we get gifts, but also at smaller things. The long-term personality trait associated with gratitude can increase positive emotions, leave us satisfied, and may help decrease envy, anxiety, and depression. Persistent personality traits are a neat thing. They affect our mood and emotional response to everyday things. Gratitude as a personality trait increases the intensity (amplitude) and duration of positive thankful emotions and makes it easier to feel thankful. It also increases the number of other people you feel thankful for (like being appreciative that your sister’s cousin’s best friend’s thrash metal band got a record deal). This happens because personality traits indicate that the brain has specific structures and wiring paths built over time. With gratitude, we can see that these changes are in a few key areas of the brain: those responsible for social bonding, perspective-taking, moral judgment and decision-making, and the reward system. They aren’t just emotional areas; they include intentional and calculated parts of the brain that help change our overall outlook. Overall, brain areas increased by gratitude are prosocial; they promote good social behaviors like friendship. Being thankful is great for making friends and feeling good, but it may also have health benefits! Psychological effects include increased positive emotions, satisfaction, and spirituality as well as decreased indicators of depression, anxiety, and envy. Gratitude-filled people also tend to be more empathetic, forgiving, helpful, and supportive. This makes sense; recognizing good things focuses our attention on more good things. Thankfully, gratitude may also affect our physical health! Measuring gratitude is difficult, so take the following with a grain of salt. Beneficial biomarkers of health measured by people with high gratitude include improved inflammation, diastolic blood pressure, heart rate, and A1C (blood sugar). These are associated with some pretty serious conditions like asthma, cardiovascular disease, and the effects of diabetes. It is unclear how feeling thankful can cause all of these changes, but it may be due to eating and sleeping habits. Gratitude has been linked with lowering dysfunctional eating habits and with improving sleep quality. A good diet is always important, but a good night’s sleep may be even more important for gratitude. So this November, let’s all be thankful for the ability to feel thankful! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Allen, S. (2018). The science of gratitude (pp. 1217948920-1544632649). Conshohocken, PA: John Templeton Foundation. https://ggsc.berkeley.edu/images/uploads/GGSC-JTF_White_Paper-Gratitude-FINAL.pdf Boggiss, A. L., Consedine, N. S., Brenton-Peters, J. M., Hofman, P. L., & Serlachius, A. S. (2020). A systematic review of gratitude interventions: Effects on physical health and health behaviors. Journal of Psychosomatic Research, 135, 110165. https://doi.org/10.1016/j.jpsychores.2020.110165 McCullough, M. E., Emmons, R. A., & Tsang, J. A. (2002). The grateful disposition: a conceptual and empirical topography. Journal of personality and social psychology, 82(1), 112. https://psycnet.apa.org/doi/10.1037/0022-3514.82.1.112
Scroll down to listen to this article.
Listen to the article here:
Boo! This Halloween many of us will dress as spooky things, visit houses with creepy decorations, go into haunted houses, watch scary movies, and enjoy other horror-related entertainment. But being scared kinda sucks. Why do many of us actively subject ourselves to being scared on purpose? One of the big draws of scary things is dichotomy: the contrast between two ideas that can’t both be true. When we watch a scary movie, we are safe in a theater, but feel the danger and emotion as if we were ourselves being chased by a shark with a knife (or whatever). In a haunted house we may get an even more visceral experience, as our neighbor jumps out at us with a rubber knife in his realistic shark costume. Knowing we are safe makes our brains bounce back and forth between danger and safety. Another big pull of Halloween scares is that they rely on expectations. Most of us would be pretty upset to come home and find a giant spider and some skeletons on our bed. But when given the proper context and expectation, we can be excited and find scary decorations fun and exciting. Fear is the major emotion at play here, but what is fear? Our emotions can be roughly divided along two lines: valence and amplitude. Valence describes the positive or negative quality of an emotion and amplitude is how strong the emotion is felt. In this organization scheme, fear has a negative valence and a high amplitude, it makes us feel bad and we feel it strongly. On top of this, amplitude seems a little more persistent than valence, so there is a delay period where we still feel excited but can change from a negative to positive valence. So fear with the right context (such as a haunted house or scary movie) makes us switch between the negative valence of fear and the logical knowledge that we are safe. We can look inside the brain to get a better understanding of what’s happening. There are two competing pathways that activate with fear, depending on the distance to danger. The midbrain pathway activates for close, immediate threats. It is the “fight or flight” response to fear. The frontal cortex is for threats that are further away and is in charge of planning and strategizing. With spooky halloween fears, these two systems are in direct opposition. Trying to overcome the midbrain pathway is hard, but rewarding. We are also rewarded when successfully surviving a scary situation. When we conquer our fear we have the high amplitude of fear combined with the positive valence of relief. So this Halloween, indulge in a little emotional hijacking and enjoy your fear a little bit! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Anders, S., Lotze, M., Erb, M., Grodd, W., & Birbaumer, N. (2004). Brain activity underlying emotional valence and arousal: A response‐related fMRI study. Human brain mapping, 23(4), 200-209. Dewey, J. (1894). “The theory of emotion: I: Emotional attitudes”. The Psychological Review. 1(6), 553–569. https://doi.org/10.1037/h0069054 Nummenmaa, L. (2021). Psychology and neurobiology of horror movies. PsyArXiv. https://doi.org/10.31234/osf.io/b8tgs
Scroll down to listen to this article.
Listen to the article here:
It was the best of me, it was the worst of me. There are two versions of your dear author: the one who loves cookies, pizza, and video games and the one who loves surfing, cycling, and roasted vegetables. In a stroke of complete luck, I live at the beach where exercise and healthy living are trendy and encouraged. That wasn’t always the case, however. When I was younger, I went to college in Indiana. There was no beach, I had no bike, everyone had a computer, and my meal plan included unlimited pizza. Unsurprisingly, these two versions of myself have very different health outcomes. One lifestyle is associated with heart attacks, diabetes, and obesity, while the other isn’t. Which version makes it through to the end isn’t just determined by self-discipline and genetics but heavily by the community you are in. Things that contribute to your health outcomes are called determinants of health. These include your genetics, behavior, and medical care, but also the physical place you spend time and social factors. The determinants of health aren’t insulated; they interact and influence each other. That last one is properly termed Social Determinants of Health (SDOH). These are the daily interactions with people and the area around you, but also the bigger systems that influence these interactions. Examples of the social determinants of health include: It was easy to see these social determinants at work during the pandemic. The “Quarantine 15” was a real phenomenon where somewhere around 48% of people in America gained weight. People were stressed, jobs and income were unstable, healthcare access was limited, exercise options dropped, and – importantly – many of us lost our community connections. Luckily, with the pandemic calming down, we are presented with opportunities to shore up our social determinants of health. With the pandemic as a reference, we can see that social determinants of health are subject to very big forces. To improve the social determinants of health in our area, we would ideally look at inequality, structural biases, macroeconomic conditions, and government policy. On the personal level, the most productive changes we can make (other than moving halfway across the country) are at the community level. This includes your family, friends, neighbors, and people you interact with and share common ground with, such as those in a book club or church. From a healthcare perspective, “community” determines who you talk to when sick, who checks in on you, who cooks food when you have a newborn, who takes you to the doctor when you can’t drive, and so on. Luckily, your community can expand. When you join a clinical trial at one of our ENCORE Research Group sites, you don’t just gain access to cutting-edge research, you gain a community that is committed to health. We partner with other groups, perform community outreach, and write extremely well-written, clever, and funny articles for your inbox weekly. On top of this, when enrolled in a clinical trial, we need to monitor your health and stay in touch. We look for what will help your specific situation and if you miss an appointment we reach out to make sure you are ok. ENCORE stands for Encouraging COmmunity Research and Education, it’s right there in our name! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Khubchandani, J., Price, J. H., Sharma, S., Wiblishauser, M. J., & Webb, F. J. (2022). COVID-19 pandemic and weight gain in American adults: A nationwide population-based study. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 16(1), 102392. https://doi.org/10.1016%2Fj.dsx.2022.102392 Artiga, S., & Hinton, E. (2018). Beyond health care: the role of social determinants in promoting health and health equity. Kaiser Family Foundation, 10. https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ Baciu, A., Negussie, Y., Geller, A., Weinstein, J. N., & National Academies of Sciences, Engineering, and Medicine. (2017). The Role of Communities in Promoting Health Equity. In Communities in Action: Pathways to Health Equity. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK425849/ Centers for Disease Control and Prevention. (8 December, 2022). Social determinants of health at CDC. U.S. Department of Health & Human Services. https://www.cdc.gov/about/sdoh/index.html
Scroll down to listen to this article.
With contributions from Stacey Lowey-Ball, BA AnthropologyListen to the article here:
The eyes are the windows to the soul. But what happens when those windows don’t get properly cleaned? They might get scratchy, stingy, blurry, and discolored. Dry eye disease is when tears don’t adequately lubricate the eye. Symptoms include scratchy burning or stinging in the eyes, red eyes, sensitivity to light, and blurry vision. This disease affects 5%-30% of the world population and is more common in women and those above 50 years old. Dry eye is a multifactorial disease, meaning multiple things may have a hand in causing it. To understand what might be going wrong, we first have to understand a little about how the eye works.
The eye is lubricated by a 3-layered film called the tear film on the outside. That’s tear like near, not tear like hair. The layers, from inner to outer, are the mucus layer, aqueous (water) layer, and lipid (oil) layer. These aren’t hard, distinct layers, but each has a separate purpose. The mucus layer is secreted by goblet cells located on the surface of the eye and lubricates it. The aqueous (water) layer is secreted by the lacrimal gland and keeps everything clean. It is susceptible to evaporation, which is where the lipid (oil) layer plays a part. The lipid layer is oily, which resists evaporation and is secreted by meibomian glands on the edge of the eyeball. Together, these layers act like a crew of window washers to keep the eye lubricated and clean. Don’t let all the vocabulary make you googly-eyed: the lacrimal gland, goblet cells, and meibomian glands just produce different types of eye fluids. They work together to produce the tear film, but they don’t work alone. The brain receives moisture signals from the eye and sends signals to the glands to keep the eye moist. The eyelids spread the tear film and help prevent evaporation. Finally, the surface of the eye itself needs to be clean and healthy. Together, these components make up the lacrimal functional unit. Disruptions to this system are the cause of dry eye disorder. Problems can be divided into broad categories, but each can overlap and lead to problems with other parts of the lacrimal functional unit.
Problems can originate in the nerves to and from the brain. These can become inflamed or attacked by immune cells such as with Sjogren’s syndrome. When the nerves from the brain to the lacrimal gland are disturbed, tear production might be reduced. When the sensory nerves from the eye to the brain are disrupted, the brain doesn’t know to tell the lacrimal glands to secrete tears and keep the tear film intact. Nerve response can also be disrupted permanently by long-term contact lens use and temporarily by laser surgery. The cells of the eye itself can also be damaged. Epithelial (surface) cells need to interface smoothly with the tear film. The aqueous (water) layer can be deficient – you may not produce enough tears. This can be due to inflammation and autoimmune problems (as above), obstructed glands, nerve damage, and more. Medicines like antihistamines, beta-blockers, and diuretics can also reduce the aqueous layer. Allergies can cause dry eye, so the fact that antihistamines can cause it too is deeply eye-ronic. Finally, tears may evaporate too quickly. This is called tear instability or evaporative dry eye and is usually due to a problem with the oil layer. Other evaporative problems include eyelid problems, gland dysfunction, decreased blinking, vitamin A / omega-3 deficiency, and environmental problems (like wind and smoke). To help with dry eye we can look at three methods: environmental, surgical, and medical. Environmental relief can be found by avoiding dry, dusty, and smoky air while ensuring you get enough vitamin A and Omega-3. Surgical blocking of the drainage tear duct can keep moisture on the eye surface longer. Medical solutions include different types of eye drops. Some mimic tears, and some deliver medicine. For severe and chronic problems, there are two major medications: cyclosporine and nerve growth factor (NGF). Cyclosporine is an immunosuppressive drug that can relieve inflammation in the nerves and glands. Nerve growth factor is an amazing medical category that can regenerate damaged nerve fibers and can heal surface epithelial cells. With new clinical trials on the horizon, we can peer through the window to new relief for dry eyes! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Lemp, M. A., & Foulks, G. N. (2007). The definition and classification of dry eye disease. Ocul Surf, 5(2), 75-92. Mantelli, F., Massaro‐Giordano, M., Macchi, I., Lambiase, A., & Bonini, S. (2013). The cellular mechanisms of dry eye: from pathogenesis to treatment. Journal of cellular physiology, 228(12), 2253-2256. https://onlinelibrary.wiley.com/doi/pdf/10.1002/jcp.24398 National Eye Institute. (April 8, 2022). Dry Eye. National Institute of Health https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/dry-eye
Scroll down to listen to this article.
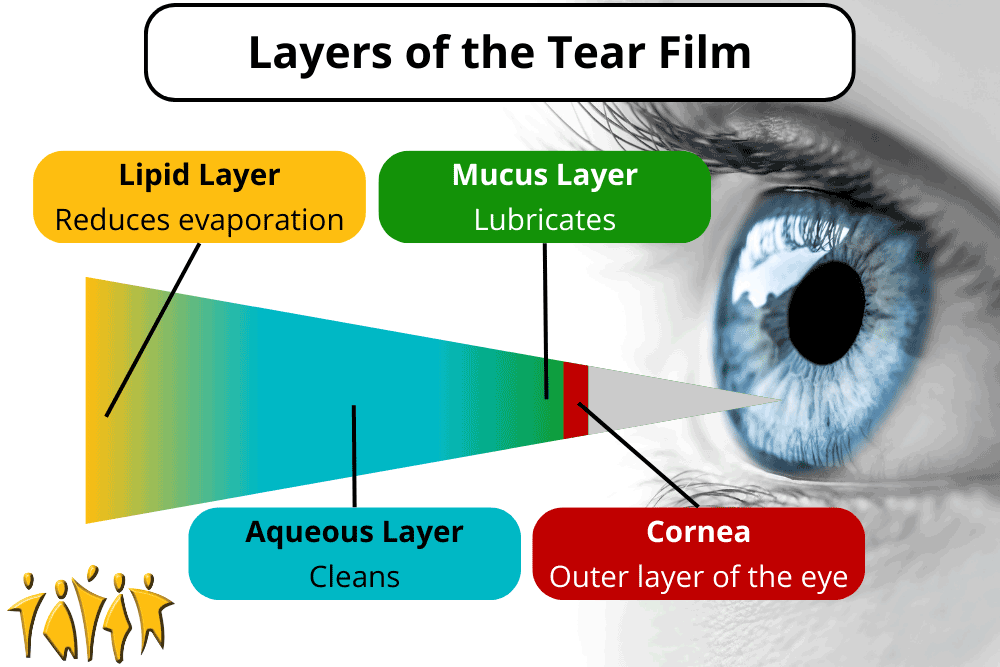
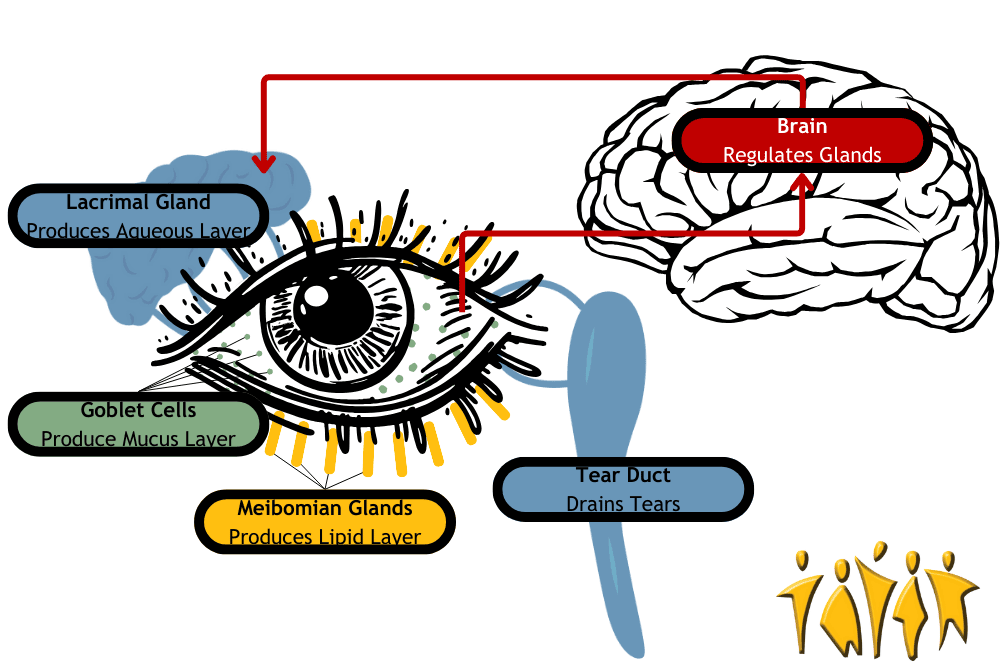
Listen to the article here:
Electricity is essential for most modern-day activities. We use it for lights, air conditioning, and watching cat videos. We also use it to keep our hearts beating. Electricity coordinates the heart and causes it to contract into its familiar wub-dub. Why do we need electricity in the heart, and what can we do when the zips don’t zap properly? Shockingly, we’ll start with a broad overview. The heart is an organ made of several billion cells. These are organized into many structures, including chambers. There are two small upper chambers called atria, which is the plural word for the left atrium and right atrium. There are also two large lower chambers called ventricles, which are again separated into left and right. The set on the left pumps fresh, oxygenated blood from the lungs to all the cells in the body. The set on the right pumps deoxygenated blood to the lungs to get more oxygen. It is a little strange to describe the heart only as a series of chambers, as the actual structure of the heart is a giant, very strong, coiled muscle. In order for muscles to contract and produce power, electricity is needed. Electricity tells the muscles they need to move. In most of the body, the electrical signals for muscles to contract are delivered by the brain. The heart is a little different. The heart is involuntary, meaning we have no direct control over when it beats. We can send signals to the heart by breathing deeply or jumping, but the electrical signal that tells the heart to beat comes from within the heart itself. Near the top is a collection of cells called the sinoatrial (SA) node. Here resides a group of cells called pacemaker cells. These cells produce a small electrical zippy zappy signal around once per second. This signal rapidly amplifies and spreads throughout the atria, causing them to contract. This spreading comes out like a wave, which allows all the atrial muscle cells to contract in a big, coordinated manner. Soon after, the signal travels through the atrioventricular (AV) node into the ventricles, propagating outward. This takes a fraction of a second, so we hear wub-dub instead of just one big beat. This also gives blood time to travel from the atria to the ventricles, ensuring it goes correctly. This system is pretty amazing, but it’s not foolproof. Many things can go wrong. The electrical signal might be disrupted, the heart might be too slow, or it might beat at a bizarre rhythm. When this happens, the heart pumps less efficiently than it needs to, and sometimes can’t pump enough blood for oxygen to get around the body. Unlike a heart attack, where heart cells die immediately, electrical problems can often be alleviated. When the electricity in our heart doesn’t behave correctly, we can put in artificial electricity. When the heart’s pacemaker cells aren’t successfully sending coordinated signals to the whole heart, an artificial cardiac pacemaker (often just called a pacemaker) can be implanted. Temporary pacemakers may sit outside the body, but permanent ones are installed inside our body cavities. These are made of materials our bodies don’t find threatening, like titanium. They can be attached to the heart through wires called leads, mounted on the heart surface, or inside the heart muscle. Each patient will have electrical problems in specific areas; maybe the pacemaker cells aren’t working properly, or maybe electricity can’t travel to the ventricles, or maybe it can’t cross from the left to the right side. Because of this, pacemakers can attach to either an atrium, a ventricle, or to both ventricles. Because the electrical problems are so varied, artificial pacemakers have many different patterns for firing. Artificial pacemakers don’t just cause beating; they also detect it. Little electrodes can tell when the heart has fired, and internal circuitry can measure this against when the cardiologist thinks a beat should have happened. Most will detect when a shock is needed and fire on demand, but some fire all the time. Pacemakers can respond to changes in heart rate, can sense abnormal rhythms, and have special modes for things like surgery. On top of all of this, medical professionals can often remotely monitor artificial pacemakers and adjust the pacemaker’s programming without surgery! This can be used to make sure heart rhythms stay ideal, but can also help alleviate the side effects of artificial pacemakers, which include chest pain, dizziness, fatigue, and shortness of breath. Pacemakers are amazing wonders of the modern era. As time goes on, scientists are developing new and more specific programs to zap the heart without zapping our fun. It’s nice to know that when you watch a video of a funny cat falling off the dresser, electricity makes your heart happy inside and out. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Buckberg, G. D., Nanda, N. C., Nguyen, C., & Kocica, M. J. (2018). What is the heart? Anatomy, function, pathophysiology, and misconceptions. Journal of cardiovascular development and disease, 5(2), 33. https://www.mdpi.com/2308-3425/5/2/33 Lak, H. M., & Goyal, A. (2020). Pacemaker types and selection. https://www.ncbi.nlm.nih.gov/books/NBK556011/ Sundnes, J., Lines, G. T., Cai, X., Nielsen, B. F., Mardal, K. A., & Tveito, A. (2007). Computing the electrical activity in the heart (Vol. 1). Springer Science & Business Media.
Scroll down to listen to this article.
Listen to the article here:
You may have heard the news; earlier this month an FDA committee unanimously concluded that phenylephrine, a common decongestant, doesn’t work. What does this mean? Why is it still on shelves? Is it poison? Should I throw my medicine away? Is the FDA a scam!? What’s the point of science if they change the rules?!? We’ll address the last two questions first. Good science is a process of change. It’s not definitive; just our best, evidence-based guess at how to predict what will happen given current best experimentation and data. As we get more data of better quality the conclusions drawn by scientists change. To be clear, when scientists update their conclusions this is good and means science is working. It means we are getting more accurate information through better practices and updated information. New technology plays a big part in this. Think of it like maps. The first explorer to document an area may have a hand-drawn map outlining the major features. Later cartographers may come along and refine the map, making it more accurate and filling in the details. Their map may show a landmark in a different, more accurate position. This doesn’t mean the original mapmaker was malicious, or that maps don’t work, but instead that we can update our information to have a more accurate view of the world. Back to the issue at hand, let’s find out what we’ve learned. On September 11th and 12th, 2023, the Non-prescription Drug Advisory Committee reviewed the results of several clinical studies which looked into the effectiveness of oral phenylephrine at lowering nasal congestion (stuffy nose). These studies measured symptoms in hundreds of patients who took phenylephrine and/or a placebo sugar pill in controlled environments. These studies found, by and large, that the decongestant was not significantly better than the placebo at providing relief. It should be noted that in the studies, most patients found relief from both phenylephrine and the placebo! It should also be noted that participants had few or no adverse reactions to the studies, though some had headaches. In response, the committee concluded that phenylephrine is not effective at providing relief when compared with a placebo; the drug doesn’t work. So what does this mean for me? First, note that this is an advisory committee. They provide independent advice to the FDA, but do not make policy. In the near term nothing has changed. The FDA will likely take a while to make any policy changes and may have public input. Additionally, the clinical trials did not find the medication dangerous, just ineffective. This means phenylephrine isn’t dangerous at the recommended doses; you don’t need to throw it away (unless it’s expired!). It also means that a phase-out period will probably be slow, because there isn’t a danger to the public beyond wasting money on a medicine that works no better than a placebo. Finally, how did this happen? How did a medication that doesn’t work get past the FDA? The answer is that while oral phenylephrine doesn’t seem to provide relief, inhaled phenylephrine continues to show effectiveness! When the oral form was approved in the 1970s, scientists thought around 30% of the medication would be absorbed in the gut. It has come to light that around 1% of the decongestant medication is actually available for our body to use when taken orally. From this, it follows that we would need to take much higher doses to get significant relief, which comes with increased side effects – including to the heart! On top of this is the completely fascinating finding in 2015 that placebos are getting better. A meta-study of several placebo-controlled clinical trials found that the effects of medications stayed the same, but the effect of placebos has been increasing over time! Some scientists believe this may be because we expect medications to do more, so the placebo is more effective! This means that when clinical trials are repeated, medications have a more difficult time showing effectiveness versus placebo. Think of our map-makers. That same landmark may have been perfectly mapped by cartographers, but tectonic plates can still cause it to slowly shift position. Lucky for us this means that new medicines brought to market are virtually guaranteed to be more effective than if they were introduced last century! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Division of Nonprescription Drugs 1 (DNPD1), Division of Inflammation and Immune Pharmacology (DIIP), Office of Clinical Pharmacology (OCP), Division of Epidemiology II (DEPI-II). (September 11, 2023). Efficacy of Oral Phenylephrine as a Nasal Decongestant. U.S. Food & Drug Administration. https://www.fda.gov/media/171915/download U.S. Food & Drug Administration. (September 14, 2023). FDA clarifies results of recent advisory committee meeting on oral phenylephrine. U.S. Food & Drug Administration. https://www.fda.gov/drugs/drug-safety-and-availability/fda-clarifies-results-recent-advisory-committee-meeting-oral-phenylephrine Meltzer, E. O., Ratner, P. H., & McGraw, T. (2015). Oral phenylephrine HCl for nasal congestion in seasonal allergic rhinitis: a randomized, open-label, placebo-controlled study. The Journal of Allergy and Clinical Immunology: In Practice, 3(5), 702-708. https://pubmed.ncbi.nlm.nih.gov/26143019/ Meltzer, E. O., Ratner, P. H., & McGraw, T. (2016). Phenylephrine hydrochloride modified-release tablets for nasal congestion: a randomized, placebo-controlled trial in allergic rhinitis patients. Annals of Allergy, Asthma & Immunology, 116(1), 66-71. https://doi.org/10.1016/j.anai.2015.10.022 National Library of Medicine. (March 3, 2011). Safety Study Comparing Phenylephrine HCL Extended Release Tablets 30 mg and Placebo (Study CL2007-07)(P07529)(COMPLETED). U.S. Department of Health and Human Services.ClinicalTrials.gov ID NCT00874120. https://clinicaltrials.gov/study/NCT00874120?tab=results Tuttle, A. H., Tohyama, S., Ramsay, T., Kimmelman, J., Schweinhardt, P., Bennett, G. J., & Mogil, J. S. (2015). Increasing placebo responses over time in US clinical trials of neuropathic pain. Pain, 156(12), 2616-2626. https://doi.org/10.1097/j.pain.0000000000000333
Scroll down to listen to this article.
Listen to the article here:
Though it’s still warm and beautiful out, winter looms on the horizon. Winter in Florida can be good: a time for family, biking and outdoor exercise, bigger waves for surfing, and tasty foods. Winter can also be bad: a time for cold, wetsuits, fruitcakes, and the flu. So what is the flu, how does it work, and why does it take after my extended family and only visit us in the cooler months? The seasonal flu is caused by the flu virus, properly called Influenza, and more properly a type of orthomyxoviridae (there will be a test at the end). There are three categories of influenza viruses that infect humans, conveniently named influenza A, B, and C. These are distinct from each other in some critical ways, one being how easily they change the proteins on the outside of the virus. Viruses are tiny little packets of DNA or RNA that are contained in a little pouch. The pouch has special proteins called antigens on the outside that help it invade target cells. The proteins are also one of the key ways our immune system detects and fights these viruses. Influenza A changes these rapidly, influenza B changes slowly, and influenza C is stable, undergoing little or no change over time. Influenza A and B viruses undergo a process called antigenic drift. This is when the surface proteins change a little bit at a time. The changes can cause incremental “improvements” to the virus, allowing it to evade our immune system and infect cells more easily. These changes are fast enough that over the course of a year your body may not be able to recognize the virus and you may get the flu year after year, but slow enough that you probably won’t get it twice in the same season – especially with a vaccine. Influenza A can also undergo antigenic shift, which is like the antigenic drift on overdrive. This is like when your dad shaves his beard for the first time in 20 years: same thing underneath but different enough you have trouble recognizing him. When this happens your body can’t recognize the virus as dangerous and previous antibodies and vaccines provide little or no aid. Because of this Influenza A has been responsible for all flu pandemics.
Why is it seasonal though? Well, it’s not seasonal everywhere. In some tropical and subtropical areas, the flu follows the rainy season and comes twice a year. In some tropical areas the flu is present year-round. This provides a clue; it’s the weather! Strangely, it might actually be our response to changing weather that is the progenitor of a flu season. Influenza viruses spread through the air. This is bad news for us in that they spread easily from person to person, but also means they are affected by the weather more than things that may be spread by fluids or insects. Temperature and relative humidity are the two biggest factors. Cool, dry air gives influenza viruses a better chance for infecting us. The virus is more stable in droplets, more of them are shed, and the droplets might stay in the air longer as they evaporate. Our defensive capabilities are decreased in the cold – anyone with a dry throat can attest to this. The protective mucus layer in our airway is decreased and the innate immune system isn’t as efficient. To make things worse, in the winter we spend more time indoors. In the industrialized world, including America, we spend almost no time outdoors. A 2001 study found that we spend around 87% of our time in buildings and 6% in cars. This varies heavily by where you work, but most of us spend almost our whole lives in buildings with recirculated, conditioned air. In the winter, heated air is drier, which promotes influenza virus stability. As we walk into and out of buildings our throats are dry and inefficient at removing viral particles. This creates ideal conditions for Influenza to infect and spread during the winter. So what can we do? Get vaccinated of course! Every year scientists work hard to produce vaccines that will target the most likely versions of influenza to emerge during the winter. Antigenic drift is taken into account and vaccines will (hopefully) protect against the likely minor antigenic changes between production of the vaccine and emergence of flu season. New mRNA vaccines shorten the time between production and deployment of vaccines based on the current dominant strain, increasing their effectiveness. All flu vaccines available in the USA are quadrivalent, meaning they protect against two strains of influenza A and two strains of influenza B. So don’t forget to get a flu vaccine, spend time with the family, and go outside! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). (12 December, 2022). How flu viruses can change: “drift” and “shift”. U.S. Department of Health & Human Services. https://www.cdc.gov/flu/about/viruses/change.htm Couch, R. B. (1996). Orthomyxoviruses. Medical Microbiology. 4th edition. https://www.ncbi.nlm.nih.gov/books/NBK8611/ Klepeis, N. E., Nelson, W. C., Ott, W. R., Robinson, J. P., Tsang, A. M., Switzer, P., … & Engelmann, W. H. (2001). The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. Journal of Exposure Science & Environmental Epidemiology, 11(3), 231-252. https://www.nature.com/articles/7500165 Lowen, A. C., & Steel, J. (2014). Roles of humidity and temperature in shaping influenza seasonality. Journal of virology, 88(14), 7692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4097773 Moriyama, M., Hugentobler, W. J., & Iwasaki, A. (2020). Seasonality of respiratory viral infections. Annual review of virology, 7, 83-101. https://www.annualreviews.org/doi/10.1146/annurev-virology-012420-022445
Scroll down to listen to this article.
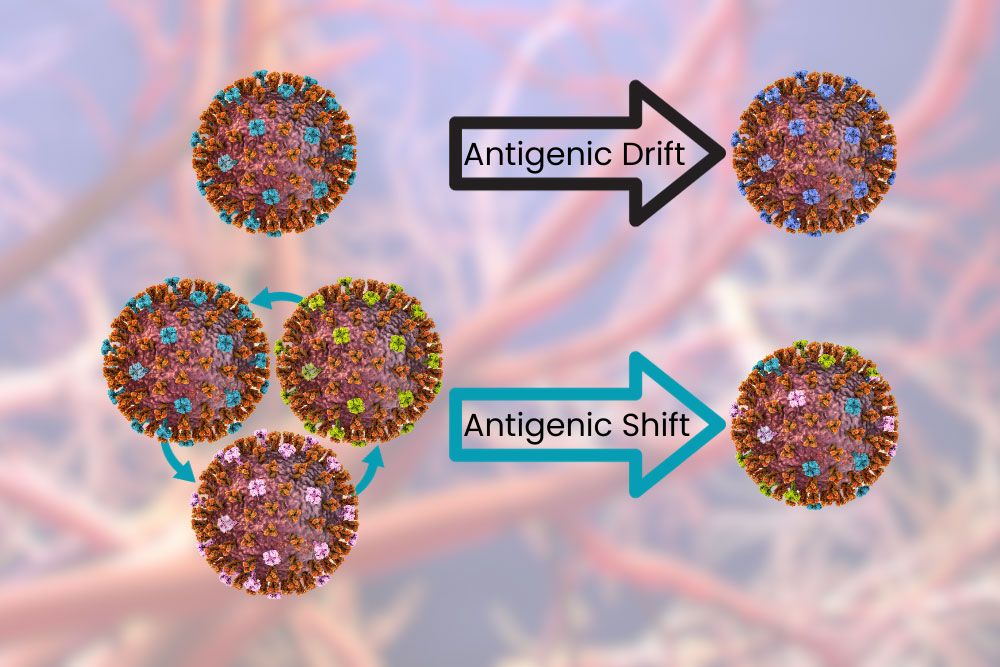
Listen to the article here:
I recently went to a dessert party. That’s a party where everyone brings a dessert. I, naturally, arrived with cookies while others brought cakes and pies. Surprisingly, there was one attendee who presented a bowl of berries, another who showcased a sweet potato casserole, and a third who simply brought avocado with a dash of salt. Do these all count as desserts? What is a dessert? A word that was clear at the outset was quickly confusing in how broad it was. Unfortunately, that confusion can also happen with medical terms. Take cardiovascular disease. It’s got something to do with the heart, but sometimes it includes strokes in the brain. So what is cardiovascular disease? “Cardiovascular” is a word made of two component parts: cardio- means “heart” and vascular indicates blood vessels. Together, cardiovascular disease is that which affects the heart and/or blood vessels. The heart and blood vessels carry oxygen to the cells and keep them alive. Since we’re made of cells, keeping them alive is pretty important. Therefore, the heart and blood vessels are also quite important, and cardiovascular disease can be dangerous if not managed. Cardiovascular disease is more common than apple pie in the United States. Data from the CDC show that nearly HALF of adults over 20 have some form of cardiovascular disease. With a prevalence that high, it’s no surprise that cardiovascular disease is the leading cause of death in America and around the world. Unfortunately, as noted above, the exact definition of “cardiovascular disease” is very broad. In researching this article you are currently reading, I consulted the World Health Organization, the American Heart Association, and the National Institute of Health (part of the CDC). These organizations listed the various diseases included in cardiovascular disease, and only agreed on two conditions: Other diseases that at least two agreed on include: Though all these diseases may seem different, they are all part of the same system. Narrow blood vessels to the heart or brain cause oxygen loss. This narrowing can be caused by plaque formed when cholesterol lodges in the vessel wall. If some of this plaque dislodges, it can lead to heart attacks and strokes. Irregular heartbeats and heart attacks can lower the amount of blood (and oxygen!) delivered around the body. Hypertension stresses the whole system and can lead to heart attack, stroke, and damage to other organs like the kidneys. Additionally, they may have similar risk factors, outcomes, and treatments. There is a genetic component to cardiovascular disease. This is evident with congenital heart defects, which occur during development. It is also evident looking at who is at risk of developing cardiovascular disease. African Americans are at the highest risk, while people who identify as Hispanic have the lowest risk. Big modifiable risks include cholesterol, smoking, and hypertension (which is itself a form of cardiovascular disease!). Other risks include diabetes, being overweight, poor diet, low exercise, alcohol consumption, and low sleep. Research is ongoing into the cycle of mental health and cardiovascular disease as well. Mood and anxiety disorders, PTSD, and chronic stress can cause direct damage to the cardiovascular system while simultaneously increasing behaviors that compound the danger, including smoking and failing to take medicines. Lowering the modifiable risks above is, unsurprisingly, one of the best ways to fight cardiovascular disease. Managing cholesterol, blood pressure, and diabetes can help. Cutting smoking and lowering alcohol intake can make a big difference. Getting help with mental health (and getting a good night’s sleep) may help your heart relax as well. Maintaining a healthy weight through a good diet and dynamic exercise is vital. Unfortunately, without management, cardiovascular disease is more like a desert than a dessert: it can kill you. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Centers for Disease Control and Prevention. (July 19, 2021). Coronary artery disease (CAD). U.S. Department of Health and Human Services. https://www.cdc.gov/heartdisease/coronary_ad.htm National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. (May 15, 2023). About heart disease. U.S. Department of Health and Human Services. https://www.cdc.gov/heartdisease/about.htm American Heart Association. (May 31, 2017). What is cardiovascular disease? https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Alonso, A., Beaton, A. Z., Bittencourt, M. S., … & American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2022). Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation, 145(8), e153-e639. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001123 National Heart, Lung, and Blood Institute. (n.d). Heart and vascular diseases. U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov/science/heart-and-vascular-diseases Accessed on September 12, 2023. The World Health Organization. (June 11, 2021). Cardiovascular diseases (CVD). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Scroll down to listen to this article.
Listen to the article here:
What happens when the things that are supposed to keep us safe turn against us? In fiction, this is usually posed as some big, world-ending problem like artificial intelligence going off the rails and killing everybody. In nonfiction, this question is hashed out in the world of autoimmune diseases. Systemic Lupus Erythematosus (SLE) is an autoimmune disease that typifies an entire cluster of autoimmune diseases , known as “lupus-associated”. These include rheumatoid arthritis, systemic sclerosis (scleroderma), Sjogren’s syndrome, and more. These diseases tend to spread though different parts of the body, which is why many have “systemic” in the name. Systemic lupus erythematosus is a chronic and progressive autoimmune disease. Chronic indicates that it is long-lasting, and progressive means that the disease can change over time, usually by getting stronger and more severe. It is much more prevalent in racial and ethnic minorities, and 90% of sufferers are women. These statistics immediately give us clues as to the nature of SLE and autoimmune diseases: they have a genetic component. People from different parts of the world have different packages of genes, but why are women so susceptible? Genes are part of our DNA, the code that describes what we are. Specifically, they are sections of code that describe how to build a protein. Each gene has instructions for a single protein, and changes to the genetic code can result in changes to the protein that it’s supposed to build. Genes aren’t randomly distributed in the DNA code; they are located on chromosomes. We have 23 chromosomes that we get from our mother and 23 from our father. Most are the same size, but the X and Y sex chromosomes look different. The X chromosome, attributed to females, contains 800-900 genes while the Y chromosome, attributed to males, contains only 50-60 genes! It is thought that a genetic component of autoimmune diseases may be found on the X chromosome. The immune system is made of cells that have specific proteins they use to identify invaders, send alert signals, and attack. A huge class of signaling molecules is called hormones. Many of these are proteins. One class of immune hormone proteins is interleukins. When there are too many of these, they are in the wrong place, or they have changed in some way the immune system can go haywire and attack healthy cells. Autoimmune diseases like SLE are complex. The immune system gets out of whack due to multiple conditions acting together. Affected people have a genetic predisposition: their DNA has code that makes it likely to produce dangerous levels or types of interleukins. This isn’t a foregone conclusion, however. An environmental stimulus is needed to start the autoimmune process. This can be airborne particles like silica or cigarette smoke, drugs including contraceptives, viruses, and even sunlight! When the genetic primer is lit, the immune system misidentifies what is good and bad and can explode on healthy cells. Like many autoimmune diseases, SLE has a cycle of remission and relapse; people have symptom-free periods, and periods of increased symptom activity. Symptoms may be low on the disease scale, including pain, fatigue, and a rash on the face. This rash may be exacerbated by UV light, appearing on the nose and cheeks where we get sun. This takes on the classic “butterfly rash” shape associated with SLE. Higher on the disease scale is damage to organs like the kidneys, heart, lungs, bloodstream, gut, and nervous system. When it is widespread it can also cause skin and joint disease, including arthritis. Severe cases can lead to hospitalization and death. So what can we do about autoimmune diseases like SLE? Each patient is different, each disease is different, and doctors have to balance the effects of medications against side effects. In general, the most obvious preventative step for autoimmune diseases is something that calms the immune system down. Antimalarials like hydroxychloroquine decrease immune activity and are often a preventative step. During flare-ups, a targeted anti-inflammatory like a glucocorticoid may be used. If these fail, doctors may prescribe immunosuppressant drugs or monoclonal antibodies. Specific organ maintenance, like treating liver and kidney problems can help alleviate damage, and doctors can also recommend procedures that work directly on our bloodstream. The future may hold promise for new medications that target specific parts of the autoimmune disease pathway. Keep your eyes open for new clinical trials aimed at helping those with autoimmune diseases like SLE. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Ameer, M. A., Chaudhry, H., Mushtaq, J., Khan, O. S., Babar, M., Hashim, T., … & Khan, O. S. (2022). An overview of systemic lupus erythematosus (SLE) pathogenesis, classification, and management. Cureus, 14(10). https://doi.org/10.7759/cureus.30330 Angum, F., Khan, T., Kaler, J., Siddiqui, L., & Hussain, A. (2020). The prevalence of autoimmune disorders in women: a narrative review. Cureus, 12(5). https://doi.org/10.7759/cureus.8094 Barber, M. R., Drenkard, C., Falasinnu, T., Hoi, A., Mak, A., Kow, N. Y., … & Ramsey-Goldman, R. (2021). Global epidemiology of systemic lupus erythematosus. Nature Reviews Rheumatology, 17(9), 515-532. https://doi.org/10.1038/s41584-021-00668-1 Mackay, I. R. (2009). Clustering and commonalities among autoimmune diseases. Journal of autoimmunity, 33(3-4), 170-177. https://doi.org/10.1016/j.jaut.2009.09.006
Scroll down to listen to this article.
Listen to the article here:
I remember learning in biology that we’re made out of cells. That’s true, but not all the way true. We’re also made out of the stuff in between cells This stuff is called the extracellular matrix. Extracellular means outside of the cells and matrix in this context means the environment that is occupied. Though the extracellular matrix isn’t a dystopian cyberworld made by robots, it can be dangerous if parts of it start getting out of control. Systemic sclerosis, a type of scleroderma, is a disease that results in excess material being deposited in the extracellular matrix, causing body-wide problems. Systemic sclerosis is a rare, chronic, and progressive autoimmune disease. It affects women in their 60s, though men and African Americans have the worst outcomes from the disease. Around one in four people with systemic sclerosis also have another autoimmune disease. The biggest risk factor for systemic sclerosis is family history; and genetics. It is thought that some people have a genetic predisposition to the disease and that environmental factors cause it to “kick on.” As an autoimmune disease, systemic sclerosis is complex. It may present differently in each patient who has it. One of the easiest ways to differentiate types is by how it affects skin. Sclerosis comes from Greek and means to harden or a tumor. Systemic sclerosis is hard, tumor-like skin that affects the whole body (or system). There are three categories based on how widespread the condition is. Systemic Sclerosis sine scleroderma is when skin is unaffected, though fingers may experience discoloration. Limited cutaneous systemic sclerosis is, as the name suggests, limited. The skin on the fingers and face is affected. It tends to progress slower and may be less dangerous. Diffuse cutaneous systemic sclerosis is quite the opposite. It is diffuse, meaning it spreads far and wide. It may affect the arms and legs up to knees and elbows, the chest, stomach area, and back. It progresses quickly and is associated with poorer outcomes. Beyond the hardening of the skin, there are other symptoms, and (unsurprisingly) none are great. Patients may experience: All of these can be annoying and painful, but many are very dangerous. Systemic sclerosis, in fact, is the most deadly of all rheumatic diseases. Let’s dig into how systemic sclerosis works to find out why. As stated before, systemic sclerosis is an autoimmune disease. Some environmental factors like smoke, alcohol, viruses, solvents, or chemicals activate our epithelial cells. Epithelial cells interact with the outside world and are located on the skin, in our lungs and digestive tract, and around organs. The cells send out danger signals in the form of cytokines. There are several cytokines, but one of the most prevalent in this system is type 1 interferon (IFN). If this were The Matrix these guys would be the Agents, good at getting rid of unwanted intruders but dangerous when they get out of control. They are usually sent out in viral infections and put the immune system into a general state of alert. When there are too many cytokines, they start causing damage that needs to be repaired. The body responds to high IFN in a couple of ways: alerting immune cells, starting inflammation, and – in people with systemic sclerosis, by activating fibroblasts. Fibroblasts make the connective tissue between cells (you may see where this is going). These guys go into overdrive and spew extra collagen, elastin, and other connective tissues between cells. They try to repair damage from the cytokines, but the excess tissue signals problems and creates a deadly feedback loop. When this is bad enough, normal cells are replaced by this dense tissue in the extracellular matrix. The skin on the fingers and toes thickens, and the vascular (circulatory) system starts getting crushed. Small blood vessels called capillaries die. The tissue around your vital organs thickens and causes damage. The body can’t deliver enough oxygen to organs, which is bad. If this happens to the blood vessels of the lungs, it’s even worse. The thickening on the fingers, toes, arms, legs, and face may be debilitating, but the real danger is what’s happening inside. So what can be done? Doctors can try to treat the symptoms and complications to keep people comfortable. They may treat vascular, skin, kidney, arthritic, and gastrointestinal problems. If the lungs are affected, specific monoclonal antibodies may be prescribed. Some patients also find that general immunosuppressors help, but these can come with myriad side effects. The best bet for patients is to discover and treat systemic sclerosis early, before damage spreads, if possible. Medications may slow the decline, possibly until the disease becomes stable. On the horizon, clinical researchers are looking at medications that may cut the feedback loop and help patients break free from the matrix. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Harrison, D. G., Coffman, T. M., & Wilcox, C. S. (2021). Pathophysiology of hypertension: the mosaic theory and beyond. Circulation research, 128(7), 847-863. https://doi.org/10.1161/CIRCRESAHA.121.318082 Myat, A., Redwood, S. R., Qureshi, A. C., Spertus, J. A., & Williams, B. (2012). Resistant hypertension. Bmj, 345. https://doi.org/10.1136/bmj.e7473 Sarafidis, P. A., Georgianos, P., & Bakris, G. L. (2013). Resistant hypertension—its identification and epidemiology. Nature Reviews Nephrology, 9(1), 51-58. https://www.nature.com/articles/nrneph.2012.260
Scroll down to listen to this article.
Listen to the article here:
What do Star Wars, Nazi-occupied France, and surge protectors have in common? We root for the resistance to win! But what if the resistance is evil and bad? Meet resistant hypertension. This little devil is a special, particularly damning form of hypertension that resists medications. Not just one or two medications, either! Resistant hypertension avoids at least three separate medications of three separate types (called classes)! Resistant hypertension is when blood pressure remains over 140/90 mmHg while seated, even when the patient is taking the maximum tolerated dose of three or more different classes of hypertension medications. It can damage the heart, eyes, and kidneys and lead to heart attack, stroke, end-stage renal disease, and death. It can be caused by a narrowing of the veins, but the prevalence isn’t narrow at all. It affects 6-9 million Americans, with the highest incidence in Black males. A few conditions are associated with resistant hypertension, including diabetes, obesity, and chronic kidney disease. To understand how this disease works, we must first understand how blood pressure works. Blood pressure is controlled by three main components: heart rate, volume pumped, and blood vessel size. This may seem like a simple system, but each of these three components are affected by a myriad of body systems. Think of it like trying to maintain peace in the middle east. It might seem like you could balance the needs of religion, economics, tradition, and foreign influence, but it turns out: no. Other big actors in the blood pressure realm include the brain and kidneys. The brain directs other organs how to act and the kidneys regulate the fluid in the bloodstream (which we call blood). On top of these big organs, blood pressure is affected by interconnected systems, genes, inflammation, salt, even the bacteria in our gut! One of the biggest systems involved with blood pressure is the Renin-Angiotensin-Aldosterone System, or RAAS (or RAS). This system involves the kidneys and uses hormones to regulate blood pressure. It relies on a few key hormones and enzymes, and is also affected by other systems like the natriuretic peptide system and the brain. In hypertension, one or more of these systems no longer functions properly. We have four major classes of medication to help get the body back on track. Long-acting calcium channel blockers (CCB) reduce the amount that the heart and arteries can contract, relaxing the system. Angiotensin is a hormone that causes blood vessels to narrow. Angiotensin-converting enzyme inhibitors (ACEI) block angiotensin from being made and angiotensin receptor blockers (ARB) block it from acting on blood vessels. Finally, diuretic medications remove water and salt from the blood, lowering the volume of fluid that the heart pumps. Each of these medications targets the body in slightly different ways. Different medications work better for some people, and side effects may present differently. A good doctor will look for a blood pressure medication (or two (or three (or more))) that brings blood pressure to healthy levels without too many side effects. When we do not achieve healthy blood pressure levels even at the maximum tolerated dose of three or more medications we have resistant hypertension. Patients with resistant hypertension are at a higher risk of major cardiac events because they can’t get blood pressure under control with available medications. Prolonged high blood pressure leads to damage throughout the cardiovascular system. So what can be done? The best first step is to lower modifiable risks. This is actually a good first step for literally anything that is dangerous. Weight loss is a good opening move if you are obese. Lowering alcohol and salt intake may help. Talking to a doctor about any medications or conditions that may be raising blood pressure is important. Finally, clinical trials may be underway to look for specialty medications that target those with resistant hypertension. Hopefully we can find a way to crush resistance without succumbing to the dark side of the force (or becoming nazis). Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Harrison, D. G., Coffman, T. M., & Wilcox, C. S. (2021). Pathophysiology of hypertension: the mosaic theory and beyond. Circulation research, 128(7), 847-863. https://doi.org/10.1161/CIRCRESAHA.121.318082 Myat, A., Redwood, S. R., Qureshi, A. C., Spertus, J. A., & Williams, B. (2012). Resistant hypertension. Bmj, 345. https://doi.org/10.1136/bmj.e7473 Sarafidis, P. A., Georgianos, P., & Bakris, G. L. (2013). Resistant hypertension—its identification and epidemiology. Nature Reviews Nephrology, 9(1), 51-58. https://www.nature.com/articles/nrneph.2012.260
Listen to the article here:
Most of us have experienced standing up and feeling a little light-headed. This is caused by gravity pulling blood into the legs, causing the brain to run a teensy bit dry. Within a few seconds, the vessels in the legs tighten and push blood out, and the heart pumps it up to the brain so we can forget where we left our glasses. For some people, it’s not quite as simple – or as harmless. Between 500 thousand and 3 million Americans, mostly women between 15 and 50 years of age, suffer from Postural Orthostatic Tachycardia Syndrome, or POTS. Postural means it relates to your position. Orthostatic comes from the Greek for “upright” and “to stand.” Tachy- means fast, and -cardia refers to the heart; together, tachycardia means the heart is beating excessively fast. Syndrome actually means a group of symptoms happening together, which is an important part of POTS. Together, Postural Orthostatic Tachycardia Syndrome (POTS) is an abnormal increase in high heart rate when standing up from a lying position. POTS has two aspects that occur together: tachycardia when standing and orthostatic intolerance. Tachycardia is a very high heart rate. With POTS, this is defined as 30 beats per minute (BPM) more than normal (40 in children) or a BPM of 120 or more. Orthostatic intolerance means the patient can’t stay upright without experiencing symptoms. Symptoms include: As alluded to earlier, POTS occurs because of gravity. When we stand up, around 2 cups (500mL) of blood falls into our lower body, and we must push and pull it back out. Baroreceptors in the cardiovascular system detect the change in blood pressure and kick the autonomic nervous system (which does things automatically) into action. The brain rapidly sends signals to redistribute blood (especially to get more blood up to the brain!) Blood vessels push out blood. They constrict, squeezing blood out and providing less space to pool up. The heart pulls blood up. If not enough blood is coming up, it beats faster to try to help. With POTS, the autonomic system breaks down somewhere, and the heart starts beating out of control to try to help. POTS is a syndrome, not a disease. This is significant because syndromes like POTS can have many causes and can be hard to precisely parse into perfunctory pieces. Any part of the system described above can be out of whack and potentially cause POTS. The brain might not receive proper signals or might not send signals in a helpful way. Our ability to squeeze blood vessels might be compromised. We might have hormone imbalances, sensitivities, or changes. The amount of blood or salt in the body might be too low. Some people find their blood pressure decreases slightly with POTS, but some find that their blood pressure increases! Conditions that can cause these differences vary widely. Small vessel muscles can weaken, pregnancy, surgery, and trauma may cause POTS, and autoimmune or infectious diseases can affect things. Genetics, diabetes, and poisoning from alcohol, heavy metals, or chemotherapy may also be implicated. The common factor is that the heart tries very hard to pump blood to the brain and doesn’t think it’s succeeding. In cases where it does fail, the brain goes into standby mode, and we faint. With all of these possible mechanisms, no solution to POTS can hope to work for everyone. Treating underlying causes is a good start, if applicable. Beyond that, each case is unique, and sufferers must talk with a medical professional to find a solution that works for them. There are no approved medications for POTS, but a doctor may prescribe something off-label that could work in a specific case. Non-medicinal remedies include drinking more water (soda does NOT count), eating more salt, and compression leggings. These should go to the waist to avoid blood pooling about the knees. The best long-term solution is physical conditioning – exercise. This can be very difficult in severe cases of POTS as it can cause exercise intolerance. A good goal is around 20-30 minutes of aerobic exercise three times a week. As with all lifestyle and medication changes, talking to a medical professional is a good idea. With POTS and its varied causes, signs, and symptoms, it is critical. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Dysautonomia International, (2019). Postural Orthostatic Tachycardia Syndrome. https://dysautonomiainternational.org/page.php?ID=30 Grubb, B. P. (2008). Postural tachycardia syndrome. Circulation, 117(21), 2814-2817. https://www.ahajournals.org/doi/full/10.1161/circulationaha.107.761643 Olshansky, B., Cannom, D., Fedorowski, A., Stewart, J., Gibbons, C., Sutton, R., … & Benditt, D. G. (2020). Postural orthostatic tachycardia syndrome (POTS): a critical assessment. Progress in cardiovascular diseases, 63(3), 263-270. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9012474/ Raj, S. R. (2006). The postural tachycardia syndrome (POTS): pathophysiology, diagnosis & management. Indian pacing and electrophysiology journal, 6(2), 84. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1501099/
Scroll down to listen to this article.
Listen to the article here:
I remember the early days of COVID-19, everything was new and scary and dangerous and no one knew what was going on. It seemed to be very dangerous for two groups of people, those of advanced age and those who were immunocompromised. Vaccines rolled out, testing became easy, and things have calmed down quite a bit. But corona isn’t all limes on the beach, as any virus, it’s still dangerous for people who are immunocompromised. What does this term mean, who are the immunocompromised, and is there anything they can do in the new reality of COVID-19? Immunocompromised is a broad term. It indicates that a person’s immune system cannot generate an appropriate response to infection. When bacteria or viruses make it inside these people’s bodies, they cause much more damage and are very hard to control. The immune system is very, very complicated, so there are many ways a person can become immunocompromised. We can generally lump these into two categories: primary and secondary immunodeficiency. Primary immunodeficiency means the condition is built-in to the body; it’s genetic. Primary immunodeficiencies are fairly rare, with <0.1% of the population experiencing them. The rest of the almost 3% of people who have immunodeficiencies have secondary immunodeficiencies.Infectious diseases (such as HIV), malnutrition, age, surgery, environmental stress, and immunosuppressive drugs can all cause secondary immunodeficiency. Immunodeficiency affects millions of Americans. Women are twice as likely as men to have immunodeficiency; it is most common in white Americans and those aged 50-59. Nearly 3% of the population – over 9 million Americans – are suspected to have immunodeficiency. Unfortunately, immunodeficiency can greatly reduce a person’s ability to deal with a COVID-19 infection. The most obvious problem is that immunocompromised people are more susceptible to severe symptoms. A disproportionate amount of people who are hospitalized for COVID-19 are immunocompromised. Immunodeficiency doesn’t compromise, it packs a double-whammy. Those with a weak immune system also find vaccines less effective! In fact, 44% of people who had “breakthrough” cases (where they were vaccinated but still hospitalized) were immunocompromised. This is because the body is unable to produce enough protective antibodies for the body to be protected – a process called seroconversion. Seroconversion is when antibodies are able to be detected in the blood. With vaccines, successful seroconversion indicates that the body is protected and has the equipment necessary to put up a good fight against the COVID-19 virus. When vaccinated against COVID-19, people with healthy immune systems showed seroconversion rates of 99%. The type of immunocompromisation affects how well vaccines produce seroconversion. People with solid tumor cancers, such as breast, colon, prostate, and lung cancer show seroconversion rates of 92%. Immune-inflammatory disorders like lupus, primary biliary cholangitis, psoriasis, and rheumatoid arthritis have seroconversion rates reduced to 78%. Vaccine effectiveness in people with blood cancers such as lymphomas, myeloma, and leukemia drops to 64%. Those with organ transplants have to be on strong immunosuppressive drugs to avoid organ rejection and because of this they have the lowest rates of seroconversion, only 27%.
Some factors of immunocompromisation. Adapted from Chinen, J., & Shearer, W. T. (2010).
So what can immunocompromised people do to protect themselves against COVID-19? A lot of the same things as people who are immunocompetent! High quality masks and respirators can help. Avoiding crowds and indoor areas with poor ventilation is a must. Washing hands with soap and water is critical, though hand sanitizer is a good second option. Immunocompromised people who contract COVID-19 should contact their doctor or other healthcare provider right away. Isolating and using masks to prevent the spread is always a good idea. Immunocompromised people may also keep infections from getting out of control if their medical provider recommends an antiviral medication or convalescent plasma. Of course, the best way to avoid getting sick with COVID-19 is through prevention, including vaccines. A 27% seroconversion rate is much better than 0% after all. And there may be more hope for immunocompromised people, as new vaccines are being developed to serve this community. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Boyle, J. M., & Buckley, R. H. (2007). Population prevalence of diagnosed primary immunodeficiency diseases in the United States. Journal of clinical immunology, 27, 497-502. https://link.springer.com/article/10.1007/s10875-007-9103-1 Chinen, J., & Shearer, W. T. (2010). Secondary immunodeficiencies, including HIV infection. Journal of Allergy and Clinical Immunology, 125(2), S195-S203. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6151868/ Harpaz, R., Dahl, R. M., & Dooling, K. L. (2016). Prevalence of immunosuppression among US adults, 2013. Jama, 316(23), 2547-2548. https://jamanetwork.com/journals/jama/fullarticle/2572798 National Institute of Health. (July 21, 2023). Special considerations in people who are immunocompromised. COVID-19 Treatment Guides, https://www.covid19treatmentguidelines.nih.gov/special-populations/immunocompromised/ Parker, E. P., Desai, S., Marti, M., Nohynek, H., Kaslow, D. C., Kochhar, S., … & Wilder-Smith, A. (2022). Response to additional COVID-19 vaccine doses in people who are immunocompromised: a rapid review. The Lancet Global Health, 10(3), e326-e328. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(21)00593-3/fulltext SY, L. A. W., SC, C. L. L., & Muthiah, L. M. (2021). Efficacy of COVID-19 vaccines in immunocompromised patients: A systematic review and meta-analysis. medRxiv. https://doi.org/10.1136/bmj-2021-068632
Scroll down to listen to this article.
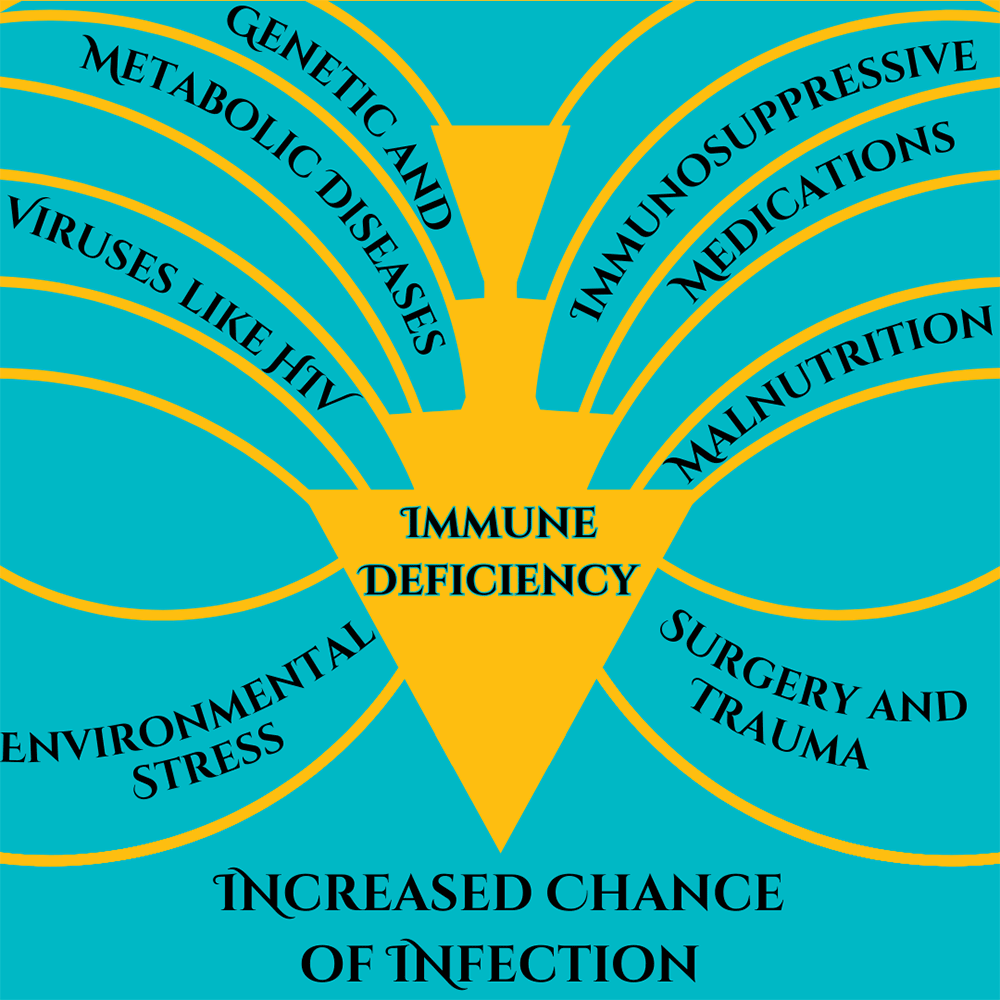
Listen to the article here:
Pain isn’t fun. So why do we feel it then? Because it is a learning mechanism. When I burn myself tasting boiling soup I quickly pull the spoon away, blow on it, and learn not to do that again until tomorrow. Pain is useful, but what about when it’s not? Fibromyalgia is a condition where the body’s sensitivity to pain has increased beyond the useful range. Instead of keeping you from stopping damaging activities, it can stop people from performing healthy ones. It is a complex, poorly understood disease. Fibromyalgia affects between 2-8% of the world population, somewhere around 500 million people worldwide. It mostly affects women and onset is usually between 30 and 35 years of age. Risk factors include being female, experiencing trauma, infections, diabetes, inflammatory diseases, neurological and psychiatric disorders, genetics, and oxidative stress. Major symptoms include: Fibromyalgia is hard to diagnose because it doesn’t have physical symptoms that we know how to detect. Doctors look for pain that has been spreading for three or more months. A rheumatologist (a doctor who specializes in inflammatory diseases), may provide the diagnosis. How does fibromyalgia work? It is multifactorial, meaning there are several possible causes that all lead to the same result. Because of this, looking at individual causes may not be helpful. Instead, according to Dr. Siracusa, fibromyalgia “…is thought to represent the degradation of the autonomic nervous system in a failed attempt to adapt to a hostile environment” (Siracusa, 2021). The autonomic nervous system is the part which controls involuntary activity, like heart rate and digestion. This theory holds that as this system breaks down from repeated or constant stresses to it; it eventually fails to interpret pain signals in a useful way. Some of these stresses may include: We will digress here to talk about some of the controversy and problems with fibromyalgia. It is hard to diagnose, doesn’t leave good molecular clues, and is hard or impossible to see. This has led to widely proliferated discounting of the symptoms, even by medical professionals. This is unacceptable. I have heard that fibromyalgia is “in their head.” Even if true, this doesn’t mean it’s any less real! Chronic and sensitized pain is debilitating. Having acquaintances and medical professionals dismiss debilitating symptoms can be devastating. With any change in how we sense the world, there are changes in the body and brain. With fibromyalgia, the most likely culprit of change is the pain system. This system, called the nociceptive system, becomes high strung, firing willy-nilly. There are changes to neurotransmitter levels, molecules that lessen pain, and nerve fibers associated with pain. Many of these changes occur in the peripheral nervous system; the nerves outside of the brain and spinal cord. There are also changes to overall brain structure, which may lead to pain when at rest. Central sensitization is a term for a state of increased pain sensitivity. Repeated injury or pain can cause sensitization, where the nerves that send pain signals fire more easily and at inappropriate times. We are just beginning to see the differences in how the brain fires using MRI and fMRI (functional magnetic resonance imaging) technology. What can be done about fibromyalgia? There are no cures, but there may be some methods to find a modicum of relief. Education is the first piece of the puzzle. Understanding what fibromyalgia is and that it tracks changes in your body can help you understand what is going on. One of the stressors to the pain system is stress and anxiety. Along with education, psychotherapy may provide some relief. Fitness can also help, and is particularly helpful when a patient has received dismissive medical advice in the past. Some patients experience a reduction in symptoms with a low glutamate diet. This is NOT a low gluten diet. Glutamate is a neurotransmitter that is a possible culprit for some nociceptive changes. Low glutamate diets are specific, quite restrictive diets that should be discussed with a dietitian. MSG, aspartame, protein concentrates, smoke flavoring, and more are all restricted on this diet. Finally, some fibromyalgia patients find relief with medication. Some specific anti-nociceptive neurotransmitter medications seem to help, as do other specific brain-altering medications. Some patients find relief with medical marijuana or prescription opioids, though side effects may not be worth it. Across the board, NSAIDs, such as ibuprofen (motrin, advil), aspirin, and naproxen (aleve) do NOT seem to provide relief. Talking to a medical professional is a good idea before making changes to your medical routine or diet. Hopefully this article helps with the education aspect of relief, and hopefully sufferers can find more as well! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Holton, K. F., Taren, D. L., Thomson, C. A., Bennett, R. M., & Jones, K. D. (2012). The effect of dietary glutamate on fibromyalgia and irritable bowel symptoms. Clin Exp Rheumatol, 30(6 Suppl 74), 10-7. Kandel, E. R., Schwartz, J. H., Jessell, T. M., Siegelbaum, S., Hudspeth, A. J., & Mack, S. (Eds.). (2000). Principles of neural science (Vol. 4, pp. 472-479). New York: McGraw-hill. Sagy, I., Bar-Lev Schleider, L., Abu-Shakra, M., & Novack, V. (2019). Safety and efficacy of medical cannabis in fibromyalgia. Journal of clinical medicine, 8(6), 807. https://doi.org/10.3390/jcm8060807 Siracusa, R.; Paola, R.D.; Cuzzocrea, S.; Impellizzeri, D. Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. Int. J. Mol. Sci. 2021, 22, 3891. https://doi.org/10.3390/ijms22083891
Scroll down to listen to this article.
Listen to the article here:
Medical terminology can be hard to understand. Much of it is in Latin, some is in Greek, several words are named after people, and terminology can change. Sometimes that change is a good thing, though. In June 2023 a collaboration of hundreds of experts in liver disease released new names for the liver diseases previously known as Nonalcoholic Fatty Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH).
Adapted from Rinella, M. E., et al., 2023
Under the broad category of Steatotic Liver Disease (SLD) we now have Metabolic dysfunction Associated Steatotic Liver Disease (MASLD), which can progress to Metabolic Dysfunction-Associated Steatohepatitis (MASH) and Metabolic Alcohol-associated Liver Disease (MetALD, which is MASLD and increased alcohol intake). This change was made for many reasons. The terms “non-alcoholic” and “fatty” may have been confusing, stigmatizing, or inaccurate. People who are not overweight may still have the disease, and those with the disease may still be consuming alcohol. Finally, naming a disease after what it isn’t (“nonalcoholic…”) is less than ideal. The new system describes the same symptoms but with more specific language. Steatosis is the accumulation of fat inside of cells and the disease is caused by changes in the metabolic system; how our cells change food into energy. A critical change has also been made with the adoption of the new term MetALD. MetALD describes people who have MASLD, but who still consume some alcohol. Alcohol affects the disease progression, but metabolic disruptions do as well. Hence, a term was developed to describe this overlap. These terms were planned and adopted by an international group of clinical researchers, scientists, educators, industry experts, and patient advocates. The American Association for the Study of Liver Disease (AASLD), European Association for the Study of the Liver (EASL), Asian Pacific Association for the Study of the Liver (APASL), and Asociación Latinoamericana para el Estudio del Hígado (ALEH) made up most of the participants and have ensured widespread adoption of the new terminology Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Rinella, M. E., Lazarus, J. V., Ratziu, V., Francque, S. M., Sanyal, A. J., Kanwal, F., … & NAFLD Nomenclature consensus group. (2023). A multi-society Delphi consensus statement on new fatty liver disease nomenclature. Annals of Hepatology, 101133. https://doi.org/10.1097/HEP.0000000000000520
Scroll down to listen to this article.
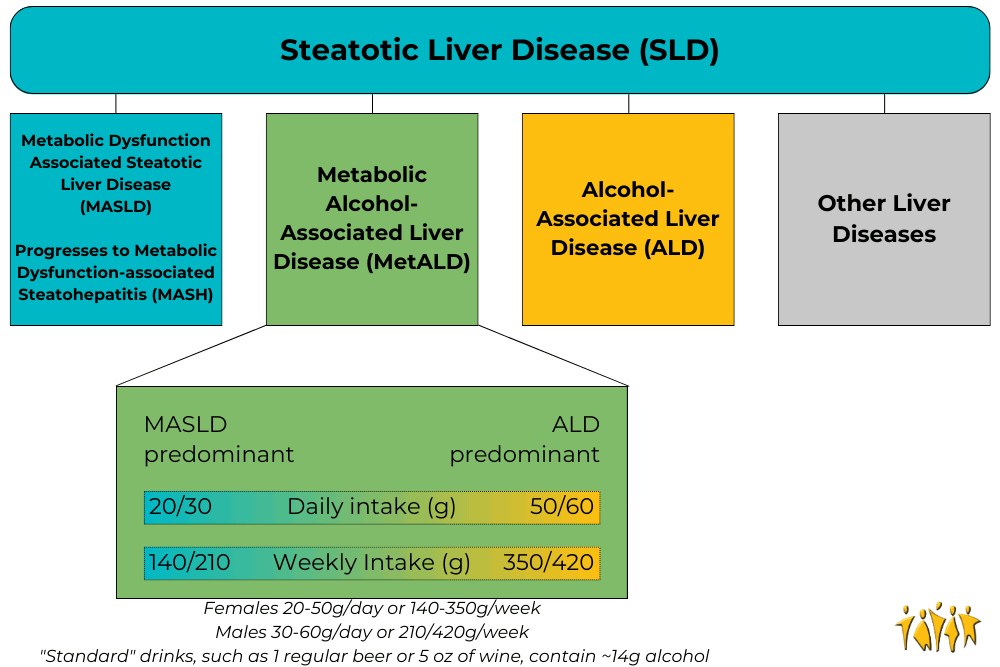
Listen to the article here:
Nonalcoholic Steatohepatitis, or NASH, has no approved medications available for treatment. This isn’t because the disease is safe, however. NASH can lead to cell death, cells going rogue, collagen accumulation, fibrosis, cirrhosis, and liver cancer. One problem with treating NASH is that it is a multifactorial disease, meaning there are many possible causes that all lead to the same outcome. The current best methods for treating NASH are exercise, weight loss, and treating other conditions that may contribute. We will discuss scientifically backed information regarding these treatment options, but it is critical that any medical advice be discussed with your doctor. NASH has many many causes and affects a lot of body systems. Medical professionals that may be involved in NASH treatment include your primary care physician, a hepatologist, dietitian, endocrinologist, cardiologist, and others. Every person is an experiment of one, and your specific circumstances may contraindicate one or all of the methods discussed below. Talk to your doctor. Weight loss is the go-to method of treating NASH. A combination of diet and exercise is the best method to achieve weight loss. This ensures fewer calories enter the body than exit it, and that the body is burning weight from fat instead of from muscle. Losing weight very rapidly can be dangerous, so be conscientious of your body’s overall health (and speak with a professional!) Research has shown that reducing weight by as little as 5% (12.5 lbs for a 250 lb person) can help improve steatosis, the fat buildup in the liver. Losing 7% or more (17.5 lbs for a 250 lb person) also shows a reduction in inflammation and improved health of liver cells. When patients, particularly obese patients, lose 10% of their body weight (25 lbs for a 250 lb person) the structural liver changes known as fibrosis start to regress or stabilize. For NASH patients of a normal weight, they may see results when losing as little as 3-5% of body weight. Exercise is a great way to lose weight, but studies have shown that exercise can help your liver even when you aren’t losing weight. The exact mechanisms for how this works are complex and not fully known. Scientists have found that exercise helps make the body more sensitive to insulin – which helps it regulate blood sugar better. It can also help cellular metabolism. Exercise is associated with a reduction in the markers of liver inflammation and may help liver cells stay healthy. Aerobic exercise, also called “cardio,” is highly recommended. Resistance training, called strength training, is also helpful, especially if aerobics are not possible. NASH patients start seeing benefits when doing exercise for 150-300 minutes (2 ½ – 5 hours) per week of moderate intensity exercise or 75-150 minutes (1 ¼ – 2 ½ hours) per week of high intensity exercise. Always ease into a new exercise routine to avoid injury. Talking to a medical professional is also a good idea before starting new exercises (there is a theme to this article). Exercise burns calories, but to lose weight we also want to manage what calories we take in. Consult with your doctor or dietitian, but reducing caloric intake to around 500 fewer than the daily recommended value may help. Further, the number of calories is not directly correlated to the quality of the calories. NASH patients find improvements when reducing items that can damage the liver, including fructose and saturated fats. Fructose is a form of sugar that is often added to sugary beverages (usually in the form of high fructose corn syrup) and contributes to insulin resistance. Saturated fats are found in meats, including red meats and processed meats. As for specific diets, research is ongoing. The Mediterranean diet has the most research backing its success in NASH patients. It is rich in fruits, vegetables, whole grains, seafood, nuts, legumes, and olive oil. Other diets may be suitable as well, including intermittent fasting, ketogenic diet, and others. One recommendation is to take the Mediterranean diet and adjust it to fit you. Regardless of the diet choice, alcohol should be limited. For smokers and former smokers, alcohol should be eliminated entirely. It should go without saying that making major adjustments to your diet should be consulted with your doctor. Other than diet and exercise, treatments for NASH are all achieved by treating other conditions that contribute, and will vary depending on the individual. Conditions that contribute are obesity, diabetes, high blood pressure, high cholesterol, cardiovascular disease, and obstructive sleep apnea. Cardiovascular disease and obstructive sleep apnea are major contributors of mortality for NASH patients and should be taken seriously. Obviously these conditions are best treated by going to your doctor. NASH is a progressive disease that gets worse over time and leads to serious, occasionally deadly complications. Clinical trials may give us a medical NASH treatment in the future. Until then, give yourself a leg up (or liver) by consulting your doctor about treatments through diet, exercise, and underlying condition management. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: American Liver Foundation. (March 16, 2023). What are the treatments for NAFLD and NASH? NASH Treatment, https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-steatohepatitis-nash/nash-treatment/ Van der Windt, D. J., Sud, V., Zhang, H., Tsung, A., & Huang, H. (2018). The effects of physical exercise on fatty liver disease. Gene Expression The Journal of Liver Research, 18(2), 89-101. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5954622/ Younossi, Z. M., Corey, K. E., & Lim, J. K. (2021). AGA clinical practice update on lifestyle modification using diet and exercise to achieve weight loss in the management of nonalcoholic fatty liver disease: expert review. Gastroenterology, 160(3), 912-918. https://doi.org/10.1053/j.gastro.2020.11.051
Scroll down to listen to this article.
Listen to the article here:
Is the liver the most amazing organ? Yes. It turns food into usable molecules. It makes proteins, bile, and hormones. It filters dangerous drugs and toxins. Without it, you would die within minutes. Also, the liver can regenerate (like a lizard’s tail!), which is basically magic. The liver is estimated to have over 500 individual functions and interacts with most body systems. In this article we’ll look at the liver, zooming in from basic facts to its cellular units. Then we’ll explore the functions of the liver. If you were to guess the largest organ in the body, would you guess the liver? I hope not, because it’s the skin. But the liver is in second place! It makes up around 2% of your body weight and usually contains about 10% of your blood. It’s located under the ribs, right below the diaphragm that inflates the lungs. It’s smooth and reddish brown when healthy (note: if you can see your liver’s color you are probably having a bad day). The liver can be divided into four parts called lobes and thousands of sub-parts called lobules. These are hexagonal columns of cells arranged so that blood can travel through carrying nutrients in and toxins and waste out. Four types of cells make up the liver: hepatocytes, epithelial cells, Kupffer cells, and stellate cells. Most of the liver is composed of hepatocytes. These are the workhorses of the liver. Hepatocytes convert fats (called lipids), sugars (called carbohydrates), and proteins (called proteins) into usable forms. They detoxify dangerous things and excrete bile and cholesterol. The barrier epithelial cells line the walls (including blood vessel walls) inside the liver and do some filtering of small particles. It is thought that these may also do some clearance of viruses. Kupffer cells are the resident immune cells. These large cells eat bacteria and debris that enter lobules. They are always touching these dangerous particles and exhibit a constant, low-level inflammation. Disruption of these cells can result in widespread, damaging liver inflammation. Finally, stellate cells store vitamin A, a critical vitamin. They are critical for promoting the liver’s amazing ability to regenerate. They form temporary scars that allow for healing. When they are damaged, however, they lose vitamin A. Damaged stellate cells can “activate” and run amok, secreting a lot of collagen that causes fibrosis and permanent scarring called cirrhosis. To understand the liver’s major functions, let’s first look at our body cells. Cells need to have a balance of chemicals to function properly. Normally cells control what goes in and out of them using special proteins. To keep unwanted things out, cells are separated from the environment around them. This separation is done by a membrane made of phospholipids. The –lipid at the end is another word for fat. Since the borders of our cells are made of fats, things that can pass through fats (called fat-soluble) can easily pass through the cell membranes. Cells can’t control this very well, so we use the liver instead. Let’s run through the liver’s major functions of storage, conversion, and creation. Storage is fairly simple. The liver stores fat-soluble vitamins and converts some of them into usable forms. It stores a quick supply of energy in the form of glycogen. Blood is stored in large quantities in the liver. This makes sense, because the liver is filtering the blood. Usually it holds a little more than 10% of the body’s blood, but the liver can expand to hold much more if needed. It can also squeeze blood out if the body is bleeding profusely. This probably isn’t great for the liver, but then again neither is bleeding out and dying. The liver converts a huge amount of material from one form into another. It acts as a gatekeeper for nearly all the blood in the body, including blood directly from the digestive tract. This includes tasty nutrients like fat and sugar, and dangerous toxins, like alcohol and methamphetamine. Blood is carried across the lobules and filtered through the hepatocytes and Kupffer cells. The liver doesn’t just remove dangerous particles, however, it metabolizes them! Metabolism is the conversion of chemicals from one form to another. One of the most important metabolic functions is detoxification. To make drugs and toxins less dangerous, the liver converts them from being fat-soluble (able to pass through cell membranes) to being water-soluble (able to be released through urine but much harder to enter cells). Carbohydrates are converted to glycogen for storage. The liver changes fats into energy for use. Proteins are broken into building blocks and waste products are removed. Remnants of dead blood cells called bilirubin are turned into bile and used for digestion. The conversion of materials into component parts helps the liver’s third broad function, creation. The liver creates, or synthesizes, many molecules that are used all around the body. It creates important hormones like angiotensin and thyroxine. It makes chemicals for the blood like prothrombin, fibrinogen, and clotting factors. It also makes the aforementioned bile, which is critical for digesting fats. The liver is the ultimate hero. Through all of these functions, the liver acts in the best interest of the body. It takes the hit from dangerous chemicals and sacrifices its own blood when we need it most. The liver is a team player of the highest degree. When it goes wrong we suffer throughout our whole body. Take care of that liver! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Eng, F. J., & Friedman, S. L. (2000). Fibrogenesis I. New insights into hepatic stellate cell activation: the simple becomes complex. American Journal of Physiology-Gastrointestinal and Liver Physiology, 279(1), G7-G11. https://doi.org/10.1152/ajpgi.2000.279.1.G7 Geerts, A. (2001). History, heterogeneity, developmental biology, and functions of quiescent hepatic stellate cells. In Seminars in liver disease (Vol. 21, No. 03, pp. 311-336). https://doi.org/10.1055%2Fs-2001-17550 Kalra, A., Yetiskul, E., Wehrle, C. J., & Tuma, F. (2018). Physiology, liver. https://europepmc.org/article/nbk/nbk535438 Lautt, W. W. Hepatic Circulation: Physiology and Pathophysiology. San Rafael (CA): Morgan & Claypool Life Sciences; 2009. Chapter 2, Overview. https://www.ncbi.nlm.nih.gov/books/NBK53069/ Ozougwu, J. C. (2017). Physiology of the liver. International Journal of Research in Pharmacy and Biosciences, 4(8), 13-24. Vaja, R., & Rana, M. (2020). Drugs and the liver. Anaesthesia & Intensive Care Medicine, 21(10), 517-523. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7508170/ Yin, C., Evason, K. J., Asahina, K., & Stainier, D. Y. (2013). Hepatic stellate cells in liver development, regeneration, and cancer. The Journal of clinical investigation, 123(5), 1902-1910. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3635734/
Scroll down to listen to this article.
Listen to the article here:
The liver is an amazing and complex organ. It can regenerate from damage, helps us digest and function, filters some toxins, and in return gets thoroughly abused by us humans. Alcohol can damage the liver, but most livers are mistreated through other means, like diabetes and obesity. This is visible in the form of accumulated fat in the liver and can lead to serious problems. Nearly 1 in 4 adults in America have non-alcoholic fatty liver disease (NAFLD). When a fatty liver becomes inflamed and damaged it is called nonalcoholic steatohepatitis, or NASH. NASH is dangerous, and is an indication of decreased liver health. If untreated, NASH will degrade the liver, potentially leading to scarring known as fibrosis and permanent cirrhosis. Cirrhosis is cirrhiously bad. At this time, there are no approved therapies for the treatment of NASH. The current standard of care is exercise and weight loss to alleviate problems that damage the liver. Unfortunately, much like trying to lick your elbow, this is easier said than done. The consequences of an impaired liver include liver failure, cirrhosis, cancer, cardiovascular disease, and more. To alleviate this burden, scientists have identified several medical approaches to combating fatty liver. These approaches generally target the underlying mechanisms that lead to a fatty liver, aiming for a long-term solution. The broadest categories for investigative NASH medication are managing fat, sugar, and inflammation in the liver. One of the liver’s major jobs is to balance the body’s energy storage needs by managing fat. One method of dealing with excess fats is to dump extra fats out of the body through the digestive system. Thyroid hormone receptor beta (THR-β) can help us do just that. Receptors are parts of a cell that detect what’s happening outside its borders. They interact with hormones, sugars, fats, or other things. Each receptor only reacts to specific molecules. When activated, THR-β may help reduce the accumulation of fats in the liver by telling the body to move fats from the liver to the gut. Medications that activate THR-β are being investigated to see if they can also do this. Another method of helping the liver manage fat is to stop fats from being created in the first place. Unfortunately, some people create an unhealthy amount of fat. They may have a mutated gene called PNPLA3. PNPLA3 genetic disorder affects how the fat cells in the body deal with triglycerides. This mutation can increase liver fat and possibly lead to NASH. Scientists are working on ways of suppressing this gene. Other research targets being studied for limiting fat production include peroxisome proliferator-activated receptor alpha (PPARα). This is a chemical receptor on liver cells that regulates how fats are processed. When activated, this receptor can lower fat creation and lead to lower blood triglycerides (the most common type of fat). Rampant activation can be dangerous, however, so very specialized Selective PPARα Modulator (SPPARMα) medications are being developed to target the system with specificity and finesse. These medications also target and activate a very interesting hormone called fibroblast growth factor 21 (FGF21), which we will cover in the next section. Fats can’t take all the spotlight, though, because one of the biggest culprits of liver damage is actually sugar. As a cookie lover, this makes me very sad. Sugars, also called glucose, are converted into fats (stored in the liver) and can damage the liver, metabolic system, heart, etc. The body detects high levels of sugar in the pancreas. High blood sugar signals the release of insulin and amylin from the pancreas to the liver. The liver then starts breaking down, converting, and storing sugars. A couple of medications look to target this system to lower the burden on the liver and help with NASH. Fibroblast growth factor 21 (FGF21), mentioned above, has broad effects, including in the pancreas. It helps manage the body’s metabolism and homeostasis and makes the pancreas more sensitive to insulin. This may be particularly helpful for people with insulin resistance. Insulin resistance leads to type 2 diabetes. FGF21’s other effects appear to include increasing energy use, potentially leading to weight loss. Glucagon-like peptide-1 (GLP-1) agonists, like Semaglutide, Trulicity, and Mounjaro, act on the same system. These directly attach to pancreatic cells, preparing them for a large insulin release when they detect high glucose levels. It is hoped that this can help the liver deal with high blood sugar without taking damage. Another potential pathway to managing blood sugar is to send it down the yellow-brick road. Sodium-glucose cotransporter-2 (SGLT2) inhibitors deal with blood sugar by expelling it out of the body with urine. The final target of potential NASH treatments is inflammation. NASH stands for nonalcoholic steatohepatitis, which literally means “non-alcoholic inflammation of the liver (due to) fat.” Inflammation is like a visit with the inlaws: good when it doesn’t last too long. Researchers hope that reducing chronic inflammation may help limit the damage of NASH and prevent a worsening of the disease. Luckily, two avenues of treatment above also target inflammation. One complication of the PNPLA3 genetic mutation is an increase in cyclophilin, a protein that can increase inflammation. By reducing excess cyclophilin through PNPLA3 management – or by targeting it directly, inflammation may be relieved. Interestingly, FGF21, which may be used to lower blood sugar, appears to lower inflammation in the pancreas. The hope is that these medical interventions may also help the liver downstream. Overall, the liver is complex, and trying to keep it from being damaged is difficult. The only real treatment available today is weight loss through diet and exercise. With luck and help from the clinical trial process, there may be new avenues available in the future. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Fisher, F. M., & Maratos-Flier, E. (2016). Understanding the physiology of FGF21. Annual review of physiology, 78, 223-241. https://www.annualreviews.org/doi/full/10.1146/annurev-physiol-021115-105339 Geng, L., Lam, K. S., & Xu, A. (2020). The therapeutic potential of FGF21 in metabolic diseases: from bench to clinic. Nature Reviews Endocrinology, 16(11), 654-667. https://www.nature.com/articles/s41574-020-0386-0 Prasad, A. S. V. (2019). Biochemistry and molecular biology of mechanisms of action of fibrates–an overview. International Journal of Biochemistry Research & Review, 26(2), 1-12. https://doi.org/10.9734/ijbcrr/2019/v26i230094 Shen, J. H., Li, Y. L., Li, D., Wang, N. N., Jing, L., & Huang, Y. H. (2015). The rs738409 (I148M) variant of the PNPLA3 gene and cirrhosis: a meta-analysis. Journal of lipid research, 56(1), 167-175. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4274064/ Sinha, R. A., Bruinstroop, E., Singh, B. K., & Yen, P. M. (2019). Nonalcoholic fatty liver disease and hypercholesterolemia: roles of thyroid hormones, metabolites, and agonists. Thyroid, 29(9), 1173-1191. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6850905/ Ure, D. R., Trepanier, D. J., Mayo, P. R., & Foster, R. T. (2020). Cyclophilin inhibition as a potential treatment for nonalcoholic steatohepatitis (NASH). Expert opinion on investigational drugs, 29(2), 163-178. https://doi.org/10.1080/13543784.2020.1703948 US Department of Health and Human Services, National Institute of Health, National Institute of Diabetes and Digestive and Kidney Diseases. (April, 2021). Definition & facts of NAFLD & NASH. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts Wang, P., & Heitman, J. (2005). The cyclophilins. Genome biology, 6(7), 1-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1175980/
Scroll down to listen to this article.
Listen to the article here:
Old houses have creaky doors, and old bodies have creaky joints. Both are caused by the degradation of the joints. With doors, the lubrication from the hinges may have degraded, or the hinge may be out of alignment, causing the grinding of metal on metal. Our joints, including knees, are similar. The joints degrade, often from misalignment, causing pain and deformation. Unfortunately, we can’t pick up a replacement knee at the local hardware store. The most common condition causing joint degradation is osteoarthritis (OA). It affects around 20% of the global population, 500 million people. At its most basic, osteoarthritis is when joints start breaking down. It can affect different joints, but the knees are the most likely to be affected. Cartilage, the strong and flexible tissue that protects your joints and bones, breaks down in osteoarthritis. This causes joint pain, swelling, and loss of function (including range of motion) for the affected joint and may exacerbate comorbidities like diabetes and heart trouble. Women are more likely than men to have osteoarthritis and tend to have more severe symptoms. One major risk factor is obesity, which puts extra stress on joints like the knees and hips. They say age is just a number, but it is also a significant risk factor for OA. The risk of osteoarthritis peaks in a person’s ’60s. The incidence of osteoarthritis has more than doubled in the last 30 years, largely due to the aging global population. A big danger of OA is physical damage caused to the joint affected. This is called a biomechanical abnormality and could be due to a joint that is misaligned or has suffered prolonged abuse. Other risk factors for developing OA include metabolic syndrome, genetics, and trauma, such as torn ligaments. So what causes osteoarthritis? A lot of things! Cartilage is broken down, but many things may cause this. Outside of the joint, changes in bone, ligament, and muscle can cause stress or degradation. Inside the joint, inflammation, and cell death can lead to failure of the support structures. Inside joints are chondrocytes, the only type of cell in healthy cartilage. They normally spend their whole lives building and maintaining cartilage. They are so dedicated to their job that they become embedded in the structure of cartilage and die in place. With osteoarthritis, stressors (including the risk factors above) can cause chondrocytes to lament the poor work/life balance and start acting irrationally. Some chondrocytes degrade and stop supporting the cartilage (often by dying), and some go into overdrive, becoming larger and further destabilizing our cartilage structure. This causes the cartilage to shrink, and bones can start grinding against each other resulting in joint degradation. This is very painful and can reduce the quality of life dramatically. What can be done? One of the most important steps is to stop biomechanical abnormalities. Physiotherapy may help fix misalignments. Weight loss, lifestyle changes, and assistive walking devices can help reduce stress on joints. Surgery may be needed to replace or rebuild joints. Unfortunately, there are no approved medications that can cure osteoarthritis. Some anti-inflammatory medications may provide some relief, and are often prescribed. Luckily, the future is looking bright. Researchers are looking at new ways to target osteoarthritis, including next-generation anti-inflammatory medications, metabolic therapies, and even therapies that may rebuild cartilage through medication! In the future, we might not need to pick up a new knee at the hardware store, we might be able to build a new one on-site! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Goldring, M. B., & Otero, M. (2011). Inflammation in osteoarthritis. Current opinion in rheumatology, 23(5), 471. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3937875/ Gu, Y. T., Chen, J., Meng, Z. L., Ge, W. Y., Bian, Y. Y., Cheng, S. W., … & Peng, L. (2017). Research progress on osteoarthritis treatment mechanisms. Biomedicine & Pharmacotherapy, 93, 1246-1252. https://doi.org/10.1016/j.biopha.2017.07.034 He, Y., Li, Z., Alexander, P. G., Ocasio-Nieves, B. D., Yocum, L., Lin, H., & Tuan, R. S. (2020). Pathogenesis of osteoarthritis: risk factors, regulatory pathways in chondrocytes, and experimental models. Biology, 9(8), 194. https://www.mdpi.com/2079-7737/9/8/194 Poole, A. R., Guilak, F., & Abramson, S. B. (2007). Etiopathogenesis of osteoarthritis. Osteoarthritis: diagnosis and medical/surgical management, 4, 27-49. https://www.sciencedirect.com/science/article/abs/pii/S0025712508001223?via%3Dihub Long, H., Liu, Q., Yin, H., Wang, K., Diao, N., Zhang, Y., … & Guo, A. (2022). Prevalence trends of site‐specific osteoarthritis from 1990 to 2019: findings from the Global Burden of Disease Study 2019. Arthritis & Rheumatology, 74(7), 1172-1183. https://doi.org/10.1002/art.42089
Scroll down to listen to this article.
Listen to the article here:
I remember a joyous time when the world was young, and we had nothing to fear or worry about except climate change, an artificial intelligence cascade, political strife, and nuclear war. But we didn’t have to worry about COVID, so it was pretty idyllic. Now, over three years later, the biggest worries of COVID are winding down. The WHO declared COVID-19 to no longer be a global health emergency on May 5, 2023, and most places have lifted or lessened restrictions put in place to stem the spread. People have stopped wearing masks, and life seems to be back to normal. But not for everyone. Long COVID has been described as COVID symptoms that last longer than 5 weeks and may last months or longer. It affects around ⅓ of COVID patients, including over 85% of those that had to go to the hospital with severe symptoms. So what is long COVID, who gets it, how does it work, and is there anything to be done about it? Long COVID, also called long haul COVID, post-COVID syndrome (PCS), or Post-acute sequelae of SARS-CoV-2 infection (PASC), is different from person to person but can be debilitating. During acute (normal) COVID infections, people experience trouble with breathing, joint pain, headache, fatigue, stomach problems, and loss of smell and taste. When I had COVID, my sense of taste was so poor that I started liking Limp Bizkit again. Long COVID symptoms are similar to those of acute COVID. Long-lasting and often crushing fatigue is the most common symptom. I’ve heard anecdotal stories of people who run out of energy just deciding what to eat during the day; it can be very intense. Other symptoms include muscle pain, cognitive impairment such as brain fog, headaches, anxiety, and more. Around 140 million Americans have had COVID at some point. A recent study found that long COVID was more common and severe in people infected before the 2021 Omicron variant. Several other risk factors have also been identified. The severity of an acute COVID infection plays a role, as does having 5 or more separate symptoms. These can be mediated by being up to date on COVID vaccines. Long COVID is almost twice as common in women, and the risk is also increased if you are over 50 years old. Other health issues can also affect your chances. Being overweight, having psychiatric disorders, having asthma, and being in “poor general health” are risk factors. Interestingly, having latent Epstein-Barr virus might also increase your chances of developing long COVID. So how does all of this work? In the acute stage of COVID, the virus spreads rapidly and tries to reproduce. It gains entry into cells using its spike protein to fool a receptor on our cells called ACE2. It then hijacks cell machinery to make copies fast. This may kill the infected cells but also brings in the immune system, which kills the invaders (if we’re lucky) and tends to cause some damage through inflammation. It is thought that long COVID occurs through many mechanisms. The immune system can be disrupted, other infections can take hold, we can experience chronic inflammation, and some body systems can be messed up. Even worse, sometimes organs can be damaged from the infection, and the virus might stick around for a while! The major organs affected in long COVID can be deduced by looking at the symptoms. Trouble breathing, lung impairment, and low breath capacity may result from chronic inflammation and clotting in the lining of the lungs. Chest pain, irregular heartbeats, heart palpitations, and postural orthostatic tachycardia syndrome (POTS, low blood volume when standing up) are caused by chronic inflammation and cell death in the cardiovascular system. The cardiovascular system has an abundance of ACE2 receptors, meaning it is targeted for direct infection by the COVID virus. Fatigue, trouble sleeping, loss of taste and smell, and cognitive impairment are due to problems with our central nervous system. COVID can cross into the brain and cause inflammation of support cells and clotting (possibly leading to stroke!), and may also affect the brain stem. Nervous system problems affect around ⅓ of people by six months after COVID. There can also be problems with the kidney and pancreas. So what can we do? Our best bet is to reduce the effects of COVID in the first place – or avoid it altogether. Staying up to date on COVID vaccines and boosters lowers both the severity of acute COVID and the risks of developing long COVID. Continuing to wear masks, washing hands frequently, and being careful around sick people can also help, and staying healthy with diet and exercise can give a leg up. Unfortunately, if you already have long COVID, there are no meds proven to cure it. Treating symptoms is our current best practice. Supplements may help, including B vitamins, iron, magnesium, zinc, and selenium. Multivitamins, mineral supplements, and probiotics have shown preliminary promise, as has the antiviral paxlovid. ANY alteration of medication, including supplements, should be run by your doctor first to ensure they are safe and don’t interact with other conditions or medications you may be on. Non-pharmaceutical solutions may also help. Physical rehabilitation – including pulmonary rehabilitation – as well as mental health and social assistance are vital to making it down the long road of long COVID. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Conti, V., Corbi, G., Sabbatino, F., De Pascale, D., Sellitto, C., Stefanelli, B., … & Filippelli, A. (2023). Long COVID: clinical framing, biomarkers, and therapeutic approaches. Journal of Personalized Medicine, 13(2), 334. https://www.mdpi.com/2075-4426/13/2/334 Koc, H. C., Xiao, J., Liu, W., Li, Y., & Chen, G. (2022). Long COVID and its Management. International Journal of Biological Sciences, 18(12), 4768. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9305273/ Raveendran, A. V., Jayadevan, R., & Sashidharan, S. (2021). Long COVID: an overview. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 15(3), 869-875. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8056514/ Su, Y., Yuan, D., Chen, D. G., Ng, R. H., Wang, K., Choi, J., … & Heath, J. R. (2022). Multiple early factors anticipate post-acute COVID-19 sequelae. Cell, 185(5), 881-895. https://www.sciencedirect.com/science/article/pii/S0092867422000721 Thaweethai, T., Jolley, S. E., Karlson, E. W., Levitan, E. B., Levy, B., McComsey, G. A., … & Donohue, S. E. (2023). Development of a definition of postacute sequelae of SARS-CoV-2 infection. Jama. https://jamanetwork.com/journals/jama/fullarticle/2805540
Scroll down to listen to this article.
Listen to the article here:
Lung cancer is distressingly common. Worldwide, over 2 million people per year are diagnosed with lung cancer, including over 200,000 in the USA. It is more common in men than women. Lung cancer has many debilitating symptoms, including chest pain, voice changes, weight loss, discomfort, coughing blood, and death. Lung cancer is the highest cause of cancer death in men and the second highest in women, and the outlook gets worse the later in the disease you are diagnosed. So what causes lung cancer, how does it work, and is there anything we can do about it? Lung cancer has several different risk factors, including low socioeconomic status, HIV, and some lung diseases. According to the National Institute of Health, radiation from atomic bombs can also increase your risk, so avoid atomic bombs. None of these come even close to the explosive risk from smoking, however. Smoking causes lung cancer and increases your risk of developing lung cancer by 20 times versus people who have never smoked. Smoke contains a lot of chemicals. Some of these enter the cells that line the throat and lungs and damage the DNA. Unfortunately, the advent of filtered cigarettes encouraged people to inhale smoke more deeply and increased cancer rates. There are at least 15 genes implicated in the conversion of cells from normal to cancerous. Cigarette smoke, along with air pollution, other carcinogens, and random mutation, can change some of the DNA in these genes and make cells cancerous. Let’s take a quick second to review what cancer is. Cancer cells are cells that have mutated and act more like independent, single-celled organisms than part of your body. They grow and divide even when they aren’t supposed to, they don’t kill themselves when they outlive their usefulness, and they move around invading other parts of the body. Unlike most single-celled organisms, they are extremely difficult to kill. They are made out of our cells, so most medicines can’t distinguish them, they hide from the immune system, and they convince parts of the body to aid their unrestricted growth. Each of these is an individually unlikely mutation. Still, the damaging effects of carcinogens like cigarette smoke cause many rapid changes in the genes of the cell, increasing the possibility that cells will acquire the necessary mutations. As cells reproduce out of control, they are more likely to mutate and acquire the other necessary mutations to become cancerous. They act independently and take resources, space, and blood from healthy cells, crowding them out and destroying large body systems. Lung cancer is differentiated from other cancers in an obvious way; the cancerous cells originate in the lungs. Epithelial cells line the lungs and create a protective barrier against environmental hazards. When they are exposed to smoke and other carcinogens this can cause mutations. Medical professionals and researchers have long-differentiated subtypes of lung cancer based on the type of cell that has become cancerous. These are broadly defined as small-cell lung cancer (SCLC) and non-small-cell lung cancer (NSCLC). SCLC is very aggressive. It makes up 15% of all cases and has a 5-year survival rate under 10%. This type of lung cancer responds well to chemotherapy but spreads rapidly and is difficult to treat when it has moved extensively. NSCLC makes up the rest of the cases, 85%. There are several subtypes, including squamous cell and large cell carcinoma and adenocarcinoma, the most common type. NSCLC has a multi-step process and can be caught early when cells are replicating or grouping together but are not yet cancerous. This type of lung cancer does not respond as well to chemotherapy. Surgery or surgery combined with chemotherapy is usually recommended. So what can we do about lung cancer? First and foremost, if you don’t already have lung cancer, make sure you STOP SMOKING. There are programs, medications, and support groups that may help. Non-smokers should also be aware of the risks and symptoms. Beyond that, early detection is critical. Cancer can be localized in only one organ, spread to the lymph nodes, and eventually spread throughout the body. When lung cancer is localized, 5-year survival rates are over 50%. When it has metastasized and spread to other locations, that survival rate drops below 5%. If you are at risk, inquire with your doctor about lung cancer screenings and be vigilant. If you currently have lung cancer, your doctor has the best information available for your specific case. Treatments include surgery and chemotherapy, along with radiation therapy, immunotherapy, laser therapy, stents, and experimental treatments. Though ENCORE Research Group sites do not currently have any lung cancer trials enrolling, we know this is a critical matter for many people. Follow this link for lung cancer clinical trials that may be in your area: clinicaltrials.gov/ct2/results?cond=lung+cancer. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Schabath, M. B., & Cote, M. L. (2019). Cancer progress and priorities: lung cancer. Cancer epidemiology, biomarkers & prevention, 28(10), 1563-1579. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6777859/ NIH National Cancer Institute Non-Small Cell Lung Cancer Treatment (February 17, 2023) https://www.cancer.gov/types/lung/hp/non-small-cell-lung-treatment-pdq NIH National Cancer Institute Small Cell Lung Cancer Treatment (March 2, 2023) https://www.cancer.gov/types/lung/hp/small-cell-lung-treatment-pdq NIH National Cancer Institute What is Cancer? (October 11, 2021) https://www.cancer.gov/about-cancer/understanding/what-is-cancer
Scroll down to listen to this article.
Listen to the article here:
It’s hurricane season, which means time to break out the big wave surfboard, your best surf leash, and maybe your evacuation kit. Hurricanes are unusual as natural disasters go because, thanks to modern technology, you can actually prepare for them. The advanced notice and frequent shifts in hurricane paths can lead to some strange behaviors, where we tire of preparing and ignore the warnings. For your safety, we recommend you adhere to all warnings and directives from federal and state agencies regarding a hurricane. We also recommend you plan for what may happen before, during, and after a storm passes. Knowing what to expect may not save all of your things, but it should help keep the important things (including your health!) safe. Before a storm hits, there is a lot of work to do. Knowing where you will go in the event of an evacuation is very important. It becomes essential if you have pets or special circumstances, as you may be limited in available options. Florida Emergency Management reminds us that the best place to shelter is with friends or family in a safe building outside of the evacuation area. Know where all of your medical information and medicines are located. Plan on what you need to take (don’t forget legal documents!) and what might get left behind (your tote bag collection). Get ready to make preparations for your home, including getting boards for windows if you need them. On the health front, make sure you’re up to date on vaccines, especially flu and tetanus! A mobile health unit reported that 44% of all visits were requests for vaccines after Hurricane Sandy in 2012. While a hurricane hits, you should shelter and stay safe. The middle of the storm is when you hope your preparations have paid off, not a time to check on them. Remember that wind is deadly, floods are deadly, and bridges can be deadly too. If you are planning to surf, don’t. Make sure you stay current with weather updates; a storm radio is very helpful here. You aren’t out of the water just because a storm has passed, literally! Floods can be ongoing, including fresh-water floods from rainfall. Your residence may be damaged, unsafe, or destroyed. Food and healthcare can be difficult to access. Researchers have found that after major hurricanes, healthy foods tend to disappear quickly, while unhealthy alternatives are easily found. They discovered that fruits and vegetables were only found in 50-60% of stores, but sugary sodas were available 90-100% of the time. In addition, healthy options tend to become more expensive. Beyond food, healthcare can become stressful. Many clinics and pharmacies may be closed or restricted. After Hurricane Harvey in Texas, a major hospital had almost 3⁄4 of its beds destroyed, leading to people sleeping on cots. In addition, hospital staff may be exhausted, stressed, and get poor sleep. Remember that they also see their homes destroyed! To top everything off, mental health can be a huge concern. The lead-up to a natural disaster is stressful and anxiety-inducing. The reality of one can be traumatic. Be aware of changes to your mood and attitude; Post-Traumatic Stress Disorder (PTSD) and depression may increase due to trauma or stress. Whatever happens this hurricane season, good preparation and knowledge can help make the unpredictability of storms more manageable. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
References: Chambers, K. A., Husain, I., Chathampally, Y., Vierling, A., Cardenas-Turanzas, M., Cardenas, F., … & Rogg, J. (2020). Impact of Hurricane Harvey on healthcare utilization and emergency department operations. Western journal of emergency medicine, 21(3), 586. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7234707/ Clay, L. A., Slotter, R., Heath, B., Lange, V., & Colón-Ramos, U. (2023). Capturing disruptions to food availability after disasters: assessing the food environment following Hurricanes Florence and María. Disaster Medicine and Public Health Preparedness, 17, e17. https://doi.org/10.1017/dmp.2021.145 Florida Division of Emergency Management (n.d.) Important shelter information https://www.floridadisaster.org/planprepare/disability/evacuations-and-shelters/shelter-information/ Lien, C., Raimo, J., Abramowitz, J., Khanijo, S., Kritharis, A., Mason, C., … & Carney, M. T. (2014). Community healthcare delivery post-Hurricane Sandy: lessons from a mobile health unit. Journal of community health, 39, 599-605. http://dx.doi.org/10.1007/s10900-013-9805-7
Scroll down to listen to this article.
Listen to the article here:
Gout has been called the “disease of kings.” This is in part because of its ancient association with lavish, relaxed lifestyles. It is also in part because the disease is old enough that kings were common. Gout was first identified around 4,600 years ago in Egypt as an affliction of the joints. Since then, it has moved from the disease of kings to that of the common man. Gout affects over nine million Americans. Its underlying partner in crime, elevated uric acid in the blood (hyperuricemia), affects over 32 million. The disease is most common in middle-aged men. There is a genetic component: Mexican Americans have a lower risk than White or Black Americans. In this article, we’ll dig into the nitty gritty of what gout is, how it works, and what we can do about it. On its surface, gout is straightforward. Uric acid forms crystals in the joints, causing arthritic inflammation. Uric acid is commonly and unfairly dismissed as a waste product. It is formed when the body breaks down purines – one of the building blocks of DNA. Purines are found in high levels in the meat and seafood we eat and are also normally produced in the body. Uric acid circulates in our bloodstream, acting as a powerful antioxidant. It cleans things up and is expelled in the urine. Unsurprisingly, urine is where uric acid gets its name. It is protective when it’s in the right places in the body – and at the proper concentrations. When we have too much uric acid, problems begin. At high concentrations, it condenses into sharp, needle-like crystals. These build up in our joints. Let’s pivot for a moment. Why would uric acid concentrations be high? There are two major mechanisms: either we make too much uric acid, or we don’t get rid of it well enough. Creating too much uric acid is actually relatively rare, making up only 10% of cases. It may be influenced by consuming meat, seafood, and beer. Low exercise, high weight, and metabolic syndrome may contribute, as do some cancers and tumors. The vast majority of cases are from an underexcretion of uric acid. This could be from other medicines, kidney issues, alcohol consumption, or genetics. We can have high concentrations of uric acid in the blood and crystals in the joints without other symptoms. This is called asymptomatic hyperuricemia. A- at the front means “not,” so asymptomatic indicates that there are no symptoms. Hyper- indicates “too much,” uric refers to the uric acid, and -emia means “presence in blood.” Asymptomatic hyperuricemia means there is too much uric acid in the blood, but there are no symptoms. The first stage of symptoms takes the form of acute gout attacks. This is where we can see intermittent periods of often very painful symptoms. Uric acid crystals accumulate in the joints, and the body needs to get rid of them. Unfortunately, the body can’t just delete things it doesn’t like and make them disappear forever. Instead, the body uses the immune system. Three major types of cells intervene. Macrophages, also called monocytes, are gigantic immune cells that eat things. Genetic and acquired differences between people can result in different skill levels of macrophages. For many people, the problems stop here; macrophages eat the uric acid crystals, and no problems emerge. Likely these people would have asymptomatic hyperuricemia. For an unlucky subset of people, their macrophages can’t deal with the crystals by themselves, so they call for help using powerful chemicals. These calls bring in mast cells, which sound an alert and release other potent chemicals. These chemicals include histamines, cytokines, and hormones which cause inflammation and sometimes destroy the crystals. With an acute gout attack, however, neutrophils are brought in. Neutrophils are big bad destructobots that follow the chemical trails released by macrophages and mast cells. They come in and smash everything rapidly. This leads to an acute or rapid onset gout attack. It hurts a lot, and they clear out some of the uric acid crystals. After acute gout attacks, it may take a bit for crystals to form again or for an immune response to trigger. This is called the intercritical period and usually has few or no symptoms. Unfortunately, this intercritical period tends to shorten over time, meaning attacks become more frequent. The fourth and final stage of gout is chronic gout. This is a very painful, destructive stage. Crystals form into big, visible deposits called tophi (plural for tophus). A tophus is a swollen area filled with white and chalky uric acid deposits—these form in cartilage, around joints and tendons, and occasionally in the kidneys. The kidneys are in charge of filtering uric acid from the blood, so this creates an accelerating feedback loop. Tophi formation is accompanied by constant joint inflammation. Inflammation chemicals and tophi formation together erode bone and degrade cartilage. This is very painful and gets worse over time. So what can be done? The first and most important is diagnosis. Gout is common but can look like other types of arthritis, so getting accurate labs and imaging is vital. If gout is positively identified, a flare-up might be helped using medication. NSAIDs like aspirin or ibuprofen are widely used but may be dangerous if you have kidney failure, which may be a cause of gout. Colchicine is also contraindicated by kidney failure, as well as many other medications. Steroids work well but come with several side effects. Each of these, as well as off-label choices, can also seriously interact with other medications and should be discussed with your doctor before use. Chronic gout must be treated at a systemic level. Education, such as this exact article you are currently reading, is a significant first step. Consider discussing uricosuric medications in detail with your doctor. Early treatment can be successful, so be vigilant! Lifestyle changes may also help. This includes limiting meat and seafood intake, cutting back on sugary soda and beer, and increasing exercise, vegetables, and possibly vitamin C. Urate-lowering drugs, such as allopurinol, are effective but may come with side effects. These reduce the formation of uric acid or reduce the absorption of it into the bloodstream. By lowering the amount of uric acid in the bloodstream, deposits in joints will start to break down, resulting in painful flare-ups as the uric acid is cleared away. This is painful enough that it is difficult for many patients to stay on their medicine. Hopefully, new medicines will help people break up this painful condition. Though the age of kings is mostly gone, gout can still be a royal pain. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Sources: Nuki, G., & Simkin, P. A. (2006). A concise history of gout and hyperuricemia and their treatment. Arthritis research & therapy, 8(1), 1-5. https://arthritis-research.biomedcentral.com/articles/10.1186/ar1906 Ragab, G., Elshahaly, M., & Bardin, T. (2017). Gout: An old disease in new perspective–A review. Journal of advanced research, 8(5), 495-511. https://doi.org/10.1016/j.jare.2017.04.008 Singh, G., Lingala, B., & Mithal, A. (2019). Gout and hyperuricemia in the USA: prevalence and trends. Rheumatology, 58(12), 2177-2180. https://doi.org/10.1093/rheumatology/kez196
Scroll down to listen to this article.
Listen to the article here:
Have you ever been told not to share a drink with someone? A spoon? A toothbrush? I remember being told if I shared a drink, I might get mono. But what is mono, is it really so bad, what causes it, and what can we do about it? To start, mono is not the real name. The disease is properly termed infectious mononucleosis. The term mononucleosis was first used in the 1920s to describe how some white blood cells, called lymphocytes, grow and have a central nucleus that resembles a different type of cell, a monocyte. Infectious mononucleosis has a few different causes, but 90% of cases are from a single virus; the Epstein-Barr virus (EBV). EBV is part of the herpes family of viruses. This category includes those that cause chickenpox/shingles and genital herpes, but each are their own separate type and can’t change into another. EBV and infectious mononucleosis are very common. Per the NIH, 90% of people can expect to get EBV at some point in their lives. Most of the time we are infected as children and have few or no symptoms. It turns out those cootie shots weren’t working after all. The most common symptoms are very generic: fatigue, fever, sore throat, and swollen lymph nodes. These usually resolve within a few weeks. For some people, however, infectious mononucleosis will persist or lead to complications. These include a rash, liver enlargement, and spleen enlargement. Further issues may develop. The liver and spleen may have problems, including a ruptured spleen if the patient engages in intense physical activities. Additionally, EBV is one of the few viruses that can lead to the development of cancer. Even without severe complications, some cases of mono can last for several weeks. So what is Epstein-Barr virus, and how does it cause problems? EBV is, as the name implies, a virus. These are “organisms at the edge of life” and need to infect host cells to replicate. EBV infects two types of cells, the epithelial cells that line the throat and B lymphocytes, a type of defensive white blood cell. When you are first infected, EBV is in a lytic phase. Lytic is from the Greek for “loosen,” and this stage is where EBV replicates rapidly and causes most of its symptoms. DNA inside the virus is open to being replicated and does so by the thousands and millions. EBV is sneaky, though, because not all of the virus particles do this. Instead, some of these particles bend their DNA into a circle inside of B cells. These B cells don’t “know” they’re infected and go about their business as usual. This is the latent stage. Latent EBV doesn’t reproduce on its own instead, it is copied when a cell splits. Latent EBV presents no symptoms and may even be integrated into our own DNA. Some will die with B cells during normal activity, but we can never be rid of EBV once we catch it. EBV occasionally reactivates and becomes lytic again. Scientists aren’t certain exactly why this happens but think it may be in response to a different infection, where the B cells are called into action. This can increase a person’s risk of developing nasopharyngeal cancer, certain lymphomas, or stomach cancers. Non-cancerous symptoms are caused by swollen, poorly performing B cells and infected cells that line the throat called epithelial cells. So what can we do about infectious mononucleosis and EBV in general? Most of the time, we don’t need to do much. Most cases resolve on their own between 2-6 weeks as the body fights and EBV converts into the latent phase. During this time, treating symptoms at home can help: drink fluids, rest, and take over-the-counter medicine for pain and fever – acetaminophen is commonly used. Rest is very important, even if you don’t feel too fatigued. B cells are produced in the spleen, which can get swollen during infection. High-intensity activity, like sports, can cause it to rupture (not good). For more rare or difficult symptoms, your doctor may prescribe corticosteroids or antivirals. Antibiotics do not work, as EBV is not a bacteria. With potentially serious symptoms and EBV staying in your systems lifelong, prevention would be ideal, but is currently impractical due to the lack of a vaccine. There are also no medicines available to rid your body of EBV. EBV is spread through saliva and other body fluids, so you can get it from sharing a straw, kissing, or getting an organ transplant. There is no approved vaccine against EBV yet, but we are hoping one may be available in the future. Look out for a clinical trial for EBV vaccines to help quench the kissing disease. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Sources: U.S. Department of Health & Human Services/Centers for Disease Control and Prevention (September 28, 2020). About Epstein-Barr Virus https://www.cdc.gov/epstein-barr/about-ebv.html Luzuriaga K, Sullivan JL. Infectious mononucleosis [published correction appears in N Engl J Med. 2010;363(15):1486]. N Engl J Med. 2010;362(21):1993-2000 https://www.researchgate.net/publication/44632890_Infectious_Mononucleosis Odumade, O. A., Hogquist, K. A., & Balfour Jr, H. H. (2011). Progress and problems in understanding and managing primary Epstein-Barr virus infections. Clinical microbiology reviews, 24(1), 193-209. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3021204/ Rybicki, E. (1990). The classification of organisms at the edge of life or problems with virus systematics. South African Journal of Science, 86(4), 182. https://journals.co.za/doi/pdf/10.10520/AJA00382353_6229
Scroll down to listen to this article.
Listen to the article here:
With warm weather upon us many of us are spending time enjoying nature and sunshine. Out in the wilderness we can enjoy blue skies, green trees, and a pain progressing from skin rash to persistent arthritis. Of course we’re talking about Lyme Disease, a growing concern in the United States. Lyme disease cases top 300,000 per year in the US, mostly in the Northeast, and affects mostly children and middle-aged Americans. Lyme disease is spread by one of nature’s grossest bugs, the tick. In case you are lucky enough to be unfamiliar with ticks, they are little arachnids (like spiders) except instead of skittering around and eating flies they hang out in long grasses and grab onto you as you walk by. Then they burrow into your skin and eat your blood while transmitting painful bacteria to your bloodstream. In Blacklegged ticks, one of those bacteria may be Borrelia. This is a little fusilli-looking bacteria with a long, twisted body and some pretty neat tricks. It has little paddles on the outside called flagella that let it swim around inside your body, aiming for nutrients and avoiding alcohol and other things. Borrelia bacteria live in both ticks and mammals, and change their gene expression and what the surface of their body looks like depending on where they are. They wouldn’t be effective invaders, however, if it weren’t for the ticks. Ticks stab a hole through the skin, which lets Borrelia invade. Tick saliva stops clotting and suppresses our immune system. Borrelia bacteria attach bits of tick saliva to their bodies to help evade detection. This makes it extra difficult for the immune system to fight. The bacteria themselves don’t produce toxins or dangerous proteins. When Borrelia bacteria successfully take hold, the immune system uses its major immune weapon: inflammation. Borrelia is difficult to fight, probably because of the tick saliva on the outside. This can make the fight long and painful for us. We call the disease Lyme, after the small coastal town in Connecticut where it was first documented in the 1970s. Lyme disease has three main stages. The early stage is characterized by skin problems around the bite location accompanied with flu-like symptoms. If we are lucky, our immune system wins here and the side effects end. However, many people experience a middle stage of headaches, stiffness, and other problems as the bacteria gets into the nerves and heart. If the bacteria has still evaded the immune system after this, it may hide in the joints, causing arthritis and long-term problems for months or years. So what can we do about Lyme disease? First and foremost, don’t get bitten by ticks! Avoid long grasses and wear long pants, tucking them into your sock or shoes helps to avoid these miniature monsters. Tick repellant also helps. Remove any ticks you find early! It takes around 36 hours for a tick to transmit Lyme disease to you, so being vigilant and removing ticks is critical. You need to remove the entire tick, including the head which is buried in your skin. After you remove a tick, you can kill it by drowning it in rubbing alcohol. It’s not recommended to squash the tick as it could further expose you to disease. If you are unfortunate enough to be bitten by an infected tick, medical help might be needed. The symptoms are caused by our immune system failing to win the fight against Lyme disease. Antibiotics boost our immune response and are highly effective against Lyme if administered fast enough. In later stages antibiotics are still effective but may not clear all symptoms. We believe prevention is the best medicine. An effective Lyme disease vaccine would boost our immune response and prevent Borrelia bacteria from gaining the upper hand. There actually was an effective vaccine in the 1990s, but misconceptions on how Lyme was diagnosed and how the disease worked – along with poor sales – caused the vaccine to be pulled from the market. Related vaccines have been available for dogs for decades but, frustratingly, not people. Perhaps with better education and a new generation of vaccines we can keep Lyme disease from souring our walks in the woods. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Sources: Aronowitz, R. A. (2012). The rise and fall of the lyme disease vaccines: a cautionary tale for risk interventions in American medicine and public health. The Milbank Quarterly, 90(2), 250-277. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3460208/ Steere, A. C., Strle, F., Wormser, G. P., Hu, L. T., Branda, J. A., Hovius, J. W., … & Mead, P. S. (2016). Lyme borreliosis. Nature reviews Disease primers, 2(1), 1-19. https://www.nature.com/articles/nrdp201690
Scroll down to listen to this article.
Listen to the article here:
May 20th is Clinical Trials Day. Of course, we are biased and think it should become a national holiday, but until that day arrives, let’s celebrate the day by studying a clinical trial designed by our founder and CEO, Dr. Michael J. Koren. The trial we will study, published in 2006, was called the Aggressive Lipid-Lowering Initiation Abates New Cardiac Events, or ALLIANCE. In case you are unaware, the sponsors of clinical trials are all very clever and enjoy coming up with neat acronyms. ALLIANCE was a large, 16-center study conducted around the turn of the millennium and enrolled 2,442 patients. All patients had coronary heart disease – blockage of a major blood vessel to the heart. The study was designed to determine the difference in outcomes for patients with coronary heart disease when taking atorvastatin, marketed as Lipitor, at a full dose of 80 mg versus usual treatment with statins or other cholesterol drugs. Patients treated with high dose atorvastatin were monitored to keep their LDL less than 80 mg/dL. Outcomes in a clinical trial are the variables measured: what researchers are monitoring for change. Typical outcomes will include things like changes in symptoms, cure, or death. The ALLIANCE patients had coronary heart disease, so the main outcomes being monitored were: This study was significant because it looked at the difference between medications given in a clinical trial setting and “usual care” for people enrolled in managed care health plans (they all had insurance). The study results were, frankly, amazing. In the “usual care” group, patients saw their average LDL levels drop by over 23 mg/dL, a significant decrease. These are nice results, but the “more aggressively treated” group did even better. They saw LDL levels drop by more than 34 mg/dL, a 50% greater reduction! Furthermore, the aggressive treatment led to 17% fewer events, including a whopping 47% fewer heart attacks! Needless to say, the aggressive atorvastatin treatment was a resounding success. The stated goal of the study was to discover the effectiveness of the investigational medication, but the ALLIANCE study also measured the difference between clinical trials and standard care. The aggressive treatment group received clinical-trial-level care with specialist medical professionals and frequent check-ins. Patients had a lot of contact, and researchers were interested in any and all health changes. The study showed great success for the sponsor. It helped make Lipitor the best-selling medication of all time (recently broken by Humira). It gave us solid evidence that the clinical trial process doesn’t just lead to new potential medications but also potentially better health outcomes for patients. Thanks, Dr. Koren, for taking leadership of this trial and the ENCORE Research Group. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Sources: Koren, M. J., Hunninghake, D. B., & Alliance Investigators. (2004). Clinical outcomes in managed-care patients with coronary heart disease treated aggressively in lipid-lowering disease management clinics: the alliance study. Journal of the American College of Cardiology, 44(9), 1772-1779. https://www.sciencedirect.com/science/article/pii/S0735109704016365
Scroll down to listen to this article.
Listen to the article here:
Sometimes when I’m desperately trying to fall asleep I instead think of all the things that might kill me. Alligators, drunk drivers, hurricanes, and running out of cookies usually top the list. Do you know what doesn’t top the list? High blood pressure. It really should though. High blood pressure is a leading preventable cause of premature death, affecting well over a billion people worldwide and causing upwards of 9 million deaths a year. Maybe the alligators can chew on those facts for a while. So what is high blood pressure, why is it such a big deal, why do we get it, and what can we do? High blood pressure is exactly what it sounds like; when the blood in your arteries is being forced through more strongly than normal. The medical name for high blood pressure is hypertension. Hyper– means over or above, and -tension, in this case, indicates the stress of your arteries. Hypertension is excessive stress on your arteries. Blood pressure can be split into two numbers, systolic and diastolic. These refer to the action of the heart, where systolic is the contracted, pumping blood pressure, and diastolic is the relaxed blood pressure. When you get your blood pressure checked, these are reported as two numbers “over” each other. A reading of 140/90 mmHg or higher is high blood pressure, but there is an increased risk of complications with blood pressure above 120/80 mmHg. High blood pressure is particularly dangerous. It is easy to see why: the bloodstream is how we deliver oxygen to the cells, and it touches every cell in the entire body. Two of the biggest dangers with elevated blood pressure are ischemic heart disease and stroke, conditions where the blood supply doesn’t reach the heart or brain. High blood pressure can also cause brain bleeds, chronic kidney damage, and other types of heart damage. All of these organs are vital to our survival, so a condition that potentially damages all of them is life-threatening. What are the causes of high blood pressure? High blood pressure is calculated the same as in any pipe at its most basic level. The amount of blood coming out of the heart is counteracted by the resistance from the arteries. More output or more resistance makes blood pressure rise. High blood pressure on its own isn’t bad, it’s adaptive for critical situations. When we see a lion and it charges us, we become stressed and initiate the sympathetic nervous system, also known as fight, flight, and freeze. Part of this system’s job is to constrict blood vessels and raise the heart rate to deliver large amounts of oxygen to cells. We see damage when we have high blood pressure for long amounts of time. Some body systems that cause prolonged elevations in blood pressure are: These are the major players in primary or essential hypertension. Secondary hypertension is caused by another identifiable disease, like kidney disease. So what can we do? Some outcomes depend on things we can’t easily change, like access to quality healthcare and blood pressure medication. Many lifestyle options can be changed to improve our blood pressure: Even though we have good evidence for lifestyle changes lowering blood pressure, the biggest difference between countries in terms of controlling blood pressure is access to medicine. Blood pressure medicines have saved countless lives and helped stem the blood tide of hypertension. There are several types of blood pressure medicines on the market. Diuretics get rid of sodium and water in the blood. Angiotensin-converting-enzyme (ACE) inhibitors and Angiotensin-receptor blockers (ARB) help ease inflammation, relax the blood vessels, and keep them from constricting. Calcium channel blockers reduce heart rate. These all have side effects, but the biggest challenge with them is that they are daily oral medications, which can be forgotten, missed, or hard to adhere to. Longer-term solutions are in clinical trials and may be available to you if you qualify. So don’t sleep on your high blood pressure. Check with your local ENCORE Research office to see what studies are enrolling. See ya’ later, alligators! Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Sources: Harrison, D. G., Coffman, T. M., & Wilcox, C. S. (2021). Pathophysiology of hypertension: the mosaic theory and beyond. Circulation research, 128(7), 847-863. https://www.ahajournals.org/doi/full/10.1161/CIRCRESAHA.121.318082 Lifton, R. P., Gharavi, A. G., & Geller, D. S. (2001). Molecular mechanisms of human hypertension. Cell, 104(4), 545-556. https://doi.org/10.1016/S0092-8674(01)00241-0 Mills, K. T., Stefanescu, A., & He, J. (2020). The global epidemiology of hypertension. Nature Reviews Nephrology, 16(4), 223-237. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7998524/
Listen to the article here:
Clinical research is vital in developing knowledge geared toward improving future health practices. It is often the only feasible solution to medical conditions where standard treatment has failed. Research can be groundbreaking and progressive but study populations lack diversity, especially regarding demographics such as race, ethnicity, age, and sex. Which begs the question: “Why is diversity important to research?” Simply put, various subsets of people can process the same medication differently. Through the clinical research process (guided by strict safety protocols), researchers gather data on how participants experience the same investigational product (IP). Suppose a clinical trial includes people from many different age, gender, and racial/ethnic groups. In that case, researchers will then have data on how several groups of people respond to the same product based on those differences. When these new products reach the market, doctors will know what works best, what doesn’t, and for whom based on those findings. Through research, doctors learned that it is best to prescribe particular medications based on patients’ ethnicity/racial background when treating hypertension. As we move forward, the clinical research community thrives on increasing the participation of all minority age, gender, and racial/ethnic groups to improve the safety profile of medical products. The US government must lead this effort through legislation. At ENCORE, we recognize that to benefit the communities we serve, we must take the steps necessary to best represent ALL in the trials we conduct. However, this requires overcoming numerous challenges, including long-standing mistrust and economic barriers which prevent minority groups from accessing and participating in research. Even though clinical trials have evolved from historically unethical practices involving minority racial groups to a transparent process where participant safety and protection are paramount, there is still a significant lack of trust on the part of potential study subjects. Especially for those who are dubious, establishing credibility and integrity within clinical research practice is crucial to growing minority group participation. We believe that physicians, especially those who serve ethnically/racially variant communities, play a significant role in achieving Diversity in clinical trials by bridging trust between researchers and minority participants. ENCORE physicians have dedicated their efforts to working alongside primary care physicians and specialists who serve these communities; to provide them with research material relevant to their practice. Doctors then have the information to make informed recommendations on whether a particular clinical trial is appropriate for their patients. Not only are people more likely to be confident in the recommendations coming from their doctors, but doctors find themselves better prepared to help patients who have failed on current therapeutic approaches. Unlike when seeking intervention via traditional means, economic hindrance isn’t a preventative factor when one chooses to participate in clinical research. Healthcare costs are a significant burden to many; however, all of the investigational medical products available here at ENCORE cost our patients nothing. All study-related materials, evaluations, blood tests, and imaging are done for free. Study participants will never be billed. Sponsors such as pharmaceutical companies, governments, and foundations fund medical research through study grants. Grants provide the funding to conduct studies at local research sites, so the cost is not transferred to the volunteers. This allows people experiencing financial constraints or without health insurance the opportunity to receive potentially groundbreaking medical treatment at no cost to them. A small monetary compensation is often provided for participants’ time and inconvenience associated with participating in a clinical study. Payment is kept within a reasonable amount to prevent enticement and undue influence on participants. Despite these steps, we recognize that much more needs to be done to garner diverse research participants in all our trials. Appropriately representing Diversity in clinical trials is an ethical and medical obligation that bounds all stakeholders. Critical players like research sponsors, investigators, referring physicians, coordinators, recruiters, and patients must work collaboratively to achieve this goal. A multi-level stakeholder approach can be more successful than one which addresses a single barrier or involves individual stakeholders. As a research facility, our responsibility in achieving increased Diversity amongst trial participants will build on our investments towards nurturing long-standing relationships. These relationships are between sponsors, community members, our diverse pool of staff and physicians, and our commitment to engagement and learning from diverse patient groups. With this approach, we are confident that trial enrollment will continue to become more diverse and result in a more accurate representation of the people that products are intended to treat. Albertha V. Lalljie, MBBS, MPH
Alzheimer’s Disease is a devastating brain disorder that gets worse over time. Early onset Alzheimer’s occurs before age 65. Most early Alzheimer patients develop symptoms in their 40s and 50s with some particularly aggressive forms starting as early as the late 20s. Any form of Alzheimer’s is a tragedy, but early onset Alzheimer’s can be particularly cruel. We do not know exactly what causes Alzheimer’s Disease. We do know that there are genetic and environmental causes that seem to mix with a high amount of randomness. We also know that some diseases exist alongside Alzheimer’s and may be risk factors. These include diabetes, hypertension, cholesterol issues, and metabolic syndrome. Alzheimer’s produces a number of terrible symptoms: Together, these symptoms combine into cognitive decline, loss of independence, and death. Early onset Alzheimer’s can have these symptoms, but is also more aggressive with shorter lifespan and larger changes in the brain. Interestingly, up to a quarter of patients with early Alzheimer’s may develop cognitive decline without memory loss. This can present as trouble with: We are still uncertain how genetic and environmental conditions translate into Alzheimer’s but the leading theory involves an accumulation of protein in the brain called amyloid plaques and tau tangles. Amyloid plaques are a buildup of a protein between neurons. It is thought that this buildup somehow causes the accumulation of tau inside of neurons. Tau is another protein that folds incorrectly and tangles up inside of neurons, leading to their eventual death. It has been very difficult to study the root causes of Alzheimer’s. This is in large part because of the inconsistency of who gets it. This also means that creating medications for Alzheimer’s has been difficult. One of the most promising avenues for study has been targeting amyloid plaques for disposal by the immune system. With luck, research can pin down a treatment to help slow or even stop the march of early Alzheimer’s. If you would like to be screened for Alzheimer’s, a free Memory Assessment is available at the Jacksonville Center for Clinical Research at 4085 University Boulevard, South, Suite 1, Jacksonville, FL 32216. Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Sources: Ayodele, T., Rogaeva, E., Kurup, J. T., Beecham, G., & Reitz, C. (2021). Early-onset Alzheimer’s disease: what is missing in research?. Current neurology and neuroscience reports, 21, 1-10. https://link.springer.com/article/10.1007/s11910-020-01090-y Mintun, M. A., Lo, A. C., Duggan Evans, C., Wessels, A. M., Ardayfio, P. A., Andersen, S. W., … & Skovronsky, D. M. (2021). Donanemab in early Alzheimer’s disease. New England Journal of Medicine, 384(18), 1691-1704. https://www.nejm.org/doi/full/10.1056/NEJMoa2100708 Reitz, C., Brayne, C., & Mayeux, R. (2011). Epidemiology of Alzheimer disease. Nature Reviews Neurology, 7(3), 137-152. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3339565/
Listen to the article here:
Sugars are sweet, tasty, and disastrous for your health in large quantities. They are also ubiquitous in modern society. We find them added to everything from salad dressings, drinks, bread, even peanut butter! Sugars and other carbohydrates make up over half of the calories consumed by Americans. Carbohydrates are broken down into a simple sugar called glucose and delivered around the body after eating. This can be surprisingly tricky. Too little glucose and cells can’t function. Too much and it gets converted to fat and damages the metabolic system, heart, and bloodstream. Type 1 Diabetes is a condition where the body doesn’t produce enough insulin. Type 2 Diabetes is more complicated; the body doesn’t respond to raised glucose in the bloodstream properly. A big culprit for failure is when insulin isn’t released well. To remedy this a class of drugs called glucagon-like peptide-1 (GLP-1) agonists have been developed. Agonist in this case means the medication has a similar function to the natural hormone. The opposite is an antagonist, which acts in opposition to them. GLP-1 medicines include Trulicity, Mounjaro, and semaglutide / Ozempic. In this article, we will review how insulin works, how GLP-1 works on the cellular level, and what GLP-1 medicines do to the body. Insulin is the main hormone that tells your body how to process sugar. Before we can understand how GLP-1 works, we need to understand the healthy release of insulin. This starts in the pancreas, an organ near our gut. The pancreas is filled with many types of cells called islet cells. These are responsible for regulating the balance of glucose in our bloodstream. Two major types are alpha and beta islet cells. Alpha islet cells produce glucagon and GLP-1. Glucagon tells the liver to increase blood sugar when you need energy. Beta cells make insulin and amylin, which help lower blood sugar. Alpha and beta islet cells work in opposition. They keep each other in check and our blood sugar levels just right. In Type 1 Diabetes, alpha cells may be dysfunctional and beta cells don’t exist or get destroyed. WIth Type 2 Diabetes, problems can occur when beta cells don’t function properly. Beta cells make insulin and release it in two stages. When these cells detect high blood glucose, they “trigger” and release insulin right away. This short response lasts 10-20 minutes, but is still several steps long. After triggering, a complicated “amplifying” pathway turns on to produce and release more insulin. Together this is powerful, slow, complex and has many potential points of failure. Beta cells are vital, and when they fail it often signals the transition from obesity to Type 2 Diabetes. GLP-1 is like a shortcut for beta cells. When it is detected the triggering response is primed and the cells are ready to release insulin as soon as glucose is detected. This pathway bypasses a lot of the complicated cellular machinery that is damaged in diabetic patients. The upshot is that GLP-1 stimulates insulin release from islet cells. An added benefit is that the insulin is only released in the presence of elevated glucose. This is good because you don’t release too much insulin, which can be dangerous. GLP-1 medications also last much longer in the body than natural GLP-1, giving longer-term effects which can last for up to a day! Now we know a little of how GLP-1 acts inside our cells, but what effects does this have on the body? Many, and widespread, it turns out! GLP-1 affects cells all over the body. The three biggest effects are decreased blood glucose, appetite suppression, and weight loss. Insulin decreases blood glucose, and GLP-1 increases the response to glucose. But GLP-1 medications have a secret extra benefit. Remember that alpha and beta cells work opposite each other. Normally when blood sugar is low, we release GLP-1 from our pancreas along with glucagon. Glucagon is very useful, and one of its uses is to stimulate the liver into producing more blood sugar. GLP-1 medications suppress glucagon production and the liver stays quiet. The pancreas still releases insulin, but the liver produces 45% less glucose! GLP-1 affects two of the biggest portions our appetite: our stomach and our brain. It slows the absorption of nutrients from the stomach, a process called gastroparesis. Food – and the glucose inside – is retained in the stomach and gut instead of the bloodstream. GLP-1 can also affect the brain. It can cross from the bloodstream into the brain, but also affect the vagus nerve – the major nerve connecting the brain and gut. Here it acts on the hypothalamus, suppressing the appetite and giving you feelings of being full. With the stomach slowing down and the brain signaling that it’s full, we tend to eat less. Combined, lower blood sugar and appetite can have serious effects on weight. This can be a big benefit of GLP-1 medications. Weight loss is linked with better outcomes for Type 2 Diabetes patients. Getting to a healthy weight is also good for the heart, joints, liver, and so on. Significant weight loss has been seen with GLP-1. Let’s not sugar-coat this though; not all weight loss is created equal. Ideally we’d cut our body fat while maintaining – or building – our muscle. This is especially true with diabetes, as skeletal muscle uses up extra glucose. Unfortunately, when we lose weight through diet restriction we lose more than just fat. This is true of gastric surgery, diet-induced weight loss, and GLP-1 medications. In GLP-1 medication studies, 20-50% of the weight lost is things other than fat – including muscle. Studies vary widely. The type of GLP-1 medication and other medications patients are taking may affect this. The best way to offset this is through building muscle with exercise! GLP-1 medications are truly amazing. They increase insulin response, lower blood glucose, suppress appetite, and lead to weight loss. It’s not all sugar and spice, however. Side effects can be rough, including vomiting and diarrhea. Additionally, meds can’t do it alone. When taking GLP-1 medications, the goal should still be to create an environment conducive to healthy living. Limiting carbohydrate intake is one critical step. Exercising is another. When fighting weight loss, victory is very sweet, but our diets shouldn’t be! Written By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Campbell, J. E., & Newgard, C. B. (2021). Mechanisms controlling pancreatic islet cell function in insulin secretion. Nature reviews Molecular cell biology, 22(2), 142-158. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8115730/ Cervera, A., Wajcberg, E., Sriwijitkamol, A., Fernandez, M., Zuo, P., Triplitt, C., … & Cersosimo, E. (2008). Mechanism of action of exenatide to reduce postprandial hyperglycemia in type 2 diabetes. American Journal of Physiology-Endocrinology and Metabolism, 294(5), E846-E852.https://journals.physiology.org/doi/full/10.1152/ajpendo.00030.2008 Cohen, E., Cragg, M., deFonseka, J., Hite, A., Rosenberg, M., & Zhou, B. (2015). Statistical review of US macronutrient consumption data, 1965–2011: Americans have been following dietary guidelines, coincident with the rise in obesity. Nutrition, 31(5), 727-732. https://pubmed.ncbi.nlm.nih.gov/25837220/ Drucker, D. J. (2018). Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell metabolism, 27(4), 740-756. https://www.sciencedirect.com/science/article/pii/S1550413118301797 Dungan, K., & DeSantis, A. (2013). Glucagon-like peptide-1-based therapies for the treatment of type 2 diabetes mellitus. https://www.uptodate.com/contents/glucagon-like-peptide-1-based-therapies-for-the-treatment-of-type-2-diabetes-mellitus#H1 Baggio, L. L., & Drucker, D. J. (2014). Glucagon-like peptide-1 receptors in the brain: controlling food intake and body weight. The Journal of clinical investigation, 124(10), 4223-4226.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4191040/ Sargeant, J. A., Henson, J., King, J. A., Yates, T., Khunti, K., & Davies, M. J. (2019). A review of the effects of glucagon-like peptide-1 receptor agonists and sodium-glucose cotransporter 2 inhibitors on lean body mass in humans. Endocrinology and Metabolism, 34(3), 247-262. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6769337/
Listen to the article here:
They say in stressful situations you should take a breath and calm down, but what if you literally can’t? Asthma is a common disease that affects around 25 million Americans. It results in several million ER visits and hundreds of thousands of hospitalizations yearly. It can also get worse over time. So what is asthma, how does it cause trouble, and what can we do about it? Take a deep breath as we dive in. To start, asthma is a medley of several related conditions that can be divided in many ways. Into allergic and non-allergic, eosinophilic and neutrophilic, adult onset, asthma with persistent airflow, asthma with obesity, and severe asthma. Several of these categories overlap and make a big mess of everything. The common threads between all types of asthma are the symptoms. Asthma is defined by its symptoms: A collection of symptoms are needed to diagnose asthma; a single symptom isn’t enough. Symptoms are also variable, getting worse at night, in the morning, or in response to a stimulus. Stimuli include irritants, allergens, exercise, infection, and weather. A pattern of symptoms in response to irritants may lead to an asthma diagnosis. Our need to breathe makes this a dangerous disease. Asthma symptoms are variable, but they all involve the airway. The airway is affected in three ways: inflammation, bronchial hyperresponsiveness, and structural remodeling. Inflammation is complicated. In allergic asthma, immune cells respond to dust, pollen, and other airborne items. These are detected by defense cells in our windpipe which mistake them as dangerous. Immune cells act quickly to try and kill the “invaders”. In asthma, the big guns are brought in. Eosinophils and neutrophils are like a bazooka: highly effective at killing invaders, but can cause area-of-effect damage when used improperly. Eosinophils cause bronchial hyperresponsiveness, impaired throat function, inflammation, phlegm, and long-term allergen sensitivity. Eosinophils can also occur in non-allergic asthma. They might get involved because of genetic predisposition, polyps, viruses, and fungi. Neutrophils are similar to eosinophils in causing inflammation, but cause more severe symptoms. They generally need more irritants to activate and can be triggered by tobacco smoke, pollutants, microbes, and obesity. You can have eosinophilic or neutrophilic asthma, or both at the same time. Whatever the flavor, inflammation is the result. One of the effects of inflammation from eosinophils and neutrophils in the throat is bronchial hyperresponsiveness. Bronchial refers to the windpipe, hyper- means abnormally high, and responsiveness in this case refers to how narrow the throat gets. Bronchial hyperresponsiveness is an abnormally high constriction of the throat in response to stimuli, such as irritants. The responsiveness is temporary, leading to the characteristic variability in symptoms. Long term inflammation can cause persistent damage, called airway structural remodeling. This is when the cells of the airway grow in different ways. The walls of the airway are thickened, there is more muscle mass in the throat, the throat contracts harder, and the airway is reduced in size. This is a more permanent change in our throat, making this a long-term effect. The symptoms are very constricting, is there relief? Yes! Eosinophils respond well to anti-inflammatory medicines known as corticosteroids, like cortisone. These are used for both long-term control and for asthma attacks. Unfortunately, these don’t work on neutrophils, and can actually prolong their lifespan, exacerbating symptoms. Bronchodilators open airways and reduce swelling. Allergy-induced asthma may also be alleviated using allergy shots, tablets, or medications. Newer medicines include monoclonal antibodies that target allergens or specific cells for destruction. Medicines that directly target eosinophils or neutrophils might provide a deeper relief from asthma. Don’t hold your breath, but keep an eye out for new research opportunities! Written By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Cockcroft, D. W., & Davis, B. E. (2006). Mechanisms of airway hyperresponsiveness. Journal of allergy and clinical immunology, 118(3), 551-559. https://www.jacionline.org/article/S0091-6749(06)01511-9/fulltext Global Initiative for Asthma. (2000). Global Strategy for Asthma Management and Prevention updated 2022. www.ginasthma.org. Pate, C. A., Zahran, H. S., Qin, X., Johnson, C., Hummelman, E., & Malilay, J. (2021). Asthma surveillance—United States, 2006–2018. MMWR Surveillance Summaries, 70(5), 1. https://www.cdc.gov/mmwr/volumes/70/ss/ss7005a1.htm?s_cid=ss7005a1_w Pelaia, G., Vatrella, A., Busceti, M. T., Gallelli, L., Calabrese, C., Terracciano, R., & Maselli, R. (2015). Cellular mechanisms underlying eosinophilic and neutrophilic airway inflammation in asthma. Mediators of inflammation, 2015. https://www.hindawi.com/journals/mi/2015/879783/
Listen to the article here:
All diseases are different. Some are immediately apparent, like a heart attack. Some have the gall to hide undetected for years. This might sound nice, but the damage that can be done while undetected gets worse over time. Primary Biliary [billy-ur-ee] Cholangitis [kow-luhn-jai-tuhs] (PBC) destroys our bile ducts, often without our knowledge until other parts of the body are damaged. PBC is a somewhat rare disease, affecting 1 in every 3-4 thousand people, so around 100,000 Americans. Of these, around 90% of cases are in women. Most patients with PBC are diagnosed in their 50’s and 60’s, though the disease may start as young as 30. On its own, PBC may not have many symptoms, but leads to debilitating conditions of the liver such as cirrhosis, failure, and cancer. It also causes downstream damage across the body such as metabolic bone disease and malabsorption of nutrients. So what is Primary Biliary Cholangitis? There are clues in the name. The biliary system carries bile, a digestive fluid produced in the liver and sent to the gallbladder and intestines. Chol- also means bile, ang- means vessel, and -itis means inflamed. Cholangitis means the tubes that carry bile from the liver (called bile ducts) are inflamed. This disease is termed “primary” because it is the direct cause of inflammation and damage. A “secondary” disease is one caused by previous infection or disease; bile ducts can also be damaged by chemotherapy or surgical trauma to the lower bile system, for example. Altogether, primary biliary cholangitis is a disease that directly causes inflammation and damage to bile ducts. There are many bile ducts and many kinds of bile ducts, with the smallest being ultra-fine and located throughout the liver. These collect digestive fluid and transport them to ever bigger ducts to be stored in the gallbladder and sent to the digestive tract. In PBC, these small ducts are destroyed. A good rule of thumb is that when digestive fluid isn’t going to the digestive tract there may be problems. The buildup of bile damages the liver over time. Bile is critical for digesting fats and many vitamins. When bile fails to be de-livered to the digestive tract we may suffer malnutrition and fatigue. Most PBC patients are symptom-free but several experience debilitating symptoms, especially at later stages. Major symptoms are fatigue and itching (called pruritus). Jaundice, skin pigmentation, and fat buildup under the skin are other potential problems. Since so many people have no symptoms, or vague ones that can be attributed to other things, PBC is detected by looking at the blood. The primary evidence is the presence of antimitochondrial antibodies. These are immune system proteins that target mitochondria, the powerhouse of the cell. Increased antimitochondrial antibodies give us a good clue as to the true nature of primary biliary cholangitis. PBC is an autoimmune disorder – our immune system attacking healthy cells in the body. The cells at hand are the ones that make up the bile ducts. How this happens is complicated, and not fully known. We do know that there is a strong genetic component. X marks the spot in this case; since it affects mostly women, the X chromosome is a good candidate for where the trouble lies. The genetics aren’t enough, however. PBC requires an environmental component. Environmental in this case means anything that started outside of our own bodies and got in. Environmental risks include things that aren’t alive, like nail polish, hair dye, cigarettes, and toxic waste. Here at ENCORE Research Group we recommend avoiding toxic waste sites whenever possible. Living environmental factors include bacteria that degrade the immune system. This is a slow process. The bile duct cells become affected and some die. As they die they present parts of their mitochondria to the immune system, which learns to attack them. Eventually, the immune system starts attacking bile duct cells directly, causing scarring and cell death. This causes the eventual collapse of the small bile ducts. So what can be done? We can’t fight the underlying autoimmune disease yet. Current treatments are aimed at restoring the function of bile. The major medication is ursodeoxycholic [er-sudi-oxy-cholic] acid (UDCA), as synthetic bile acid. This only helps 60% of the time, and may be supplemented with obeticholic [oh-bet-i-colic] acid (OCA) to aid in the process. Neither of these help with symptoms. Itching may be treated with creams and cold water, and fatigue is treated with exercise, occupational, and physical therapy. Sicca, meaning dry eyes and mouth, is also a symptom, and is treated with artificial tears and saliva, or medications that increase these. Future treatments would target the underlying immune response or the associated inflammation. Either way, a treatment that stops damage is needed to help sufferers of PBC – and to keep those that aren’t suffering feeling well! Written By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Dauphinee, J. A., & Sinclair, J. C. (1949). Primary biliary cirrhosis. Canadian Medical Association Journal, 61(1), 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1591584/?page=1 Lleo, A., Invernizzi, P., Mackay, I. R., Prince, H., Zhong, R. Q., & Gershwin, M. E. (2008). Etiopathogenesis of primary biliary cirrhosis. World journal of gastroenterology: WJG, 14(21), 3328.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2716587/ Onofrio, F. Q., Hirschfield, G. M., & Gulamhusein, A. F. (2019). A practical review of primary biliary cholangitis for the gastroenterologist. Gastroenterology & hepatology, 15(3), 145. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6495411/ Ruemmele, P., Hofstaedter, F., & Gelbmann, C. M. (2009). Secondary sclerosing cholangitis. Nature Reviews Gastroenterology & Hepatology, 6(5), 287-295. https://www.nature.com/articles/nrgastro.2009.46 Strazzabosco, M., & Fabris, L. (2008). Functional anatomy of normal bile ducts. The Anatomical Record: Advances in Integrative Anatomy and Evolutionary Biology: Advances in Integrative Anatomy and Evolutionary Biology, 291(6), 653-660.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3743051/
Listen to the article here:
Sticks and stones may break my bones, but words can never hurt me. But what if words could hurt you? Meet the nocebo effect, the evil twin of placebo. The nocebo effect is an increase in negative symptoms in response to patient expectations. This occurs in both clinical trials and normal clinical care. In clinical trials, this frequently presents as adverse events occurring during a placebo administration (such as a sugar pill instead of a blood pressure med), but it’s important to note that nothing needs to be administered for an increase in symptoms. Nocebo effects may sound like no big deal, but symptoms can be significant. In clinical trials, 4-26% of patients who discontinue medication do so because of nocebo reactions. Unfortunately this burden isn’t evenly spread. Women experience an outsized effect, as do those suffering from certain psychiatric illnesses, such as anxiety and depression. Furthermore, both pessimistic and type A individuals experience higher rates of nocebo effect. So how does it work, and are the effects real? Nocebo effects are due to our own expectations. When a doctor, nurse, or researcher states the potential side effects for a medication or procedure, patients are more likely to experience those effects. This has been shown in several anecdotal settings, but also in multiple research studies. During the COVID clinical trials, patients were reporting serious side effects that tracked popular media descriptions – even when they were given saline instead of the real vaccine! These effects show the power of negative expectations, one of the three psychological mechanisms underpinning the nocebo effect. Negative results are a direct result of expectations. Researchers in one study tested the effect of word phrasing on pain outcomes. When pregnant women were preparing to get an anesthesia injection the researchers talked them through what might happen. Half the patients were given the standard spiel, “You are going to feel a big sting and burn in your back now”. The other half were given the same information in much more neutral language: “We are going to inject the local anesthetic that will numb the area.“ The neutral language group experienced significantly less pain during the injection – just from phrasing! Scientists think the negative expectations might increase focus on symptoms. The expectations don’t have to come just from doctors or nurses, however. Seeing someone else suffer a side effect or hearing stories can produce the same effect! Two other psychological underpinnings for the nocebo effect are less direct. Misattribution is the blaming of normal aches and pains to a new medicine. Progressive disease effects can also be misattributed to a placebo medication. Finally, conditioning has a large effect. Conditioning is the long-term associations we make between seemingly related things. Some patients feel nauseous at the smell of a hospital, for instance. This can also be very specific; the color of a pill can induce distinct side effects. Patients taking blue sugar pills are more likely to experience and report drowsiness than those taking pink sugar pills. Psychology shows us the framework for understanding what’s happening, but what’s going on under the hoodie? Our brains experience changes at suggestions. Scientists think these changes may be due in large part to anticipatory anxiety. Anticipatory anxiety activates at least two pathways in the brain: pain and stress. Part of the pain pathway is called the CCKergic pronociceptive [pro-no-si-cep-tive] system. It is activated by a peptide called cholecystokinin [kow·luh·si·stuh·kai·nuhn] (CCK), and increases our perception of pain at the spinal level. This undermines anesthesia and increases our feelings of pain. The stress pathway moves through a few brain regions along the hypothalamus–pituitary–adrenal (HPA) axis and produces cortisol. Cortisol is a hormone that causes all of the classic signs of stress – increased heart rate and blood pressure, sweating and breathing, among others. The activation of these two major pathways primes our brain and bodies to experience worse symptoms – especially those we are expecting. So what can be done? Well, reading this article is a great start! Around 75% of patients haven’t heard of or don’t believe in the nocebo effect, even though they experience it. Thinking about risks in terms of percentages instead of raw numbers can help. Four in a thousand may increase anxiety more than 0.4%.Other methods may be in the hands of medical professionals. Positive framing, such as with the injection example above, can make a lot of difference. In addition, identifying risky patients may help with how information is presented. Fortunately, understanding the mechanistic nature behind the nocebo effect can help lessen your anxiety – and symptoms! Written By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Kong, J., Gollub, R. L., Polich, G., Kirsch, I., LaViolette, P., Vangel, M., … & Kaptchuk, T. J. (2008). A functional magnetic resonance imaging study on the neural mechanisms of hyperalgesic nocebo effect. Journal of Neuroscience, 28(49), 13354-13362. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2649754/ Planès, S., Villier, C., & Mallaret, M. (2016). The nocebo effect of drugs. Pharmacology research & perspectives, 4(2), e00208. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4804316/ Varelmann, D., Pancaro, C., Cappiello, E. C., & Camann, W. R. (2010). Nocebo-induced hyperalgesia during local anesthetic injection. Anesthesia & Analgesia, 110(3), 868-870. https://doi.org/10.1213/ANE.0b013e3181cc5727
Listen to the article here:
Obesity is a big medical concern. It is when there is an excessive amount of fat that causes medical problems. It is usually defined using the Body Mass Index, or BMI. BMI is a very crude calculation determined only by height and weight. In the USA, “overweight” is defined as a BMI over 25 kg/m2, and “obese” is over 30. This measurement is simplistic and does not take into account any nuance. For example, the CDC has found that the average American male is 5’9” and just under 200 lbs. This gives a BMI of 29.4, which is overweight. Arnold Scwartzenneger is 6’2”. At his peak performance, he weighed around 235 lbs, giving him a BMI of 30.2, which is classified as obese. Independent tests, however, have found that the average male has 28% body fat, whereas Arnold was at 8%. Nuances aside, BMI is an important calculation. If the main measurement for obesity can give silly results, does that mean obesity is a made-up condition? Absolutely not. Obesity causes and makes several medical conditions worse. Four major mechanisms cause damage: inflammation, stress, fat, and weight. Inflammation can lead to diabetes, cancer, infertility, polycystic ovary syndrome (PCOS), and more. Stress is bad for many body systems, including mental health. Increased fat (also called lipids) can lead to liver damage. Stress and increased fat together can increase the chances of blood vessel damage, high blood pressure, heart attack, and stroke. Finally, the pressure of weight itself can degrade joints, squeeze organs, damage the kidneys, and constrict blood vessels. So what causes obesity? At its simplest level, weight gain is caused by consuming more calories than you need. The reasons why some people can’t burn all of the calories can be vastly more complex. They can be broadly lumped into four categories: environmental, genetic, inflammatory, and brain-based mechanisms. Environmental causes happen outside of the body. These include low exercise, a sedentary lifestyle, poor diet, and some medications. Eating disorders can be inherited, though the mechanism is unknown. The genetic factors of obesity are very complicated. There are over 200 genes that may affect obesity. To make matters worse, your body alters parts of the genetic code in response to environmental factors. This process, called epigenetics, complicates things a lot. On top of these two, inflammation is a big risk. Inflammation can lead to conditions such as metabolic syndrome and insulin resistance which affects how the body processes energy. Energy mismanagement on a systemic or cellular level is very hard to fight. Brain-based mechanisms are complicated, but very powerful. We must first remember that some brain functions are specialized for a bygone time. Our brains are biased to ensure we are safe in times of scarcity, not times of plenty. This can lead to trouble in our modern era of readily available food. The brain can change on a physical level. When we routinely engage in dangerous behavior it is usually because parts of the brain have changed in an unhelpful way. An example of brain changes can be found in systems around a hormone called Leptin. Leptin is secreted by fat cells and helps regulate our appetite. When fat stores run low, the brain detects low levels of leptin and kicks on your appetite – you get hungry. When you are full and fats are plentiful, there are abundant leptin molecules; your brain interprets this as full. When there is a change in this system – if the brain becomes resistant to leptin, for instance – trouble emerges. You might experience the feeling of hunger far after your body has eaten enough because your brain is misinterpreting the signals. The reward system can change dramatically in response to energy-dense foods. Rats exposed to tasty, fatty foods like cheesecake and bacon have reward system reductions similar to those seen with cocaine and heroin. Obesity can spiral out of control, making it harder to reverse over time. Those four methods of creating damage: inflammation, stress, fat, and weight are all risk factors for obesity. Inflammation, for instance, can increase metabolic syndrome, a big driver of obesity. Obesity causes inflammation and might make metabolic syndrome worse. They can also disrupt the brain pathways that affect reward, inhibition, appetite, etc. Stress and changes to the reward pathway can lead to mental health trouble and worsen everything. So what can be done? The best place to start is by targeting causes. It is necessary to keep a healthy environment where you are encouraged to exercise and limit calories. Other changes may need more assistance. Medications may be available or in trials to correct changes in gene expression, inflammatory responses, and specific hormones that affect the brain. Equally important is support from friends, family, and medical professionals. The struggle against obesity can quickly spiral out of control. Don’t be afraid to look for help with this condition. Written By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Chooi, Y. C., Ding, C., & Magkos, F. (2019). The epidemiology of obesity. Metabolism, 92, 6-10. https://doi.org/10.1016/j.metabol.2018.09.005 Kenny, P. J. (2011). Reward mechanisms in obesity: new insights and future directions. Neuron, 69(4), 664-679. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3057652/ Obradovic, M., Sudar-Milovanovic, E., Soskic, S., Essack, M., Arya, S., Stewart, A. J., … & Isenovic, E. R. (2021). Leptin and obesity: role and clinical implication. Frontiers in Endocrinology, 12, 585887. https://www.frontiersin.org/articles/10.3389/fendo.2021.585887/full St‐Onge, M. P. (2010). Are normal‐weight Americans over‐fat?. Obesity, 18(11), 2067-2068. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3837418/ Upadhyay, J., Farr, O., Perakakis, N., Ghaly, W., & Mantzoros, C. (2018). Obesity as a disease. Medical Clinics, 102(1), 13-33 .http://www.medicinainterna.net.pe/sites/default/files/Obesidad_como_enfermedad.pdf
Listen to the article here:
Diabetic Neuropathy is a nerve damage complication of Type 1 and Type 2 Diabetes. It is a result of high blood sugar (glucose) which harms nerves typically in feet and legs. Diabetic Neuropathy affects everyone differently, symptoms can range from mild to impairing as it can lead to problems in the digestive system, heart, urinary tract, and blood vessels. Diabetic Neuropathy is a serious health condition that affects about 50% of people who have diabetes. There are four main types of diabetic neuropathy which have a variety of symptoms depending on the type and how a persons’ nerves are affected. Due to slow development of symptoms, a person is typically unaware that they have diabetic neuropathy until the nerve has suffered significant damage. The four types of diabetic neuropathy: This is the most common type and it first affects the legs and feet. It can progress to affect the hands and arms. Symptoms of peripheral neuropathy normally increase at night and include: This type can affect nerves in the internal organs such as the heart, digestive system, sexual organs, sweat glands, and urinary tract. Signs and symptoms include: This is the most uncommon type and is seen in about 1% of people with type 2 diabetes. It results in problems with the nerves in legs, buttocks, thighs, or hips. Symptoms typically are on one side of the body but can spread to the other side. Symptoms include: This type only affects one nerve at a time typically in the face, torso, arm, or leg. Symptoms can differ depending on the nerve being affected however they typically include: When diabetic neuropathy is diagnosed in early stages there is a higher chance that the medicine will be more effective. In order to diagnose diabetic neuropathy doctors often run tests and examinations such as: In addition to these tests and examinations, a doctor often tests blood glucose, blood pressure, and cholesterol in order to narrow down the root of the problem. Treatment for diabetic neuropathy can sometimes be as simple as changes in lifestyle, however more serious stages of neuropathy require medications in order to manage symptoms and pain. Written by: Sofia H. Davila, Clinical Researcher.
Sources: Mayo Foundation for Medical Education and Research. (2022, April 29). Diabetic neuropathy. Mayo Clinic. Retrieved February 23, 2023, from https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/symptoms-causes/syc-20371580#:~:text=Diabetic%20neuropathy%20is%20a%20type,in%20the%20legs%20and%20feet. “Diabetic Neuropathy.” Diabetic Neuropathy | Johns Hopkins Medicine, 18 Aug. 2020, https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/diabetic-neuropathy-nerve-problems.
Listen to the article here:
Peripheral Neuropathy
Autonomic Neuropathy
Proximal Neuropathy (diabetic polyradiculopathy)
Mononeuropathy (focal neuropathy)
Fats are tasty in food, but not particularly good in the bloodstream. They can also be toxic to the liver and cells in general. We have special cells called adipose cells that store fat in our body. These cells have defenses against dangerous fat components called free fatty acids. Free fatty acids are the high-energy parts of fats, the part that gives you energy. Fatty acids are a great way to store energy and can be turned into power for your body, but the high energy content can also be dangerous in the wrong places. The liver transforms free fatty acids into usable energy. From here, the energy is delivered to cells all over the body. The liver is part of the system that makes sure the body’s energy demands match the available energy. Unfortunately, when too many free fatty acids are delivered to the liver, they can start to build up in the liver tissue and cause damage. Fatty liver is one of the most common ailments in Western countries. One in every three to four people in the US havw a fatty liver. Excessive alcohol consumption can cause a fatty liver, but most sufferers develop non-alcoholic fatty liver disease (NAFLD). Either way, people have steatosis. Steato- means fat, and -osis indicates a condition, especially an abnormal one. Steatosis of 5-10% is problematic and is the earliest indication that the liver is starting to suffer damage. Many people with fatty liver and no other abnormalities can make a full recovery, usually by stopping whatever is causing the steatosis. We know that alcohol can directly damage the liver, but how does NAFLD start? The causes are complicated, but some similarities exist. Excess fat released from fat cells, excess fat created by the liver, and excess fats from the diet all find their way into the liver. These are normally not an issue, but all are affected when the body isn’t regulating insulin properly. Insulin lets body parts know when you have food or are starving. When insulin isn’t processed correctly the body thinks it’s starving and tries to compensate – even when there is plenty of food present. In the middle of this the liver suffers. After a prolonged period of fat accumulation, a patient with NAFLD may develop non-alcoholic steatohepatitis, or NASH. Steato- for fat, hepat- indicating the liver, and -itis which means inflammation. This second leg on the terrible journey develops when fat causes inflammation in the liver. The gut changes and gives the wrong signals to the liver. Cells develop insulin resistance and can’t convert sugars into energy or fats correctly. Free fatty acids cause cell problems and elicit an immune response. Stresses on the liver cause a feedback loop, where inflammation disrupts cell function. The body tries to fix the liver but can’t overcome the massive amount of dangerous fats. Cells in the liver die, and the living cells can be damaged trying to compensate. With NASH, the inflammation is long-lasting, also called chronic. The liver can regenerate from NAFLD and NASH. It can’t sustain forever, however. When the liver is permanently damaged, the tissue can scar and die. This is a permanent reduction in liver function. We call this scarring Cirrhosis. Cirros- is the Greek word for yellow-brown (the color of a dying liver), and -osis refers to a condition, especially an abnormal one. Cirrhosis has multiple stages and can be asymptomatic but cannot be recovered from without intervention. The current treatment for cirrhosis is a liver transplant. Though we’ve been talking about the dangers of fats in the bloodstream and liver, it should be noted that the body makes a lot of these fats out of carbohydrates – sugars. A healthy diet without too many sugars and with lots of exercise are the best preventative measures for these conditions. Conditions related to insulin resistance, such as type 2 diabetes and metabolic syndrome can both cause and be caused by these conditions. Also, even though we have presented these as a pathway, note that you can progress from NASH to NAFLD or become symptom-free; it’s not a one-way journey! If you have any of these conditions, talk to your primary care physician to look for solutions. Also, keep an eye out for clinical research trials that may alleviate symptoms or the underlying fat buildup.
Sources: Pierantonelli, I., & Svegliati-Baroni, G. (2019). Nonalcoholic fatty liver disease: basic pathogenetic mechanisms in the progression from NAFLD to NASH. Transplantation, 103(1), e1-e13. . https://doi.org/10.1097/TP.0000000000002480 Sanyal, A. J. (2019). Past, present and future perspectives in nonalcoholic fatty liver disease. Nature reviews Gastroenterology & hepatology, 16(6), 377-386.
Listen to the article here:

The liver is an amazing and necessary organ. It can regenerate from a minor injury, break down dangerous chemicals and drugs, and help maintain the proper balance of nutrients, fats, and sugars in the body. It has hundreds of other important roles as well. With all this responsibility, we are in trouble when the liver stops working. One way the liver stops working is through non-alcoholic steatohepatitis (NASH). Steato- means fat, hepato- indicates the liver, and -itis means inflammation. Steatohepatitis is inflammation of the liver caused by fat accumulation. This is a progressive form of non-alcoholic fatty liver disease – the most common liver disorder in western countries. Progressive means that this disease gets more severe over time. NASH is a large problem in America, affecting 3-12% of adults. Furthermore, NASH can lead to cirrhosis, where the liver is permanently damaged, and lead to possible liver transplantation. Over a million adults in America have NASH-related cirrhosis. How do we get NASH? As the name indicates, this is not caused by alcohol. There are many pathways to developing NASH, but the underlying cause may be excess carbs and fatty acids. This can be due to diet or behavior, underlying genetics, or associated syndromes. Some of the syndromes associated with NASH are: The underlying mechanism of NASH can be very complex. A leading precursor to NASH is insulin resistance, where cells fail to respond to insulin. Conditions that cause or are caused by insulin resistance, such as type II diabetes and metabolic syndrome, may increase your chances of developing NASH. They also may develop or worsen as NASH symptoms get worse. Insulin resistance causes different types of fats to accumulate in the liver. This makes it very difficult for the liver to process the fats and they ultimately build up in liver cells. These fats, especially ones called nonesterified fatty acids (NFEAs), are very dangerous. They cause damage to liver cells and can also activate cytokines that start the inflammation process. Eventually, we get NASH, an inflammation cascade in the liver caused by fats. Cytokines start inflammation in the liver. Cell death attracts the immune system, which enters and causes inflammation while trying to help. Liver cells die and are less able to process fats, which leads to a compounding effect. Eventually, we may transition to cirrhosis, where permanent liver scarring and damage occur. There are few treatments on the market for NASH. As usual, the primary therapy for NASH is a good diet and regular exercise. Medicinal remedies are all in the experimental phases. Potential targets include increasing insulin sensitivity, decreasing fat creation, decreasing circulating fats, breaking fats down, and anti-inflammation treatments. One way to decrease circulating fats is by expelling them through the digestive system. In the liver, moving fats to the gut is regulated by thyroid hormones. Thyroid hormones activate receptors, which exist all over the body and cause many different effects. Thyroid hormone receptor Beta (THR-β) exists almost exclusively in the liver. Scientists are working to create medicines that activate THR-β and help clear fats from the liver in NASH patients. If you are interested in participating in a research study, contact your local ENCORE Research Group site today!
Sources: Noureddin, M., & Sanyal, A. J. (2018). Pathogenesis of NASH: the impact of multiple pathways. Current Hepatology Reports, 17, 350-360. Parthasarathy, G., Revelo, X., & Malhi, H. (2020). Pathogenesis of nonalcoholic steatohepatitis: an overview. Hepatology communications, 4(4), 478-492. https://doi.org/10.1002/hep4.1479 Pierantonelli, I., & Svegliati-Baroni, G. (2019). Nonalcoholic fatty liver disease: basic pathogenetic mechanisms in the progression from NAFLD to NASH. Transplantation, 103(1), e1-e13. . https://doi.org/10.1097/TP.0000000000002480 Pramfalk, C., Pedrelli, M., & Parini, P. (2011). Role of thyroid receptor β in lipid metabolism. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease, 1812(8), 929-937. https://doi.org/10.1016/j.bbadis.2010.12.019
Listen to the article here:
Eosinophilic asthma is a type of asthma that is characterized by high levels of eosinophils in the airways. Eosinophils are a type of white blood cell that are involved in the body’s immune response to allergens and other triggers. When eosinophils are activated, they release inflammatory chemicals that can cause damage to the airways, leading to asthma symptoms. Symptoms of eosinophilic asthma include wheezing, coughing, shortness of breath, and chest tightness. These symptoms may be more severe than those of other types of asthma and may not respond as well to traditional asthma treatments like inhaled corticosteroids. Diagnosis of eosinophilic asthma involves a blood test to measure eosinophil levels and a sputum test to look for eosinophils in mucus from the lungs. Treatment may involve targeted biologic medications that specifically target eosinophils, such as mepolizumab, reslizumab, and benralizumab. These medications work by reducing the number of eosinophils in the airways, which can help to reduce asthma symptoms and improve lung function. If you or someone you know has severe asthma, clinical trials may be an option for you. Clinical trials are an important way to test new medications and treatments for asthma and other conditions. They allow researchers to gather important data on the safety and effectiveness of new treatments, and they provide patients with access to cutting-edge therapies that may not be available through traditional channels. By participating in a clinical trial, you can play an important role in advancing medical research and helping to improve the lives of people with eosinophilic asthma and other conditions. Clinical trials for this condition are currently available at ENCORE Research Group’s Jacksonville Center for Clinical Research, University Blvd. location. To learn more, you can contact us by phone, or sign up on our website. Our knowledgeable staff can guide you through the process and help you determine if a clinical trial is a good option for you.
Celiac disease is a genetic autoimmune disease that affects the digestive system. It is triggered when a person consumes gluten, which is a protein found in rye, wheat, and barley. When a person with celiac disease eats gluten, their immune system reacts to the protein by attacking the small intestine. The role of the small intestine is to digest food and allow the body to use the nutrients. When the body attacks the small intestine, it damages the lining of the small intestine, resulting in symptoms that include bloating, abdominal pain, and weight loss. Eventually, after the small intestine has suffered damage, it can result in the body’s inability to absorb nutrients, therefore leading to a deficiency of nutrients and health problems. It is often difficult to tell if children have celiac disease, as the symptoms in children and adults differ. Symptoms in adults include: Adults can also experience a variety of symptoms unrelated to the digestive system, such as: Digestive problems are commonly seen in children with celiac disease, rather than in adults with celiac. Symptoms in children include: Symptoms are often not enough to tell if someone has celiac disease. People are more susceptible to celiac disease if they have some of the risk factors listed below: Diagnosis of celiac disease is through blood tests that check for certain antibodies and biomarkers. Often following these blood tests is an endoscopy/biopsy of the small intestine to evaluate the damage caused by the body’s response to the gluten protein. Although there is no cure for celiac disease, a change in diet helps to regulate the symptoms of celiac disease. A gluten-free diet often consists of gluten-free foods and vitamin and mineral supplements to regulate the body’s nutrients. Following a gluten-free diet allows the small intestine to heal. Doctors and dietitians can help guide people on their diet and inform them of gluten-free alternatives. This diet is normally life-long in order to prevent symptoms or a flare-up of the small intestine again. Doctors sometimes prescribe steroids as well to help regulate the inflammation of the small intestine. It is often difficult for people with celiac disease to eat out at restaurants or buy pre-made food from stores as it is tricky to be one hundred percent certain that a food is truly gluten-free. Stickers on foods say “may contain gluten” as a way to protect the manufacturing companies from lawsuits. However, most of the time the food does not contain gluten itself but has a small chance that it could have been cross-contaminated during the production process. This limits food that people with celiac disease feel safe consuming and buying. The FDA has standards that must be met in order for a food to be labeled as “gluten-free”. The final product must contain, at most, 20 mg/kg (20 parts per million) gluten or less. However, this rule does not apply to alcohol which can contain gluten. This amount of gluten (20 ppm) will not result in any side effects in a person with celiac disease, since it is too small of an amount. Another way people can be sure that they are consuming gluten-free foods is to call a restaurant ahead of time and ask if they have a gluten-free menu or serve alternatives for people with gluten intolerance. Written by: Sofia H. Davila, Clinical Researcher
Sources: Mayo Foundation for Medical Education and Research. (2021, August 10). Celiac disease. Mayo Clinic. Retrieved February 17, 2023, from https://www.mayoclinic.org/diseases-conditions/celiac-disease/diagnosis-treatment/drc-20352225 NCI Dictionary of Cancer terms. National Cancer Institute. (n.d.). Retrieved February 17, 2023, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/small-intestine U.S. Department of Health and Human Services. (n.d.). Eating, diet, & Nutrition for Celiac Disease. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved February 20, 2023, from https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-disease/eating-diet-nutrition
Atrial fibrillation (AFib) is a heart rhythm disorder characterized by irregular heartbeats in the heart’s upper chambers, called the atria. In AFib, the electrical signals that regulate the heartbeat become abnormal, causing the heart to beat too fast or slow instead of contracting normally. Atrial fibrillation can have detrimental effects such as stroke, heart failure, and blood clots.
Image Credit: cdc.gov
As a result of the irregular heart beatings, a variety of symptoms can be present such as: In some cases, people with AFib may not experience any symptoms, making it difficult for some people to tell whether or not they may have AFib. Some broader symptoms can include: Sometimes even these broader symptoms can not help people determine if they have AFib. The only way for people to know if they have AFib without experiencing any symptoms is to get tested and diagnosed by a doctor. It is strongly recommended that if a person has any of the risk factors below, they get checked, just to be safe, by a doctor. AFib is often seen in older adults, with risk factors that include: Some treatments are more effective when delivered in the early stages of AFib, which means that a person should not postpone getting checked by a doctor for AFib. However, symptoms and causes of AFib can often differ between men and women. In women, AFib usually is caused by problems with the heart valves. Compared to men, where AFib usually stems from coronary artery disease (CAD). As a result, women with AFib have a greater chance of having a stroke than men with AFib. Women with AFib also are more likely to have heart attacks and congestive heart failure than men with AFib. As a result, treatments for men and women often differ slightly. Treatment for AFib is typically a medication to control heart rhythm and prevent blood clots. However, in some cases, procedures such as electrical cardioversion, ablation, or implantation of a pacemaker or defibrillator may be necessary. Men with AFib are often placed on non-drug therapies such as pacemakers and catheter ablation. Women with AFib are more likely to have a cardioversion and be prescribed antiarrhythmic medications such as dofetilide. However, typical treatments for both men and women include blood-thinning medications, surgery, and lifestyle changes to manage AFib risk factors. Written by: Sofia H. Davila, Clinical Researcher
Sources: Miller, K. (2022, December 27). Atrial fibrillation: The difference between men and women. Healthgrades. Retrieved February 17, 2023, from https://www.healthgrades.com/right-care/atrial-fibrillation/atrial-fibrillation-the-difference-between-men-and-women Centers for Disease Control and Prevention. (2022, October 14). Atrial fibrillation. Centers for Disease Control and Prevention. Retrieved February 17, 2023, from https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
Our patients are enthusiastic and excited to take part in clinical research. There are a variety of reasons a patient would want to participate in a clinical trial: they join to benefit future generations, to advance medicine, to get medical help and compensation, and to increase diversity. The most frequent reason for joining a clinical study, however, is to help others. Clinical research is the best framework for ensuring the safety and effectiveness of new medications, devices, and procedures. This includes everyone from participants of phase 1 clinical trials to final consumers after FDA approval. But what does the process actually look like for patients? People hear about us from a wide variety of sources: advertisements, community outreach programs, the internet, and personal referrals from family and friends. Thousands of our patients are referred to us by friends, family, and their own physicians. People’s great experiences with us make them very likely to recommend us to others. Most of our patients are repeat offenders. In fact, over 99% of our patients return for another study. When you are interested in an ENCORE Research Group study, our experienced and compassionate recruiters will talk with you. These experts care about your time more than anything else. They will run through a quick checklist to see if you prequalify for a study. If you prequalify, they will schedule an evaluation. They will find a time that works best for you to come in or receive a call with a research coordinator. Here the compassionate and attentive nature of ENCORE Research Group excels. You will receive forms to fill out your medical history, medications, and contact information. During your appointment, our attentive and detail-oriented staff will review your documents. They will confirm and expand on any medical conditions that may affect your participation. This step makes sure you are always safe and gives our staff personal knowledge to help you during your study. Patient safety is always our number one priority. After an evaluation, if you choose to participate, you will start the informed consent process. Here you will review the clinical trial process and the plan for your specific study. Research coordinators will explain and review a highly detailed and regulated consent form. This document informs you about the study, potential side effects, the goals and endpoints of the study, your rights, and what to expect. This is a vital step. We will also remind you that you can end participation in the study at any time for any reason. Your voluntary participation does not oblige you to continue at any point. What happens from here depends on your specific study, but some things will remain constant. Our doctors and medical staff will talk with you. Other patients describe them as professional, friendly, and compassionate. You may receive medication, a placebo, device, or undergo a procedure. This will have been explained in detail during the informed consent process. One big difference between ENCORE Research Group and a normal doctor’s office is the comprehensiveness and amount of follow-up. Our doctors give you their full, undivided attention when you are in their office. They have plenty of time and want to know the intricacies of your medical history. For most studies, our staff will periodically check up on you after you leave. We are also keenly interested in knowing if you experience any new or changing symptoms. This will continue until your study has concluded. Then, if you wish, we will contact you if you qualify for more studies. This process results in a streamlined, professional, and personal system. You get to help medicine and society, but also experience top-quality, attentive care for a variety of conditions. Join the clinical trial process with ENCORE Research Group and see why nearly all of our patients come back! By Benton Lowey-Ball, BS Behavioral Neuroscience
There are many ways to think of the human body. One of my favorites is that the body is like a donut. The inside of the donut is our entire body and everything that makes us what we are. The outside is our skin. The hole in the middle is made of our mouth, throat (esophagus), stomach, and intestines. The body treats the entirety of the digestive tract as the outside world. The intestines act like the skin; keeping most things out of the body and only letting specific molecules through. This has some important implications. The whole outside of the donut – including the throat and intestines – is covered in epithelial cells. These are tight cells that interact with the outside world. When these cells determine that they are touching something dangerous they signal to get rid of it immediately. This might feel like burning or itching on the skin, and may be something like diarrhea or vomiting in the digestive tract. These may feel crummy to us, but they are very useful in keeping us safe. The immune system is in charge of identifying and reacting to chemical and biological dangers. These can be harmful bacteria, worms, and things like splinters or some drugs. The immune system kicks into action, trying to kill or remove the dangerous particles without damaging body cells. This is a tricky dance. Antibodies will identify the dangerous particles or creatures and special B or T cells will widely sprinkle alarm particles, calling for reinforcements. What the body does next is determined by where the danger is found. In the gut – which the body treats as the dangerous outside world – the defenses are strong. One of the biggest guns we have is a cell called an eosinophil. These are very dangerous cells. They contain highly toxic particles and proteins that aggressively dunk in on invaders. They also signal to the intestines to contract and eject the contents. They only exist in specific parts of the body and are normally difficult to activate. Unfortunately, sometimes our body identifies otherwise safe items as dangerous. This is called allergies, and can be very annoying. Many of us suffer from seasonal allergies, but that doesn’t mean we should glaze over the dangers of allergic reactions. One difficult condition is eosinophilic esophagitis. Eosinophilic means it is caused by the dangerous eosinophil cells. Esophagitis refers to the fact that this happens in the esophagus, the throat. Eosinophils do not normally reside in the throat at all. The throat’s main job is to move food into the stomach, so it doesn’t need to detect danger. When eosinophils mistakenly reside in the throat, however, they can misidentify otherwise safe foods before the stomach gets a chance to digest them. This can result in the eosinophils damaging the throat. Eosinophilic esophagitis affects four in every thousand people, and can affect people of all ages. Most sufferers were diagnosed as children. In fact, it is one of the most common diagnoses for children who have trouble eating. It is chronic, or long lasting, and symptoms are debilitating. Sufferers experience inflammation of the throat, poor food intake, vomiting, and a poor appetite. Unfortunately there are few treatments available to fix this condition. The most effective has been reducing the diet of patients. This may consist of starting with a very strict diet and reincorporating food slowly to discover triggers. Scientists are actively looking at the underlying causes of why eosinophils are in the throat to begin with. Possible future treatments would likely stop eosinophils in the throat at a cellular or genetic level. The body may be a donut, but that doesn’t mean everything is tasty and fresh. If you are suffering from eosinophilic esophagitis or other conditions, call ENCORE Research Group and ask about studies you may qualify for. By Benton Lowey-Ball, BS Behavioral Neuroscience
Furuta, G. T., & Katzka, D. A. (2015). Eosinophilic esophagitis. New England Journal of Medicine, 373(17), 1640-1648. https://doi.org/10.1056%2FNEJMra1502863 Janeway Jr, C. A., Travers, P., Walport, M., & Shlomchik, M. J. (2001). Effector mechanisms in allergic reactions. In Immunobiology: The Immune System in Health and Disease. 5th edition. Garland Science. https://www.ncbi.nlm.nih.gov/books/NBK27112/ Rothenberg, M. E. (2004). Eosinophilic gastrointestinal disorders (EGID). Journal of Allergy and Clinical Immunology, 113(1), 11-28. https://doi.org/10.1016/j.jaci.2003.10.047 Zuo, L., & Rothenberg, M. E. (2007). Gastrointestinal eosinophilia. Immunology and allergy clinics of North America, 27(3), 443-455.https://doi.org/10.1016%2Fj.iac.2007.06.002
Listen to the article here:
In the 1990’s the philosopher Haddaway posed a critical question: What is love? This Valentine’s Day, many of us will experience love and companionship. We like to think of love as an amorphous, idealistic quality, but there are serious biological underpinnings. What is the biology behind love, and is the heart really where love lies (spoiler: maybe?) We know that the brain directs our physical actions, but for the brain to come up with an idea, it needs input from the outside world. Interestingly, the brain can’t sense anything directly. If someone were to open up your skull and have a poke around, you would undoubtedly have a weird bit of sensation, but you wouldn’t experience the feeling of touch on the brain. We need special sensors (usually located on the skin) to feel things like touch. Indeed, our brain relies on signals coming in from all over the body to tell us about the outside world. Interestingly, we also rely on signals to tell us about the inside world – what we are experiencing. The brain interprets signals from the body, and we can experience that interpretation as an emotion. As an example: your heart beats automatically all day, every day, at a hopefully regular interval of around once a second. When you see a scary event, such as a wild lion charging you, your brain and body respond in sync. The heart rhythm changes, beating much faster to provide your muscles, sensory organs, brain, etc., extra oxygen in order to move fast. But this effect isn’t strictly rational. After we escape from the lion, we still feel “amped up.” This effect can last for thirty minutes or so, and the reason for the long-lasting effect is complicated. Our autonomic nervous system – the one in charge of things we don’t consciously control – has kicked into action. This pathway acts like cupid, shooting cortisol through our body and activating special nervous system pathways that take a while to cool down. But our brain also looks at the state of our body to interpret our emotional state. If our palms are sweaty, we’re breathing heavily, and our heart is racing, the brain interprets that as being amped up and decides we’re still pretty excited or scared. The brain is in charge of deciphering which emotion we’re feeling, but the body lets us know how strongly we’re feeling that emotion. This is why we sometimes still feel the need to continue an argument after the other party has conceded. It’s why telling someone to “calm down” doesn’t work – but taking some deep breaths does. Meditation, stretching, exercise, and sleep all affect our emotional state because the brain looks at the condition of the body and tries to figure out how it’s feeling. In addition, a healthy heart that can respond well to changes may increase a person’s emotional regulation. Does it do this with love as well? According to neuroendocrinology researcher Robert Sapolsky, it does! The science may not be entirely clear, but the easiest way to be certain of this is by looking at the irrationality of love. Love doesn’t make sense, and it’s so strong that we base enormous portions of our life just on this single emotion. Love is the basis of countless pieces of art, works of literature, grand buildings, and justifications for war. When we experience love – that fluttering of the heart, the excitement and elation, the involuntary smile on our face, and the giddiness so high that our mouths stop working and we say embarrassing, cheesy things – it’s the body to blame. Our heart races when we’re in love and the brain sees this as a huge exciting event – because it is. Just seeing the person we love can change our heart rate. Physical touch from a loving partner can help lower our heart rate in response to stressful situations. And the long-term effects of companionship sometimes include a partial synchronization of our heart rhythms. We can thank our hearts for at least some of what we call love. This Valentine’s day, get your heart racing with a partner or loved one, and keep that heart beating strong! By Benton Lowey-Ball, BS Behavioral Neuroscience
Ditzen, B., Neumann, I. D., Bodenmann, G., von Dawans, B., Turner, R. A., Ehlert, U., & Heinrichs, M. (2007). Effects of different kinds of couple interaction on cortisol and heart rate responses to stress in women. Psychoneuroendocrinology, 32(5), 565-574. https://doi.org/10.1016/j.psyneuen.2007.03.011 Kandel, E. R., Schwartz, J. H., Jessell, T. M., Siegelbaum, S., Hudspeth, A. J., & Mack, S. (Eds.). (2000). Principles of neural science (Vol. 4, p. 980). New York: McGraw-hill. Mather, M., & Thayer, J. F. (2018). How heart rate variability affects emotion regulation brain networks. Current opinion in behavioral sciences, 19, 98-104. Sapolsky, RM. (various works)
Listen to the article here:
Cardiovascular disease has remained the number one cause of death worldwide. Multiple clinical trials have revealed that a common and modifiable risk factor for cardiovascular disease is high cholesterol, and if a person lowers their cholesterol, they can lower their risk for heart-related diseases. Most of us have heard of cholesterol, but what is it? Why is having too much cholesterol a bad thing? How do we get cholesterol in our bodies? What can you do to lower your cholesterol to healthy levels? Cholesterols are a broad and useful type of fat found in the body. The body needs them to create hormones, essential vitamins (like vitamin D), and other molecules. They float on the surface of our cells, helping to maintain the structure and function of cell barriers. Cholesterols regulate cell activity and act outside of cells. They insulate the neurons in our brain, allowing us to think. In fact, cholesterol is so important to daily function, that every cell in the body can make cholesterol from basic materials, except your eyelashes! There are times when cholesterol is downright bad. LDL cholesterol and Lipoprotein a [Lp(a)] have some particularly sticky portions that can get stuck to the inside of our bloodstream. We call one of these portions ApoB. Sticky cholesterol obstructs blood flow in the form of plaques. Without help, this leads to atherosclerosis, scarring, and hardening of the arteries. Atherosclerosis further cascades into cardiovascular disease, clots, heart attacks, and stroke. This is very bad. Unfortunately, it is also very common; atherosclerosis in the neck is found in ¼ of people worldwide. Lowering excess cholesterol is a global health concern. Our liver creates enough cholesterol to supply our bodies. We are also able to absorb cholesterol from our diets and make some in other cells. The most effective methods of reducing cholesterol are lifestyle and diet changes. However, for some people, diet and exercise don’t seem to budge their cholesterol numbers at all. For others, the ability to exercise and dietary restrictions may be limited. This is where medications can step in. To understand how a medication may reduce LDL and/or Lp(a), we need to learn a bit about how the body makes things from DNA. Genes are bits of DNA that contain the blueprint for a protein. Genes provide the blueprint to messenger RNA (mRNA). The mRNA translates genetic code into proteins. The cells then fold proteins into complicated, machine-like shapes. Proteins interact with molecules and other proteins to create all sorts of things for the body – including cholesterol. Clinical research has been expanding which of these steps we can target for medications. Statins are the first line treatment for reducing cholesterol. They target hydroxymethylglutaryl coenzyme A (HMG-CoA). HMG-CoA is a protein used to construct cholesterol molecules. Reducing HMG-CoA slows the body’s ability to create cholesterol, lowering cholesterol levels. Statins block the production of the “bad” LDL-C cholesterol and lower levels by as much as 60%. The benefits for statins to reduce cardiovascular events have been proven in multiple clinical trials over a diverse patient population. Other oral medications, including ezetimibe and bempedoic acid, can be taken with statins. Ezetimibe can lower LDL-C levels by approximately 20% by inhibiting cholesterol absorption in the intestines, making it a useful add-on medication when statins alone are insufficient. Bempedoic acid can lower LDL-C by 15-25% by decreasing cholesterol synthesis in the liver. Because bempedoic acid is converted to an enzyme found only in the liver and not the muscles (like statins), it is often an alternative for patients who have statin-associated muscle myalgias. Monoclonal antibodies (MoAbs) are a newer class of medication. MoAbs like alirocumab and evolocumab act like signaling molecules. These two stay outside of cells and tell the liver to produce less of the protein PCSK9. Controlling PCSK9 is a newer method of changing a person’s cholesterol profile. PCSK9 controls how much extra LDL cholesterol is absorbed and recycled by cells. MoAb medications affect this by targeting signaling receptors on the outside of the liver. Even newer medications target the process by which genes get turned on inside the cells. They are called gene silencing therapies because they aim to “silence” the gene’s effects. Antisense oligonucleotides (ASOs) and small interfering RNA (siRNA) stop the liver from producing functional LDL or Lp(a) mRNA molecules. These act at different, very early stages of the cholesterol process. In addition, specialized packaging on the medications deliver them to the liver and not other cells. This can make for very targeted medications that (hopefully) have fewer side effects. Inclisiran is the first FDA-approved siRNA therapy to lower LDL cholesterol. It is a subcutaneous injection taken twice a year. Imagine going to your physician’s office just twice a year to get your “cholesterol vaccine”! Even more amazing, gene editing tools such as CRISPR could reduce overexpression of PCSK9 or other genes on a long-term basis. These are still in early phase trials, but the future is looking bright. Lipoprotein a,or “L-P-little-a”, or Lp(a), is a new target for decreasing the risk of cardiovascular disease. Lp(a) is genetically inherited and increases the risk for both heart disease and stroke because it can promote plaque buildup, blood clots, and inflammation. New gene silencing therapies are in clinical trials right now using both ASO and siRNA technology. Diet, lifestyle changes, and statins remain the front-line defense against high cholesterol. New medicines may work with or replace these classical defenses. As technologies move through the clinical research apparatus, we may be able to tailor custom combinations of medications for individual patients. ENCORE Research Group has been involved in every step along this path, helping to study medications in every category. Join our team and help pave the way for new medications to help combat high cholesterol!
Sources: Craig, M., Yarrarapu, S. N. S., & Dimri, M. (2018). Biochemistry, cholesterol. https://www.ncbi.nlm.nih.gov/books/NBK513326/ Fernandez-Prado, R., Perez-Gomez, M. V., & Ortiz, A. (2020). Pelacarsen for lowering lipoprotein (a): implications for patients with chronic kidney disease. Clinical Kidney Journal, 13(5), 753-757. https://doi.org/10.1093%2Fckj%2Fsfaa001 Prati, P., Vanuzzo, D., Casaroli, M., Di Chiara, A., De Biasi, F., Feruglio, G. A., & Touboul, P. J. (1992). Prevalence and determinants of carotid atherosclerosis in a general population. Stroke, 23(12), 1705-1711. https://doi.org/10.1161/01.str.23.12.1705 Tokgözoğlu, L., & Libby, P. (2022). The dawn of a new era of targeted lipid-lowering therapies. European Heart Journal. https://doi.org/10.1093/eurheartj/ehab841
Listen to the article here:
After we eat a meal, all that energy has to go somewhere. Body cells can use freely floating glucose sugar in the bloodstream, but fats are a bit trickier. Just like oil and water don’t mix, fats have trouble moving through the blood in our veins and arteries. They must be packaged inside special containers called lipoproteins in order to travel where they need to go. For fats that we eat, the fats (called triglycerides) are packaged into ultra-low-density chylomicrons by the digestive system. Our liver also processes and repackages fats. The liver makes very low-density lipoproteins (VLDL) out of triglycerides and ejects them into the bloodstream. VLDLs can then use the bloodstream to travel to fat cells or be converted into other forms of energy storage. The number of triglycerides in the bloodstream at once needs to be well regulated. For adults, fasting triglyceride levels should be under 150 mg/dL. This number decreases to below 90 mg/dL for people under 19 years of age. Unfortunately, one in ten adults have high levels, called hypertriglyceridemia. When there are too many triglycerides, they can stick to the inside of the bloodstream. They can create and contribute to hard plaques, a condition called atherosclerosis. These put stress on the cardiovascular system and can lead to atherosclerotic cardiovascular disease (ASCVD). Very high triglycerides above 500 mg/dL is called severe hypertriglyceridemia. This can lead to even more problems, including chylomicronemia, pancreatitis, and death. What contributes to high triglyceride levels? A lot, actually! A diet that is high in sugars and fats, excessive alcohol consumption, being overweight, and a sedentary lifestyle can contribute. Some conditions, such as diabetes, kidney and liver disease, and thyroid problems increase your chances. Anything that affects liver function is likely to change how the body processes fats and may increase triglycerides. This means some life-saving medications, including several cancer, hypertension, and HIV treatments may increase triglycerides. Some people have high or very high triglycerides – usually in the form of chylomicrons – even without these risk factors. This may be because of our genes. One of the major genetic culprits for increased triglycerides is a gene called APOC-3. This gene codes for a protein of the same name: Apolipoprotein C-III (apoC-III). You can tell these apart because the gene is uppercase, italicized, and uses a (3), while the protein is mostly lowercase and uses roman numerals (III). The protein apoC-III can lead to some detrimental effects. Normal triglycerides bind to a different protein, apoC-II. This helps them get broken down in the bloodstream. ApoC-III binds to triglycerides in the same place as apoC-II but makes them less able to be processed. These triglycerides build up in the bloodstream and can cause atherosclerosis and ASCVD. Scientists also have evidence that apoC-III makes triglyceride-rich molecules stickier to the arteries. ApoC-III binds to chylomicrons very well, making these fats especially resistant to breaking down. So why do we have apoC-III anyway? It turns out, not all of us do! Different people have different variations of the APOC-3 gene. Some people have a gene that produces excessive apoC-III protein, and a few have genes that produce none! People with defective APOC-3 genes seem to be just as healthy as everyone else. Maybe healthier, as their levels of triglycerides are very low, even after a fatty meal! Researchers consider a defective APOC-3 gene to be cardioprotective, meaning that it lowers the chances of heart disease. Are there methods for us to lower the production of apoC-III and our triglyceride-rich chylomicrons? It looks possible. The liver produces more apoC-III in response to high levels of blood sugar and most fats, so lowering these may help. It decreases production of apoC-III when it encounters high levels of insulin or polyunsaturated fats (such as Omega-3 fatty acids). This may be helpful, but is bad news for those with type 2 diabetes. In these patients the bloodstream has extra glucose and lacks insulin. Treating high triglycerides can be complicated. A diet low in alcohol, carbs, and fats but high in omega-3 fatty acids can help. Exercise and weight loss are often helpful. Doctors may also prescribe fibrates, nicotinic acid (niacin), or statins. Unfortunately, these medications may not work if you have excessive levels of apoC-III and high chylomicrons. A diet that is very low in fats – under 20 grams a day – has been the only option for some patients. New classes of medication may be helpful as well. Antisense oligonucleotides, gene therapy, and custom antibodies can be used to target the production of specific proteins. Antisense oligonucleotides, for instance, bind to APOC-3 mRNA in the cell, preventing it from creating apoC-III proteins. They do this with extreme specificity, targeting only the gene in question. They can also do this only in liver cells by being packaged in a special way. Drugs that target apoC-III production may be able to bring down otherwise stubbornly high triglycerides without too many side effects. A side effect of reading the ENCORE Research Group website is learning about these new medicines and when they may be available for you in a trial!
Sources: Alves-Bezerra, M., & Cohen, D. E. (2017). Triglyceride metabolism in the liver. Comprehensive Physiology, 8(1), 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6376873/ Goldberg, R. B., & Chait, A. (2020). A comprehensive update on the chylomicronemia syndrome. Frontiers in endocrinology, 11, 593931. https://doi.org/10.3389/fendo.2020.593931 National Institute of Health, National Heart, Lung, and Blood Institute. (April 7, 2022). High blood triglycerides. U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov/health/high-blood-triglycerides Rahmany, S., & Jialal, I. (July 18, 2022). Biochemistry, Chylomicron. https://www.ncbi.nlm.nih.gov/books/NBK545157/ Taskinen, M. R., Packard, C. J., & Borén, J. (2019). Emerging evidence that ApoC-III inhibitors provide novel options to reduce the residual CVD. Current atherosclerosis reports, 21(8), 1-10. https://doi.org/10.1007/s11883-019-0791-9
Listen to the article here:
The Role of Apolipoprotein C-III (apoC-III) in Atherosclerosis and Cardiovascular Disease
In fifth grade, I learned that mitochondria are the powerhouses of the cell. But what’s the fuel? The answer is carbohydrates. Big carbohydrates are broken down by digestion and converted into a couple of simple sugars. The most abundant of these simple sugars in our bodies is glucose. Glucose is small, simple, and packed with energy. We transport it through our bloodstream to cells in our body. Glucose levels are regulated by the liver and pancreas. Unfortunately, conditions like diabetes can result in the dysregulation of blood glucose levels. Having too much sugar in the blood is very bad over time. It can result in damage to the eyes, kidneys, nerves, and heart. On the flip side, having low blood sugar can get dangerous right away. Glucose is the fuel that powers our cells, without it the brain and other organs can’t function. We know that glucose is critical to body function. We also know that glucose levels can get out of control. What can we do to make sure glucose levels stay safe? The most important piece of the puzzle is information. Good information on what our blood glucose levels are is critical to know what to do. We get this information by testing our blood glucose levels. There are three major ways of testing blood glucose; chemical redox reactions, color change, and enzyme-based reactions. Now we know the chemical methods of measuring glucose, but how do we actually test our glucose level? Three broad testing types exist: oral, self-test, and continuous glucose monitors. These are differentiated mainly by the frequency and invasiveness of the test. As the old saying goes, knowledge is power! With the help of the latest CGM technology, we are able to see information in real-time such as how food, exercise, and stress impact glucose levels. This helps us take immediate action to manage our glucose levels. So, take action to keep your blood glucose in the healthy range with your new knowledge, a good diet, and consistent exercise. Make sure it stays there by monitoring your blood glucose levels regularly. Keep your eyes open to look for new studies looking at ways to monitor your blood glucose and keep your cells powered up!
Sources: American Diabetes Association (n.d.). Understanding A1C diagnosis. American Diabetes Association. https://diabetes.org/diabetes/a1c/diagnosis McMILLIN, J. M. (1990). Blood glucose. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Chapter 141. https://www.ncbi.nlm.nih.gov/books/NBK248/ Wang, H. C., & Lee, A. R. (2015). Recent developments in blood glucose sensors. Journal of food and drug analysis, 23(2), 191-200. https://doi.org/10.1016/j.jfda.2014.12.001
Listen to the article here:
Cardiovascular disease (CVD) is the leading cause of death in the United States. There are several risk factors for cardiovascular disease. This can include things you can’t change, such as sex, age, and genetics. They can also include things you can change. The WHO identifies four big behaviors that can change your risk of developing CVD: These behaviors generally lead to other undesirable indicators of health, including obesity, hypertension, high blood sugar, and increased cholesterol. Clearly, ceasing the behavioral risks is a high priority. Unfortunately, this is often easier said than done. One of the most difficult habits to quit is smoking. Studies show that those attempting to quit without assistance have an over 90% relapse rate. Several medications exist to help quit smoking, including Bupropion SR (aka Wellbutrin) and Varenicline (aka Chantix). There are also nicotine-based alternatives, including gum, inhalers, lozenges, nasal sprays, and patches. Nicotine rewires the brain as it’s consumed. It releases dopamine, the brain’s reward drug, and rewards us for smoking. Researchers think the frequency of smoking may be partially to blame for the intensity of the addiction. The amount of dopamine released is not particularly high compared with other drugs, but nicotine also causes changes to the striatum. The striatum is part of the reward circuit in the brain. Through a complicated mechanism, nicotine increases the amount of a protein called FosB, which changes the striatum’s sensitivity to dopamine. This is a change at the genetic level which makes the brain more susceptible to further reward signals. Nicotine seems to make normal activities more pleasurable. Unfortunately, as nicotine adjusts the brain’s mechanisms, the brain relies on it to get to a baseline of reward. Upon quitting smoking, the brain finds normal activities less enjoyable. On its own, nicotine may have negative effects, and in heavy doses it has been shown to be dangerous. The biggest dangers of smoking, however, are likely in the myriad of other chemicals in tobacco and cigarettes. Though nicotine causes changes in the brain, cigarettes cause changes to the fats in your body, further increasing CVD risk. Along with this, cigarettes cause cancer, COPD, diabetes, erectile dysfunction, and immune system changes. Clearly, quitting smoking is critical to health. With the addictive nature of nicotine and the low success rate of quitting cold turkey, assistance may be needed. The brain gets addicted to nicotine, but we can fight back using behavior. You can actually help yourself “break the cycle” of nicotine addiction by changing your daily routines. For example if the first thing you do in the morning is reach for a cigarette, change your routine to going to the bathroom and brushing your teeth first instead. Behavioral interventions can make a significant difference. Combining behavior changes and counseling with a nicotine replacement or medication can help quit rates approach 30%. Indeed, nicotine replacements are most effective when used with behavioral interventions. Changing your behavior or routine can have positive impacts on your health. So next time you want to reach for a cigarette, grab your phone instead! Give us a call and discover what clinical trials you can take part in!
Sources: Bancej, C., O’Loughlin, J., Platt, R. W., Paradis, G., & Gervais, A. (2007). Smoking cessation attempts among adolescent smokers: a systematic review of prevalence studies. Tobacco control, 16(6), e8-e8. https://doi.org/10.1136%2Ftc.2006.018853 Fiore, M. (2008). Treating tobacco use and dependence; 2008 guideline. https://stacks.cdc.gov/view/cdc/6964/cdc_6964_DS1.pdf Garbin, U., Fratta Pasini, A., Stranieri, C., Cominacini, M., Pasini, A., Manfro, S., … & Cominacini, L. (2009). Cigarette smoking blocks the protective expression of Nrf2/ARE pathway in peripheral mononuclear cells of young heavy smokers favouring inflammation. PloS one, 4(12), e8225. https://doi.org/10.1371/journal.pone.0008225 Koren, M. (Host). (2022, May 22). Nicotine replacement therapies to help stop smoking [Audio podcast episode]. In Medevidence! Truth behind the data. ENCORE Research Group. https://www.buzzsprout.com/1926091/10484183-nicotine-replacement-therapies-to-help-stop-smoking Messner, B., & Bernhard, D. (2014). Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arteriosclerosis, thrombosis, and vascular biology, 34(3), 509-515. https://doi.org/10.1161/ATVBAHA.113.300156 NIDA. (2018, September 28). Recent Research Sheds New Light on Why Nicotine is So Addictive. https://nida.nih.gov/about-nida/noras-blog/2018/09/recent-research-sheds-new-light-why-nicotine-so-addictive US Department of Health and Human Services. (2014). The health consequences of smoking—50 years of progress: a report of the Surgeon General. https://www.ncbi.nlm.nih.gov/books/NBK294320/
Listen to the article here:
We humans seem to like making a fresh start. Whether it’s the beginning of a semester, a month, or a week, we like having a “clean slate” to make changes. The most widely used of these fresh start times are at the beginning of the year, with a New Year’s Resolution. Over 40% of all Americans make New Year’s resolutions, but much like a firework, we make a bright claim with a loud noise, only for it to burn out quickly as the year goes on. How can we make good resolutions that we are likely to follow, and are there strategies we can use to help us follow through? Probably the most important piece of a New Year’s Resolution is coming up with a good resolution in the first place! Surveys show that around two-thirds of all resolutions are health-oriented, including eating healthier, exercising, getting in shape, etc. Psychological studies have shown that the wording of your resolution matters. Most resolutions can be broadly lumped into either activation or avoidance goals. Activation goals are those that encourage you to do something: exercise more, eat more greens, etc. Avoidance goals are those that encourage you to not do something: watch less TV, eat less pizza, etc. Several studies have shown that activation goals are significantly more likely to be successful than avoidance goals Sometimes our end goal is to decrease something: to lose weight, stop smoking, or eat slightly fewer cookies. In order to increase chances of success, it can be helpful to reimagine these goals as activation goals. Instead of losing weight, we can aim to exercise four days a week. Instead of stopping smoking, we can try to chew gum daily. Instead of eating fewer cookies, we can try to do some push-ups instead. When trying to avoid negative things, it can be hard to find rewards and easy to identify failures. By trying to do positive things, we can enjoy the reward of achieving our goal incrementally. Even small changes can help. Instead of “I resolve to eat no cookies this year” we can set the goal as “I resolve to do a push-up instead of eating a cookie every day.” Eventually, we will focus more on the positive action, the push-up, than the negative one, the cookie. This way our brain will spend more time focusing on the things we resolve to do! When we follow through on a resolution, we are making a behavioral change. These changes are governed by our brain, and mimic changes within it. Some of our most popular resolutions correspond to changes in our reward pathway, called the mesocorticolimbic circuit. This contains several brain structures and is a part of the brain that is hijacked by addictive drugs. Two structures in particular, the nucleus accumbens and striatum, seem to be affected by things like resolutions. Addictive things including sugar decrease these areas’ sensitivity to naturally occurring dopamine. This makes the brain need more and more of those items to find the same level of reward. Lowering sugar, drugs, and alcohol can help restore the dopamine receptors and give your brain a fighting chance. Studies have also shown that exercise increases dopamine sensitivity of the mesocorticolimbic circuit, giving some protection against addictive undesirable behaviors. Other behaviors that we do frequently and repetitively will also make changes to the brain’s pathways, reinforcing the behaviors. So now we know how to structure our resolutions, and how our brain responds to changes, but what can we do to make sure we don’t give up on our resolutions? The most important change is a lifestyle change. This is true with resolutions, but also with weight loss medications, smoking cessation, etc. Changing the triggers for what you want to avoid makes it easier to do the activities you desire. Even small changes – like sitting in a different chair than your preferred cookie-binge recliner – can make the process easier. Along with this, we want to make sure we have strategies to deal with tempting situations. If work has cookies on Fridays, drinking a lot of water can fill your stomach and help alleviate the temptation. Unexpected situations can also arise. If your mother invites you for afternoon tea and biscuits – only for you to learn that “biscuit” is British for “cookie”- having a plan to politely decline can be very handy. Finally, realize that resolutions aren’t all-or-nothing. If I succumb to chocolatey chip temptation and eat a cookie today, it doesn’t mean I’ve failed at my resolution and should give up. Instead of looking at hiccups as failures, look at them as learning opportunities. These are great opportunities to learn what triggered your lapse and practice a strategy to act positively and avoid this trigger in the future. Taken together we have solid starting points for our resolutions. Resolve to do positive actions that you want to accomplish. Structure resolutions to be activation based and give yourself opportunities to celebrate success instead of regretting failure. Give yourself the advantage of changing your lifestyle to accommodate and incentivize your resolution. Give yourself a break when you miss a day and learn how to move forward better tomorrow. When we resolve to do things we want to do, we only have to countdown the days until we celebrate another New Year and a successful resolution! Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Larimer, M. E., Palmer, R. S., & Marlatt, G. A. (1999). Relapse prevention. An overview of Marlatt’s cognitive-behavioral model. Alcohol research & health : the journal of the National Institute on Alcohol Abuse and Alcoholism, 23(2), 151–160. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6760427/ Oscarsson, M., Carlbring, P., Andersson, G., & Rozental, A. (2020). A large-scale experiment on New Year’s resolutions: Approach-oriented goals are more successful than avoidance-oriented goals. PLoS One, 15(12), e0234097. https://doi.org/10.1371/journal.pone.0234097 Trifilieff, P., & Martinez, D. (2014). Imaging addiction: D2 receptors and dopamine signaling in the striatum as biomarkers for impulsivity. Neuropharmacology, 76 Pt B(0 0), 498–509. https://doi.org/10.1016/j.neuropharm.2013.06.031 Wimmer, S., Lackner, H. K., Papousek, I., & Paechter, M. (2018). Goal orientations and activation of approach versus avoidance motivation while awaiting an achievement situation in the laboratory. Frontiers in psychology, 9, 1552. https://doi.org/10.3389/fpsyg.2018.01552
Listen to the article here:
Most of us have heard by now that chocolate is healthy, or that a small amount is healthy, or that you can eat an infinite amount of chocolate and it will be healthy forever. Where do these claims come from, and do they add up? There is evidence of people consuming chocolate up to 1600 years ago. It is native to the Americas and was said to be the “food of the gods” in mesoamerica. Today we think of chocolate as sweet and delicious and the perfect food, but this was not always the case. Chocolate is thought to have originally been mixed with water and drunk as a bitter, spiced beverage. During the 1500’s chocolate was brought to Europe, where it was considered as exotic as Mars. Healers claimed chocolate healed diseases of the liver and stomach, and that it could help with fever. By 1631, chocolate had changed. Adding sugar was now typical, and the prescriptions for chocolate had changed as well. Chocolate in this era was used to help gain weight (likely due to sugar), stimulate the brain (likely due to caffeine), and aid in digestion. Ironically, the same benefits chocolate seemingly presented to chronically underweight pre-industrial people has become a bit of a problem for us. By the mid to late 1800’s there were investigations into the health problems associated with chocolate’s additives – milk and sugar. They found that regularly eating fatty, sugary foods might not be healthy. By the 1900’s chocolate began to be associated with obesity, tooth decay, gum disease, etc. The “dark” chocolate age had begun. By the early 2000’s, the opinion pendulum on chocolate had begun to swing back. Individual components of chocolate, such as flavanols, methylxanthines (Methyl-zan-theens) and polyphenols were shown to be beneficial to heart function in a lab. Since then there have been claims that chocolate helps everything from cardiovascular problems to metabolic ones and even cancer. It looked like chocolate was on a holiday high in medical opinion. Unfortunately, these results may have been candy-coated. Research trials haven’t shown as much benefit as in the lab. One sweet spot picked up by newspapers was an observational meta-study which looked at over 300,000 participants. This study looked for an association between chocolate consumption and coronary artery disease (CAD). They found that people who ate chocolate more than once a week (or more than 3½ times a month) had a significantly lower incidence of CAD, heart attack, heart failure, and acute coronary syndrome. It is important to note that this was not an interventional study, and only looked at associations. Additionally, this didn’t take into account the type of chocolate eaten. Finally, this study found that some negative indicators actually rose, likely due to the extra calories from fats and sugars added to chocolates. The best way to look for health benefits or drawbacks of any medicine is to do an interventional experiment – a clinical trial. This is where you compare groups randomly assigned to take chocolate or a placebo. An examination of 15 such studies where chocolate was the medicine sadly found few benefits. These studies looked for changes in: When looking at all 15 studies, there was no significant change in any of these indicators. The only significant change across studies was a decrease in triglycerides. This can be helpful, as high triglycerides can be a risk factor for CAD, stroke, and pancreatitis. Overall, however, chocolate doesn’t appear to be the miracle drug it’s been touted as for the last millennium and a half. As we have learned countless times, using randomized clinical (interventional) trials is the best and often only way to discover if medicines have the effects people claim! Interventional trials are conducted at clinical research organizations such as ours, ENCORE Research Group. We are a premier clinical research organization that has conducted more than 2,500 clinical trials over 25 years and has worldwide recognition for providing patients access to cutting edge medical research. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Krittanawong, C., Narasimhan, B., Wang, Z., Hahn, J., Virk, H. U. H., Farrell, A. M., … & Tang, W. W. (2021). Association between chocolate consumption and risk of coronary artery disease: a systematic review and meta-analysis. European journal of preventive cardiology, 28(12), e33-e35.https://doi.org/10.1177/2047487320936787 Lippi, D. (2015). Sin and pleasure: the history of chocolate in medicine. Journal of agricultural and food chemistry, 63(45), 9936-9941. Montagna, M. T., Diella, G., Triggiano, F., Caponio, G. R., Giglio, O. D., Caggiano, G., … & Portincasa, P. (2019). Chocolate,“food of the gods”: History, science, and human health. International Journal of Environmental Research and Public Health, 16(24), 4960. https://doi.org/10.3390/ijerph16244960 Tan, T. Y. C., Lim, X. Y., Yeo, J. H. H., Lee, S. W. H., & Lai, N. M. (2021). The health effects of chocolate and cocoa: A systematic review. Nutrients, 13(9), 2909. https://doi.org/10.3390/nu13092909
Listen to the article here:
With the onset of frosty weather and short days, we can all use a boost. Luckily, giving gifts can produce a “warm glow” to help out. This isn’t just decorative talk, giving gifts has been shown to increase well-being in people across the globe. In study after study, psychologists have found that acts of kindness, such as giving gifts, have positive results on both the receiver and the giver. In one study, scientists gave children treats while measuring happiness. The children were then asked to give treats to a puppet. These could be their own treats or ones from a researcher’s supply. The data showed the children were happier to give a treat to the puppet than to receive one for themselves and were happiest when they gave their own treat to the puppet. Overall, the cheer of giving seemed maximized when giving away more important gifts. Why could this be, though? Why would gift giving be beneficial for the person losing something? Could it be that giving a gift clears your already extremely crowded gingerbread house and increases your Feng shui? The real answer is that gift giving is a prosocial behavior. This means that it promotes social acceptance and friendship. This is a positive behavior in social contexts. Prosocial behaviors are seen in several social animals, including apes and dogs. Scientists have shown that giving gifts can increase synchronization between friends. In two studies, scientists hooked pairs of friends up to brain scanning devices. The friends performed cognitive tasks, then one would give the other a gift (at a random time), and they would perform the task again. The scientists found that accuracy on the tasks increased. In addition, activity increased in the dorsolateral prefrontal cortex (DLPFC). This is part of the brain located beneath the hairline (assuming you have hair). It is associated with decision making and memory, and is also implicated in suppressing selfishness and building relationships. This helps with cognitive tasks, but also with forming and maintaining friendships. Even more interesting, they found that the brain waves of friends were synchronizing! The brainwaves measured in the DLPFC would “sync up” and produce similar patterns after gift giving! Giving a gift doesn’t just increase friendship, it helps you think like your friends too! The DLPFC isn’t the only section of the brain that’s active when giving. When giving to charity, people’s mesolimbic reward system and subgenual areas activate. The mesolimbic reward system is a general reinforcement pathway in the brain, and also rewards for things like food, sex, and drugs. The subgenual area releases important hormones such as oxytocin (the love hormone) and vasopressin. These make us feel good and increase our social happiness. So this winter, give gifts to keep yourself warm inside and out. By giving gifts you can increase your own happiness, strengthen bonds with friends, and release dessert-like chemicals in the brain. Also, consider giving the gift of health to others by volunteering for a clinical trial at one of our ENCORE Research Group locations. By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Aknin, L. B., Barrington-Leigh, C. P., Dunn, E. W., Helliwell, J. F., Burns, J., Biswas-Diener, R., … & Norton, M. I. Prosocial Spending and Well-Being: Cross-Cultural Evidence for a Psychological Universal.https://doi.org/10.1037/a0031578 Aknin, L. B., Hamlin, J. K., & Dunn, E. W. (2012). Giving leads to happiness in young children. PLoS one, 7(6), e39211. https://doi.org/10.1371/journal.pone.0039211 Balconi, M., Fronda, G., & Vanutelli, M. E. (2019). A gift for gratitude and cooperative behavior: brain and cognitive effects. Social cognitive and affective neuroscience, 14(12), 1317-1327. https://doi.org/10.1093/scan/nsaa003 Balconi, M., Fronda, G., & Vanutelli, M. E. (2020). When gratitude and cooperation between friends affect inter-brain connectivity for EEG. BMC neuroscience, 21(1), 1-12. Curry, O. S., Rowland, L. A., Van Lissa, C. J., Zlotowitz, S., McAlaney, J., & Whitehouse, H. (2018). Happy to help? A systematic review and meta-analysis of the effects of performing acts of kindness on the well-being of the actor. Journal of Experimental Social Psychology, 76, 320-329. https://doi.org/10.1016/j.jesp.2018.02.014 Moll, J., Krueger, F., Zahn, R., Pardini, M., de Oliveira-Souza, R., & Grafman, J. (2006). Human fronto–mesolimbic networks guide decisions about charitable donation. Proceedings of the National Academy of Sciences, 103(42), 15623-15628. https://doi.org/10.1073/pnas.0604475103
Listen to the article here:
The familiar wub-dub of the heart accompanies us throughout our lives, providing a gentle beat that keeps us alive. But for some of us, the beat might not be so steady. For 33 million people worldwide, the heartbeat lacks a rhythm at all. It sounds like shoes in a clothes dryer and gets progressively worse. This is called Atrial Fibrillation, or AFib for short. The risks of AFib increase with age, and there is a genetic component as well. Other risk factors include: In order for AFib to occur, doctors believe there needs to be a trigger and a substrate. A trigger, or driver, is the electric signal that travels to the heart and initiates an arrhythmic event. This can be from several areas, but is frequently from one of the big pulmonary veins that carry oxygen to the heart. A substrate is the underlying condition that makes a sustained event possible and could be structural or electrical. Common substrates include the electrical system of the heart, dilation (or stretching) of the atrium, cellular-molecular changes, and/or an increase in disruptive cells called fibroblasts. In general, many or all of these changes would occur, leading to constant AFib. AFib is very dangerous. Other than a wonky pulse, there are three major complications: heart failure, stroke, and myocardial infarction (a heart attack). Heart failure is when the heart can’t pump enough blood, while stroke and myocardial infarction can be caused by stray blood clots. Heart failure is both a risk and a symptom, which illustrates one way in which AFib is a progressive disease. Through complicated electric and biocellular mechanisms, long term AFib seems to cause more AFib. Treating AFib has proven difficult. It is effective to treat the underlying risk factors, such as obesity and diabetes, but this is difficult and the actual cause of AFib isn’t always clear. Controlling the rhythm of the heart is also tough and risky, as messing with heart rhythm can easily lead to big problems. Atrial fibrillation ablation is an effective treatment. It is an intensive surgical procedure where doctors scar problem areas to reduce electrical activity. Even with this method, the risk of resurgence is over 30% after 5 years. Two of the biggest complications of AFib are related to blood clots. Because of this – and the difficulty of other treatments – major pharmaceuticals often target thromboembolisms, or clots. The clotting system itself is very complicated. A simple version is that platelets activate and produce several enzymes. These enzymes make thrombin, which makes a big mesh-like protein called fibrin. This would be a slow process, except that thrombin also activates amplifier enzymes, which makes this process very fast. The fibrin then catches red blood cells and blocks wounds – or blood vessels. When these clots travel to the brain they can cause a stroke. When they restrict blood flow to the heart they can cause a myocardial infarction – a heart attack. Classic anticoagulants, such as Warfarin (also called Jantoven and Coumadin) work by stopping the clots before they start. These are Vitamin K dependent anticoagulants and can be effective at reducing clots. Unfortunately, they are occasionally too effective. The biggest side effect of Vitamin K dependent anticoagulants is increased bleeding. This can be a serious problem for several patients, including high-risk older patients. Doctors are investigating new classes of medications which do not depend on vitamin K. These are called Non-vitamin K oral anticoagulants (NOACs) and some target the amplification pathway of clotting instead. There are currently four FDA-approved NOAC drugs on the market; dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). Thrombin and fibrin still get produced and some clotting can occur, but the rapid amplification is shut down. The hope is that this can allow the body to repair trauma and stop external bleeds without building internal clots from AFib. With your help and participation in clinical trials, we can push science without pushing clots. By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Iwasaki, Y. K., Nishida, K., Kato, T., & Nattel, S. (2011). Atrial fibrillation pathophysiology: implications for management. Circulation, 124(20), 2264-2274. https://doi.org/10.1161/CIRCULATIONAHA.111.019893 Wijesurendra, R. S., & Casadei, B. (2019). Mechanisms of atrial fibrillation. Heart, 105(24), 1860-1867. http://dx.doi.org/10.1136/heartjnl-2018-314267 Vann, M. R. (May 10, 2013) The Sound of an Afib Heartbeat. Everyday Health. https://www.everydayhealth.com/heart-health/sound-of-afib-heartbeat.aspx
Listen to the article here:
Clostridioides difficile, C. difficile, or just C. diff is a particularly nasty bacteria that can make us very sick. The bacteria itself has the name difficile because it was difficult to isolate and study when it was first discovered. Forms of the problem bacteria are found all over the environment, but most can’t make us sick. The organism itself doesn’t kill cells like a virus; instead, it can produce toxins that can kill cells in the gut. C. diff has over 800 different strains, but only a few produce dangerous toxins. Overall, C. diff causes dangerous infections in hundreds of thousands of patients each year. Several people have C. diff inside their gut already, but it doesn’t cause them problems. Other bacteria in our gut can outcompete C. diff and keep it from causing damage. Unfortunately, one of the biggest medical breakthroughs, antibiotics, can destroy these helpful bacteria and allow C. diff to start running amok. In fact, any kind of immunosuppression can increase your risk of developing C. diff, including HIV/AIDS medications and those used after organ transplants. Being above 65 years old is another large risk factor. Close contact with some animals, like pigs, can also pose a risk. The most dangerous forms of C. diff are spread from person to person. This occurs with our most vulnerable populations: those in hospitals and those in elderly care. Due to the innate nature of care, people in hospitals and care homes can be exposed to C. diff unknowingly. How does C. diff survive in the notoriously clean hospital environment? The bacteria has a special trick up its sleeve; it can become dormant – and almost invincible. C. diff has two life cycle stages, the spore and vegetative stage. While in the spore stage, C. diff is inactive. It doesn’t need to eat or breathe. While in this stage it can survive in the environment, the stomach, through most antibiotics, and through alcohol washes. When a C. diff spore makes it into our gut, however, trouble can begin. It germinates in the duodenum – the part of the intestine connected to the stomach. Here it transforms into the vegetative stage. In the vegetative stage, C. diff is active. It can’t survive the stomach or in oxygen, but thrives in the intestines. Here it grows and reproduces. This is also where some strains produce dangerous toxins. The toxins of C. diff can produce a host of issues. The toxins can degrade and kill intestinal cells and cause inflammation of the intestines. Major symptoms are diarrhea, inflammation of the gut, and tissue necrosis (cell death). Other symptoms can include: So what can be done to fight C. diff? The first line of defense is the simplest: wash your hands! Prevention is the strongest barrier: avoid close contact with people who have an active infection and wash clothes and linens regularly. A medical professional (who should be wearing gloves!) can monitor any antibiotics an infected person is currently taking and might suggest probiotics. Some specific antibiotics target C. diff, including Metronidazole, Vancomycin, and Fidaxomicin. These may have unpleasant side effects, but can be effective. Treatments available include fecal microbiota transplantation (FMT), antitoxins, new antibiotics, and injectable antibodies. Additionally, prophylactics that can help protect the gut and vaccines against the dangerous toxins are in development. Keep an eye out, and with your participation in clinical trials, we can help protect those at the highest risk from C. diff! By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Dayananda, P., & Wilcox, M. H. (2019). A review of mixed strain Clostridium difficile colonization and infection. Frontiers in microbiology, 10, 692.https://doi.org/10.3389/fmicb.2019.00692 Smits, W. K., Lyras, D., Lacy, D. B., Wilcox, M. H., & Kuijper, E. J. (2016). Clostridium difficile infection. Nature reviews Disease primers, 2(1), 1-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5453186/ U.S. Department of Health & Human Services/Centers for Disease Control and Prevention (September 7, 2022). What is C. diff https://www.cdc.gov/cdiff/what-is.html
Listen to the article here:
When EMTs arrive on the scene of an emergency, they have to remember their ABCs. These are Airway, Breathing, and Circulation. The absolute top priority for any patient is to ensure they have an open airway to breathe, that air is entering the lungs, and that the heart is pumping blood to the brain and other organs. This is also the most important thing our body does in daily life as well. We can go weeks without food, days without water, hours without ice cream, and minutes without oxygen. In order to get oxygen from the lungs to our brain and organs, we rely on one of the most remarkable organs in our body: the heart. The heart pumps automatically, nonstop, 24/7, from womb to grave. It consists of four chambers, two on top, and two on the bottom. Each heartbeat pulls blood into the top two chambers and pumps it out of the bottom two. The bottom two are more muscular and do the heavy lifting. Unfortunately, the heart can deteriorate and lead to heart failure. Heart failure is a condition where the heart can’t pump well enough to deliver oxygen to the organs effectively. The heart is still pumping, but organs are not receiving enough oxygen to function. This is not good. Heart failure affects over six million Americans and ten times as many people worldwide. Risk factors for heart failure include: Heart failure has several signs and symptoms. Some of the most consistent are edema and shortness of breath. Edema is fluid trapped in the body’s tissues and most often pools in the lower extremities and the abdomen. Shortness of breath is due to the heart failing to deliver enough oxygen. This is particularly prevalent when trying to do activities or when lying down. Shortness of breath can keep patients from exercising or sleeping, which only exacerbates problems. Patients who have limited exercise in their routine may not be aware of progressive difficulty, masking this important symptom. Other symptoms can be broad and nonspecific. They include: If you have heart failure and find yourself experiencing several of these conditions simultaneously, especially with edema and shortness of breath, we urge you to contact your physician immediately. Additionally, you may want to keep track of your level of fatigue because this symptom increases as the heart failure progresses. The excellent news is that new and exciting monitoring devices are currently being developed to help patients manage their heart failure and determine if their condition is deteriorating. Check out clinical research options available to you with ENCORE Research Group on our enrolling studies page. By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Albert, N., Trochelman, K., Li, J., & Lin, S. (2010). Signs and symptoms of heart failure: are you asking the right questions?. American Journal of Critical Care, 19(5), 443-452. https://doi.org/ajcc2009314 Groenewegen, A., Rutten, F. H., Mosterd, A., & Hoes, A. W. (2020). Epidemiology of heart failure. European journal of heart failure, 22(8), 1342-1356. https://doi.org/10.1002/ejhf.1858 U.S. Department of Health & Human Services/Centers for Disease Control and Prevention (October 14, 2022). Heart failure https://www.cdc.gov/heartdisease/heart_failure.htm
Listen to the article here:
We all know how Thanksgiving works. A giant meal with a giant turkey followed by tasty desserts. Then, after the meal, sleepiness sets in. But why? We usually blame the turkey and the tryptophan in the protein. But I’m a vegetarian, and I still get the post-thanksgiving snoozies. So, what is tryptophan, and does it make us tired, or is there something else to blame? This article contains a cornucopia of information to help answer these questions. Tryptophan is an essential amino acid. Amino acids are the building blocks of proteins and are baked into many of the body’s needs. Being an “essential” amino acid means that we can’t create our own tryptophan and must instead gather it from the foods we gobble up. We need some tryptophan in our diet because it is used to create some critical molecules our body uses. Two of these important molecules are the neurotransmitter serotonin and the hormone melatonin. These are critical little molecules derived from tryptophan and – interestingly, both interact with our sleep cycle. Serotonin acts on parts of the brain involved with learning, pain, social behavior, and sleep, among many others. Melatonin is like turkey dressing; it’s harvested further from serotonin and can increase sleepiness. Neither of these gets produced in large quantities after eating turkey, however. The large amount of other amino acids found in turkey protein keep tryptophan from making a pilgrimage to the brain after a meal because the amino acids compete for rides on the path to our brain. So then, why do we feel tired after a big Thanksgiving meal? Well, one reason might be linking carbs (sugars) to tryptophan. Some carbohydrates can increase the ability of tryptophan to cross into the brain and get serotonin and melatonin cooking. Additionally, heavy carbohydrate intake has been associated with higher levels of tiredness and lower levels of alertness. This can be attributed to the rise in blood sugar from the heavy carbohydrates which is followed by release of insulin to lower the blood sugar. The lower blood sugar causes you to feel tired. So too much dessert might be resulting in a blood sugar crash after the meal. In fact, too much of everything may be making you tired. When we eat large meals, the body activates the parasympathetic nervous system. This is also known as the “rest and digest” pathway, and does exactly what it sounds like. After a large meal, the body focuses on relaxation and digestion. This can cause extra blood flow into the stomach and can make you less alert and awake. Turkey may get too much blame for our tiredness. As my sweet tooth will attest, the desserts may be a bigger culprit. So, this Thanksgiving, feel free to gather the family to feast (and nap) as you please, but squash the blame on the turkey! Written by: Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Ballantyne, C. (2007). Does Turkey Make You Sleepy? Scientific American. https://www.scientificamerican.com/article/fact-or-fiction-does-turkey-make-you-sleepy/ Høst, U., Kelbaek, H., Rasmusen, H., Court-Payen, M., Christensen, N. J., Pedersen-Bjergaard, U., & Lorenzen, T. (1996). Haemodynamic effects of eating: the role of meal composition. Clinical Science, 90(4), 269-276. Mantantzis, K., Schlaghecken, F., Sünram-Lea, S. I., & Maylor, E. A. (2019). Sugar rush or sugar crash? A meta-analysis of carbohydrate effects on mood. Neuroscience & Biobehavioral Reviews, 101, 45-67. Vreeman, R. C., & Carroll, A. E. (2007). Medical myths. Bmj, 335(7633), 1288-1289.
Listen to the article here:
Several of my friends hate flossing their teeth. They go months without flossing, which I think is pretty gross. But then an odd thing happens. About a week before their dental appointment, these same friends will start flossing. By the time they reach their appointment, they have unusually clean gums (though dentists can see through this fairly well, I’m told). On a different tone, some family members have a condition called White Coat Syndrome. When they go to the doctor’s office, their nervousness causes a spike in blood pressure or heart rate, giving deceptively high readings. What’s going on? Can psychological effects like these be used to our advantage?
The Hawthorne Effect is a term used to describe a very beneficial effect seen in clinical trials. This is named after a productivity study in Hawthorne Works, a Western Electric factory in the 1920s and 30s. The study was attempting to discover a link between the amount of light and productivity of workers. When increasing the amount of light, productivity increased. Strangely, when lowering the amount of light, productivity also increased! Researchers attributed the increase in productivity to the workers simply being observed. In research, we tend to see increased positive results for patients simply because we are observing them in a study.
Hawthorne Works
Let’s analyze a 2014 sleep study. Researchers measured 195 patients’ amount and quality of sleep at night. 81 days later, before any medical intervention, researchers measured the patients again. They found that patients slept an average of 30 minutes longer per night and had an increased quality of sleep. This was before any medication or intervention! The change was attributed to the Hawthorne Effect. Patients at ENCORE Research Group comment on the excellent quality of care they receive during clinical trials. Instead of seeing a doctor for a few minutes once a year, patients see doctors and medical staff for much longer and are encouraged or required to call and report changes in health. Quality of care is increased and makes for a pleasant and healthful patient experience. Patients in clinical trials may also experience more observation time from medical professionals due to the attention to detail that clinical trials require for data integrity in studies. Finally, patients are found to have better adherence to medication requirements while undergoing clinical trials. The increased emphasis on accuracy and adherence results in better patient outcomes, even when they are part of a placebo or standard-of-care group. In clinical trials, we see these benefits and must account for them. Randomization of patients helps spread the effect. Everyone sees increased baseline results on average; we are interested to find out if those receiving investigational treatment do even better. Join a clinical trial today and experience the Hawthorne Effect for yourself… and floss your teeth! Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Benedetti, F., Carlino, E., & Piedimonte, A. (2016). Increasing uncertainty in CNS clinical trials: the role of placebo, nocebo, and Hawthorne effects. Lancet Neurol, 15, 736-47. http://dx.doi.org/10.1016/S1474-4422(16)00066-1 Cizza, G., Piaggi, P., Rother, K. I., Csako, G., & Sleep Extension Study Group. (2014). Hawthorne effect with transient behavioral and biochemical changes in a randomized controlled sleep extension trial of chronically short-sleeping obese adults: implications for the design and interpretation of clinical studies. PLoS One, 9(8), e104176. https://doi.org/10.1371/journal.pone.0104176 ENCORE Research Group. (2020, October 14). Hawthorne effect.[Video]. Youtube. https://www.youtube.com/watch?v=1DH7jwqFlyw Mayo, E. (1993). The human problems of an industrial civilization. The Macmillan Company. McCarney, R., Warner, J., Iliffe, S., Van Haselen, R., Griffin, M., & Fisher, P. (2007). The Hawthorne Effect: a randomised, controlled trial. BMC medical research methodology, 7(1), 1-8. https://doi.org/10.1186/1471-2288-7-30
Listen to the article here:
The liver is critical to maintain body function. Unfortunately, millions of Americans suffer from liver disease. When the liver suffers prolonged damage, scarring can form. This scarring, called cirrhosis, is debilitating and reduces liver function. Cirrhosis is sometimes called end stage liver disease, and is irreversible. On its own, cirrhosis can be painful and cause suffering, but is frequently made worse through complications. One of these is encephalopathy. Encephalopathy is a broad term used to describe several diseases and disorders. The unifying concept is that these diseases change the brain’s structure or function. When the cause of this change is through cirrhosis, the condition is called hepatic encephalopathy. This is the condition caused by cirrhosis of the liver, and can be horrible. It comes with a high mortality rate, over 25%, and affects over 30% of people with cirrhosis. The full mechanism of how hepatic encephalopathy works isn’t fully known. The most likely candidate for hepatic encephalopathy is a buildup of ammonia in the bloodstream. Ammonia is a common waste product for many cells. A damaged liver has trouble filtering ammonia from the blood. The ammonia accumulates in the blood where it can travel to the brain and cause confusion and disorientation at first. Additionally, liver damage can result in reduced muscle mass and immunosuppression. Muscles can remove excess ammonia from the blood, but may become damaged without a functional liver and be unable to help. A reduced immune system can lead to a buildup of harmful bacteria that produce excess ammonia. These combine to create excess toxic levels of ammonia in the bloodstream that make their way to the brain. The brain is normally protected from toxins in the blood through the blood brain barrier. Astrocytes are special cells in the brain that surround blood vessels and help filter the blood, letting only specific nutrients and particles through. Excess ammonia in the blood appears to damage astrocytes, with wide ranging effects on the brain. When the blood-brain barrier is reduced, toxins can enter the brain. This can lead to damage in neurotransmission, meaning the brain cannot function effectively. There is also an increased chance of infection in the brain and alterations to brain metabolism. This is a devastating compilation which can drastically reduce quality of life. In the early stages of hepatic encephalopathy, people may experience a general slowing of the brain. This is noticeable in attention, some motor response, and other vague areas. As the encephalopathy progresses, people experience more severe symptoms. Changes in personality have been reported, such as irritability and impulsivity. They may angrily buy m&ms in the checkout line. It also slows the brain and reduces its ability to function. People may become disoriented, experience distortions of time and space, become excessively sleepy, and descend into a coma. Clearly this condition needs medical attention! Luckily, hepatic encephalopathy can be reversible in many patients! The most important short-term treatment is to get rid of excess blood ammonia. The current standard of care is lactulose, a chemical that binds to ammonia and expels it rectally. This helps in the short term, and can also be recommended to help reduce recurrence. Though effective, lactulose is a laxative and can cause bloating, cramping, and other undesirable side effects. Because of this, many patients don’t like using this drug long term. Since the immune system is suppressed with cirrhosis, antibiotics may help as well. In fact, antibiotics may be helpful in preventing hepatic encephalopathy in the first place by eliminating harmful, ammonia producing bacteria before they can produce too much ammonia. Used with or without probiotics and drugs that help restore normal brain chemistry, we may be able to lower the burden of hepatic encephalopathy for those who suffer. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Bustamante, J., Rimola, A., Ventura, P. J., Navasa, M., Cirera, I., Reggiardo, V., & Rodés, J. (1999). Prognostic significance of hepatic encephalopathy in patients with cirrhosis. Journal of hepatology, 30(5), 890-895. https://doi.org/10.1016/s0168-8278(99)80144-5 Ferenci, P. (2017). Hepatic encephalopathy. Gastroenterology report, 5(2), 138-147. https://doi.org/10.1093/gastro/gox013
Listen to the article here:
In science and medicine we measure if and how well things work using measurements. This idea may sound simple, but it’s often a challenge to find out exactly what to measure – and how. We typically measure things that can change – things that can vary. We call these things variables. Variables can be broadly split into two major categories: dependent and independent. Either type of variable can change, the difference is what changes them. Independent variables are changed by researchers, particularly in clinical (patient) research. This variable in a medical research study is what we are testing. The changes to an independent variable may include dose, length, and method of drug delivery. We evaluate independent variables that may change outcomes of the people in a study – but sometimes they do not. In order to understand the effect of medicines, researchers test the medicine against a control. The control could be a placebo (something that has no effect) or a standard of care (the current normal medicine). Dependent variables are what we expect to change during a trial. In a clinical research, we may expect changes in blood pressure, cholesterol levels, disease symptoms, mortality, and other categories. In a well designed study, we assess changes in the dependent variables related to changes in the independent variables. There is always the chance that the dependent variables are changed by other things, however. A patient might take a new blood pressure medicine but retire from their job. The reduced stress could decrease their blood pressure even if the medicine did not. Because of individual changes in people’s circumstances, researchers use statistics to find trends. If your blood pressure medicine was only studied on the one person above, you might have erroneous results. Instead clinical trials have dozens, hundreds, or even thousands of participants. With large populations these little differences get figured out. One person might retire, but another might get fired, having an opposite effect. Altogether, statistical analysis can help discover if any changes in the dependent variable are due to the effects of the independent ones.
Chart 1. Each amount of Rosuvastatin on the left corresponds to an amount of LDL on the right. The dependent variable (LDL levels) change in proportion to the amount of independent variable (rosuvastatin) taken by the patient.
Other variables exist in a study. The most concerning of these variables is known as a confounding variable. This is a variable that can undermine the study at a fundamental level. A confounding variable can be introduced by researchers and might include things like placing all overweight patients in the 10 mg group and all underweight people in the placebo group. ENCORE Research Group (and any legitimate clinical research group) avoids confounding variables and bias by randomizing patients. Patients are randomized through an impartial method (usually a computer program) which will randomly place patients into any of the test groups. By randomizing patients, we can avoid the most concerning confounding variables and make sure we are studying what we intend to! To learn more about the clinical trial process, call our Recruitment Team at (904) 730-0166. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Schweiger, C. (2003). Clinical trials with rosuvastatin: efficacy and safety of its use. Italian Heart Journal: Official Journal of the Italian Federation of Cardiology, 4, 33S-46S. https://pubmed.ncbi.nlm.nih.gov/14983745/ Stewart, P. A. (1978). Independent and dependent variables of acid-base control. Respiration physiology, 33(1), 9-26. https://www.nlm.nih.gov/nichsr/stats_tutorial/section2/mod4_variables.html
Listen to the article here:
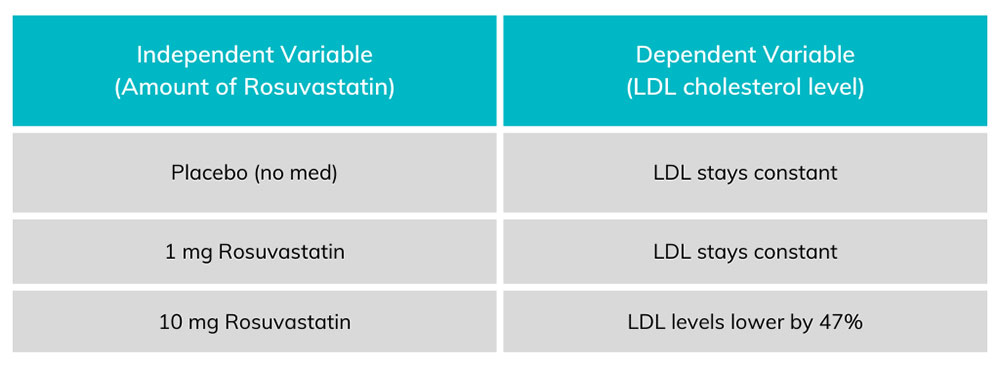
A pandemic spread around the planet in the first quarter of the century. Not this century, however, but the last. The 1918 Flu Pandemic was the largest and deadliest outbreak of disease since the bubonic plague in the 1300s. The first official reported case was in Kansas in 1918. This gives the disease its proper name, the 1918 Influenza Pandemic. A much more common name, however, is the Spanish Flu. The name Spanish Flu is an unfair name. Spain lost around a quarter million people to the 1918 Influenza. This is less than half as many as the USA, and fewer than Afghanistan, Mexico, Russia, Italy, and Japan. On top of that, India lost somewhere above 18 million people, and China between four and nine million. The big difference in losses was due to Spain being neutral during World War I. Because of this, they weren’t shy about publishing accurate data. Spain was the first country to publicly disclose that the pandemic was real, and other countries underreported or lied about numbers for years. This may strike some as familiar; during the COVID-19 pandemic, several national and local governments around the world tried to downplay the severity of COVID for political gain. But what is influenza? Influenza, known as the flu, is very similar to COVID-19 in many ways. It is a viral infection, and its primary symptoms are cough, fever, joint pain, headache, body aches, and others. However, more serious complications such as pneumonia, liver damage, or brain problems can be triggered by influenza. It spreads through the air and can survive in water. Soap, changes in pH, and heat can destroy the influenza virus. The most dangerous part of influenza is how variable it is. The influenza virus has several subtypes, and each of these mutates constantly. This makes it hard for the immune system to detect and fight new forms of the virus. It also means the specific symptoms of infections can change. In the 1918 influenza pandemic, the strain of influenza was particularly deadly for young, healthy people. This resulted in a lot of excess deaths compared to other strains. The 1918 Influenza Pandemic was made much worse because of World War I. The war resulted in overcrowded barracks, troops stuffed in ships, and people crowding in shelters. Additionally, it spread wide and far as governments deployed troops around the world. A lack of accurate reporting and proactive measures certainly didn’t help. The biggest difference between then and now was medicine. 1918 was over a hundred years ago, but in the realm of medicine, it may as well have been much longer. Viruses were only discovered around 20 years prior, and there were no effective ways to fight them. There were no antiviral medications. For patients that developed pneumonia, there were no ventilators and no antibiotics. On top of this, there was no influenza vaccine. The “Spanish flu” of 1918 helped refocus medical attention around pandemics – particularly influenza. In the early 1930s new vaccines were being developed from chicken eggs, and less than ten years later, the first experimental influenza vaccines were developed. Today, our yearly flu shots come from a direct line of response from the 1918 influenza pandemic. A century later, we have come a long way with medical advances, and since we know the influenza virus mutates regularly, the best way to help continue the fight against it is to participate in a clinical trial for the latest flu vaccines. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Hayden, F. G., & Palese, P. (2009). Influenza virus. Clinical virology, 943-976. Jester, B., Uyeki, T. M., Jernigan, D. B., & Tumpey, T. M. (2019). Historical and clinical aspects of the 1918 H1N1 pandemic in the United States. Virology, 527, 32-37. Johnson, N. P., & Mueller, J. (2002). Updating the accounts: global mortality of the 1918-1920″ Spanish” influenza pandemic. Bulletin of the History of Medicine, 105-115. Knobler, S. L., Mack, A., Mahmoud, A., & Lemon, S. M. (2005). The threat of pandemic influenza: are we ready? workshop summary. Mayer, J. (29 January 2019). “The Origin Of The Name ‘Spanish Flu’”. Science Friday. Retrieved 30 July 2021. https://www.sciencefriday.com/articles/the-origin-of-the-spanish-flu/ CDC, National Center for Immunization and Respiratory Diseases. (September 28, 2022). Similarities and Differences between Flu and COVID-19. https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm
Listen to the article here:
How does the body use energy? After we eat, most food is broken down into parts that cells can use for energy. The bloodstream carries these pieces through the bloodstream to our cells, which let them in and convert food to energy. In some cases, the cells don’t let food particles in. In these cases, the problem may be diabetes. Cells need to separate their insides from the environment around them. Cells only let in specific molecules at specific times. Insulin is the molecule that tells cells to let in sugars in the form of glucose. It is produced by the pancreas and is released when the pancreas detects high levels of sugars in the blood. In some cases, such as with obesity, fatty acids can disrupt how cells absorb and use sugar in the blood. When this happens, cells are less sensitive to insulin and absorb less blood sugar per unit of insulin in the blood. Since blood sugar stays high, the pancreas produces more and more insulin, which has less and less effect. Cells can’t respond to all the excess insulin and are increasingly resistant to its effects. Insulin is also the hormone the pancreas uses to communicate with the liver about blood sugar. When the liver detects insulin it converts blood glucose into glycogen, a short term storage molecule. When high levels of insulin persist, the liver sends extra energy to fat cells. After long periods of insulin resistance, the pancreas itself stops working properly. Pancreatic cells become damaged and unable to produce insulin. This is called Type 2 Diabetes (T2D). With T2Ds, blood sugar stays high, insulin stops being produced, any produced insulin is less effective, and cells stop metabolizing properly. On top of this, the body gains excess weight which can stress the pancreas further. Other symptoms include cardiovascular disease, nerve dysfunction in the extremities (called neuropathy), and increased chance of death. Diabetes is very common in the United States. Tens of millions of Americans have T2D. Type 1 diabetes is an autoimmune disorder which results in pancreatic damage. Type 2 diabetes is an insulin resistance disorder and can have a slow onset. Major risk factors are obesity and lack of exercise. These should be the first steps to managing T2D as well. When a healthy diet and exercise aren’t enough to manage healthy blood sugars, or aren’t an option, several key medications exist to help with type 2 diabetes: Altogether, there are several medications which may be helpful for controlling type 2 diabetes. Discovering how these medications interact, lowering side effects, and finding treatments that are easy and straightforward is key. If you have type 2 diabetes, look for enrolling studies soon and improve your diet and exercise if possible! Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Berg, J. M., Tymoczko, J. L., & Stryer, L. (2012). Biochemistry (7th Ed., pp 798-803). New York: W. H. Freeman and Company DeFronzo, R. A., Ferrannini, E., Groop, L., Henry, R. R., Herman, W. H., Holst, J. J., … & Weiss, R. (2015). Type 2 diabetes mellitus. Nature reviews Disease primers, 1(1), 1-22. https://www.nature.com/articles/nrdp201519 Olokoba, A. B., Obateru, O. A., & Olokoba, L. B. (2012). Type 2 diabetes mellitus: a review of current trends. Oman medical journal, 27(4), 269. http://doi.org/10.5001/omj.2012.68 Rena, G., Hardie, D. G., & Pearson, E. R. (2017). The mechanisms of action of metformin. Diabetologia, 60(9), 1577-1585. https://doi.org/10.1007%2Fs00125-017-4342-z U.S. Department of Health & Human Services/Centers for Disease Control and Prevention (August 10, 2021). Insulin Resistance and Diabetes https://www.cdc.gov/diabetes/basics/insulin-resistance.html U.S. Department of Health & Human Services/Centers for Disease Control and Prevention (December 16, 2021). Type 2 Diabetes https://www.cdc.gov/diabetes/basics/type2.html Witters, L. A. (2001). The blooming of the French lilac. The Journal of clinical investigation, 108(8), 1105-1107.https://doi.org/10.1172%2FJCI14178
Listen to the article here:
Methods used to diagnose Alzheimer’s disease are changing. In the past, the only definitive way to diagnose Alzheimer’s disease was after death, by an autopsy, which is not exactly helpful for treatment. The autopsy would reveal both amyloid plaques and tau tangles in the brain; these are hallmarks that characterize Alzheimer’s disease. Thankfully, science has drastically improved over the years. We currently have spinal fluid tests that look for these two key biomarkers and imaging tests that show changes in the brain. A recent example of other evolving diagnosis methods is COVID-19. Early in the pandemic, when there were no COVID-19 tests, the only way to know if someone might have the virus was to check for a fever. Nowadays, we look for biomarkers – such as with a rapid antigen test – which can detect antigens to the virus even in asymptomatic people. We now understand that a person can be suffering from the progressive nature of Alzheimer’s even if they do not yet show signs of cognitive impairment. Without biomarker testing, most patients’ first symptoms are memory loss, including long and short-term. Alzheimer’s is usually associated with increased age because the biological underpinnings of the disease accumulate over time. Diagnosis can be made by using something called the ATN framework. This framework describes the two major proteins involved, amyloid plaques and tau tangles, and the associated neurodegeneration – changes in the brain structure.
Let’s discuss the AT part of ATN: the two protein accumulations called amyloid plaques and tau tangles. It is no coincidence that these are also the biomarkers sought by scientists and doctors when diagnosing Alzheimer’s. Amyloid plaques are bundles of protein that build up outside of cells in the brain. They disrupt how cells connect and communicate with each other. Tau tangles are proteins found inside the neurons. In a healthy neuron, tau proteins help stabilize the microtubule that transfers nutrients. In Alzheimer’s patients, the tau proteins become corrupted and tangled, blocking the neuron’s transport system. This leads to cell death. As more cells die and neural network connections break down, areas in the brain begin to shrink. In the late stages of Alzheimer’s disease, there is widespread loss of brain volume.
The N of ATN is neurodegeneration which is the deterioration of neurons causing specific structural changes to the brain. A structural MRI and a radioactive PET scan are two classic methods of determining neurodegeneration. These are effective as staging tools, discovering how far along the disease has progressed. They are effective but can be expensive and time-consuming. The good news is that researchers are currently working on blood tests that will hopefully be able to detect tau biomarkers quickly and easily. A blood test should be easy, cheap, and relatively simple. With luck, these early biomarker findings will also help drive the effectiveness of clinical therapies, paving the way for better Alzheimer’s treatments in the years to come. By Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Kandel, E. R., Schwartz, J. H., Jessell, T. M., Siegelbaum, S., Hudspeth, A. J., & Mack, S. (Eds.). (2000). Principles of neural science (Vol. 4, pp. 1149-1159). New York: McGraw-hill. Largent, E. A., Wexler, A., & Karlawish, J. (2021). The Future Is P-Tau—Anticipating Direct-to-Consumer Alzheimer Disease Blood Tests. JAMA neurology, 78(4), 379-380. https://doi.org/10.1001/jamaneurol.2020.4835 Ossenkoppele, R., Reimand, J., Smith, R., Leuzy, A., Strandberg, O., Palmqvist, S., … & Hansson, O. (2021). Tau PET correlates with different Alzheimer’s disease‐related features compared to CSF and plasma p‐tau biomarkers. EMBO molecular medicine, 13(8), e14398. https://doi.org/10.15252/emmm.202114398 Peterson, R. C. [UCI MIND] (2019, April 3). Diagnosis of Alzheimer’s disease in the era of biomarkers – Ronald C. Petersen, MD, PhD [Video]. Youtube. https://www.youtube.com/watch?v=KtS5xynes2M What Happens to the Brain in Alzheimer’s Disease? (2017, May 16) National Institute on Aging. https://www.nia.nih.gov/health/what-happens-brain-alzheimers-disease
Listen to the article here:
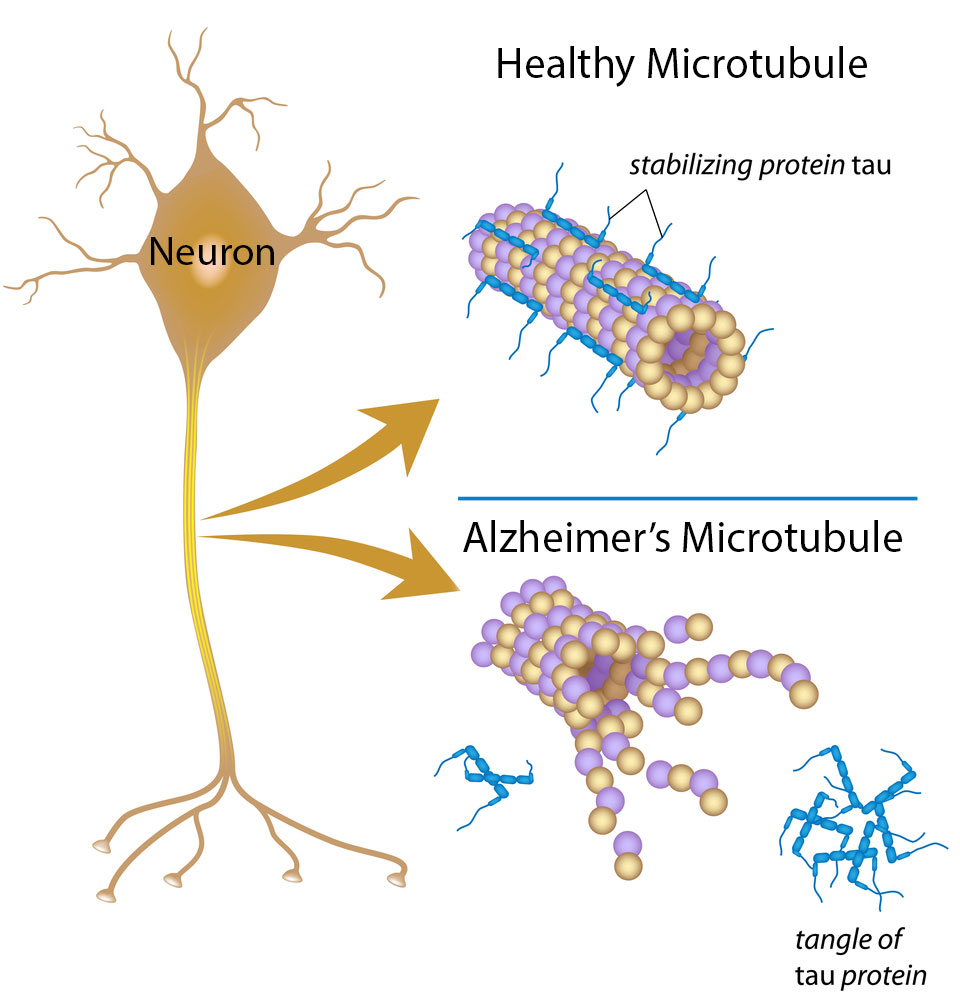
Imagine if your plumbing stopped up. Not your toilets, but your sink and shower. How would you get rid of the dirt and junk off your skin? How would you make sure you stay clean? Our kidneys ask this question every day. The blood in our body travels around and around, including the critical filtration stage of the kidneys. The kidneys act as a big two-way filter. Impurities and excess minerals or water are extracted from the blood, and necessary minerals or water are added as needed. The kidneys keep the ingredients of blood at healthy levels. Finally, kidneys get rid of waste products and extra water by producing urine. When this goes wrong, your blood can’t function properly and waste products can build up. When dealing with the kidneys, you may see three terms thrown about. The origin of “kidney” is unknown, but likely English. “Renal” is the Latin word for kidneys, and the prefix “nephro-” is Greek in origin. If you see any of these terms you can bet we’re dealing with the kidneys. With this in mind, when the kidneys fail to perform their job, we call it renal insufficiency. There are two major divisions in how the kidneys fail, based on the amount of time. There are several possible causes of renal impairment. The vast majority of causes are “upstream,” meaning something affects the blood before it gets to the kidneys. In acute cases, this can be hypotension – not enough fluid, some drugs, such as NSAIDs, or organ failure. When there isn’t enough fluid in the bloodstream, the kidneys compensate by releasing more water, which can deplete the kidney’s reserves and cause failure. In chronic kidney disease, the most frequent cause is diabetes, especially type 2. Prolonged hypertension, and vascular diseases can also be the culprit. With chronic cases, the kidneys will do their best to compensate – constantly filtering out excess blood sugar, for instance. Over time, the excess sugar damages the blood vessels in the kidneys. Some parts of the kidneys may fail and the remaining portions get stressed and eventually decompensate. This is when the kidney fails as an organ. Other possible causes of renal impairment are contained in the kidneys and “downstream” blockages. The kidneys themselve can be the victim of disease or injury, possibly due to long term upstream stress. The ability of the kidney to release urine can also -in rare cases – be disrupted. Regardless of the cause, renal impairment is very dangerous. The kidneys are responsible for keeping blood healthy. A failure of the renal system can result in a need for dialysis or transplant. Dialysis is when external technology filters blood and maintains levels. This is uncomfortable, cumbersome, and expensive. Fixing renal impairment can be a tall order. The most important step is usually treating the underlying cause. Since the kidneys filter several drugs out of the bloodstream, stopping or replacing them may be key. Fluids may need to be replaced in acute cases, and lifestyle changes may be needed in chronic ones. Maintaining healthy blood sugar levels can be key if the root cause is diabetes. For heavily progressed chronic renal impairment, dialysis or transplant may be the only options. Transplant and dialysis are not fun, so we should try to avoid renal impairment before it starts. Many of the tactics to keep your kidneys healthy are the same to keep the rest of your body healthy. Exercise, not overindulging on sugar, and keeping your diet under control can help. Additionally, maintaining a healthy blood pressure is vital. Finally, lowering or cutting out tobacco and alcohol can help keep your kidneys healthy. When it comes to filtering your blood, give your kidneys every advantage you can! By Benton Lowey-Ball, BS Behavioral Neuroscience
Adapted from: Bindroo, S., & Rodriguez, Q. BS; Challa, HJ Renal Failure. (February 24, 2022). StatPearls; StatPearls Publishing: Treasure Island, FL, USA. https://www.ncbi.nlm.nih.gov/books/NBK519012/
Listen to the article here:
Heart failure is quite frankly, a terrifying sounding condition. It is severe, but not as immediately drastic as it sounds. Put simply, heart failure is when the heart fails to pump as much blood as the body will need long-term. The heart works like a balloon, filling with blood and contracting to pump it out. Ejection fraction is a term used to describe the amount of blood pumped out compared with the total the heart can hold. In a normal heart, 50-70% of blood is ejected with each heartbeat. When this amount falls below 40%, a person has a reduced Ejection Fraction (the rEF of HFrEF). This is a serious condition. The heart pumps blood to every cell in the body. This is how cells receive oxygen and nutrients, and how they get rid of waste products. Without enough blood, cells suffocate. Oxygen isn’t reaching cells and the brain interprets this as being short of breath. Common symptoms of HFrEF include: Inside the body, doctors can also look for diagnostic markers. These may include structural changes to the heart and increased natriuretic peptides. Natriuretic peptides are hormones that regulate the amount of salt and water in the blood. They act as vasodilators, opening blood vessels which can be helpful in compensating for heart failure. The body attempts to compensate for the loss of oxygen and nutrients in the blood in many ways, but long term the body has trouble sustaining with heart failure. Who is at risk of developing HFrEF? Unfortunately, it is more prevalent in the United States than almost anywhere else, affecting 6.5 million Americans each year. Risk factors include age, being male, obesity, and smoking. Additionally, other medical conditions increase your risk of developing Heart Failure with reduced Ejection Fraction. Previous heart attacks, coronary heart disease, diabetes, and hypertension are some associated conditions. All told, HFrEF leads to around a million hospitalizations every year, and being hospitalized for HFrEF comes with a low 5-year survival rate. What can be done? There are several methods of dealing with a reduced ejection fraction. Some methods treat symptoms, such as diuretics, and others can help reduce mortality, such as beta-blockers. There are several other medications and even some implantable devices that can help with HFrEF. These can help improve your ejection fraction or health outcomes but are not yet a silver bullet. New medications with increased outcomes and fewer side effects are entering clinical trials and may help with the underlying condition. To learn more about current heart failure research options, call our office today. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Bloom, M. W., Greenberg, B., Jaarsma, T., Januzzi, J. L., Lam, C. S., Maggioni, A. P., … & Butler, J. (2017). Heart failure with reduced ejection fraction. Nature reviews Disease primers, 3(1), 1-19. https://www.nature.com/articles/nrdp201758 Martinez-Rumayor, A., Richards, A. M., Burnett, J. C., & Januzzi Jr, J. L. (2008). Biology of the natriuretic peptides. The American journal of cardiology, 101(3), S3-S8. https://doi.org/10.1016/j.amjcard.2007.11.012 Murphy, S. P., Ibrahim, N. E., & Januzzi, J. L. (2020). Heart failure with reduced ejection fraction: a review. Jama, 324(5), 488-504. https://doi.org/10.1001/jama.2020.10262
Listen to the article here:
If someone in your family had a heart attack or stroke before the age of 60, you could be at risk and might want to have your blood tested for this little-known hereditary risk factor, Lp(a). Cardiovascular disease remains the leading cause of death in the United States, even during the COVID-19 pandemic. Determining and reducing the risk factors for cardiovascular disease is critical. Lipoprotein(a), also called Lp(a), pronounced “LP Little a” is a particularly dangerous culprit. Its levels are controlled by a single gene, and a single genetic variation in this gene is enough to drastically change Lp(a) levels. Unfortunately, since it is genetically determined, diet, exercise, and lifestyle have little or no effect on Lp(a) levels. High Lp(a) can contribute to several cardiovascular conditions. These include a two to three times increase in the risk of developing: Lp(a) has been referred to as the evil twin of the more familiar LDL (bad) cholesterol and is a triple threat because it is: There are two methods of measuring Lp(a). The most common method of measuring Lp(a) is by mass, in mg/dL. Measuring how many individual particles, regardless of size, is another method and is measured in nmol/L. It is important to know which method was used when understanding your numbers. If you have never had your Lp(a) level checked, we offer Lp(a) testing to our ENCORE community for those who pre-qualify (call for details). Currently, there are no approved therapies to lower Lp(a) levels and reduce one’s risk. However, three exciting therapies are currently being studied in clinical trials at ENCORE Research Group sites across Florida. The good news is that because of clinical research and your involvement, we have new treatments for elevated Lp(a) on the horizon! Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Sources: Kamstrup, P. R. (2021). Lipoprotein (a) and cardiovascular disease. Clinical chemistry, 67(1), 154-166. https://doi.org/10.1093/clinchem/hvaa247 Miksenas, H., Januzzi, J. L., & Natarajan, P. (2021). Lipoprotein (a) and cardiovascular diseases. JAMA, 326(4), 352-353. doi:10.1001/jama.2021.3632 Health.harvard.edu Amgenscience.com
Listen to the article here:
Fatty liver disease is incredibly prevalent in the United States. Some estimates place the number of Americans with non-alcoholic fatty liver at over 30%, that’s around 100 million people in this country! Liver diseases are deadly serious; the liver is a critical organ and without it we cannot survive. The biggest problem with all liver diseases is that they frequently progress without symptoms. Because of this, the disease may progress to a dangerous or irreversible stage before it is even detected. Clearly, early, and routine testing for people at risk is critical. We can’t see the liver from the outside, so the only way to learn about how it is doing is by looking at it. We can look through the skin using technology or under a microscope using a biopsy. A biopsy – looking at a section of the liver under the microscope – is the “gold standard” of liver diagnostic techniques. This has drawbacks, however. Patients typically need to dedicate half a day to the procedure, and there can be rare complications. A biopsy is an invasive procedure requiring a piece of the liver be taken and examined. It is a critical piece of the liver diagnosis pie but is not a routine procedure to be done without cause. Imagining techniques can be very effective in diagnosing a fatty liver. Some techniques, such as a CAT scan and ultrasound, can’t diagnose the amount of scarring on the liver but can give an indication that there is fat present. CAT scans use x-rays, but imaging is otherwise safe. An ultrasound is fast and non-invasive. It is an excellent first step that many doctors use when they suspect a fatty liver. Magnetic Resonance Imaging (MRI) is the next best diagnostic procedure to a liver biopsy. With an MRI, doctors can clearly see the state of the liver. They are expensive, however. This again means they are an excellent tool for those who are known to have fatty liver but may not be an option for all patients to use regularly. Ultrasonic elastography is a different technique. It is commonly called Fibroscan, after the manufacturer of the diagnostic tool. Fibroscan uses sound waves to gently shake the liver and measure how it responds. The liver will stretch slightly. In a healthy liver, the tissue stretches more, but hard scar tissue is less elastic. The fibroscan can interpret the difference and determine how much fat and scar tissue is present. The test is very similar to an ultrasound; it is painless, fast, and safe. The fibroscan does not replace other imaging techniques but is cheap and effective at determining the stage of fatty liver present. Unlike other techniques, a Fibroscan can be done routinely for anyone who is at risk of having fatty liver. Fibroscans are very popular around the world, including in Europe, Asia, South America, and Canada. It is a cheap procedure with little reimbursement for practitioners, which unfortunately prevents widespread use in the USA. Risk factors for non-alcoholic fatty liver include being overweight or obese, being prediabetic or having diabetes, and eating a high-fat diet. If you are concerned about fatty liver, talk to your primary care physician and/or contact ENCORE Research Group for a complimentary Fibroscan. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Afdhal, N. H. (2012). Fibroscan (transient elastography) for the measurement of liver fibrosis. Gastroenterology & hepatology, 8(9), 605. Koren, M. (Host). (2022, July 20). Common fibroscan technology questions [Audio podcast episode]. In Medevidence! Truth behind the data. ENCORE Research Group. https://encoredocs.com/medevidence/ Koren, M. (Host). (2022, July 13). You cannot live without your liver [Audio podcast episode]. In Medevidence! Truth behind the data. ENCORE Research Group. https://encoredocs.com/medevidence
Listen to the article here:
Metabolic syndrome is a cluster of conditions which have been slowly rising in people in the United States. It is also known as insulin resistance syndrome. It is currently defined as three of the following conditions: Having one of these conditions does not mean that you have metabolic syndrome. Having three or more of these conditions will result in a diagnosis of metabolic syndrome and will increase your risk of health complications. If left untreated, metabolic syndrome can lead to heart disease, Type 2 diabetes, and stroke. Metabolic syndrome is incredibly prevalent – affecting over one-third of Americans. Hispanic adults are at the highest risk. Among non-Hispanic adults, white men and black women are at higher risk than other groups. Other risk factors include lifestyle, age, family history, and use of some medications. Similar conditions may increase the chances of getting metabolic syndrome. These include being overweight or obese, immune system and sleep problems, and PCOS. Unfortunately, these risk factors overlap with the symptoms. This implies that metabolic syndrome may spiral and get worse over time. The exact mechanism of metabolic syndrome is unknown, but scientists have an idea of what is to blame. It may be insulin resistance, dysfunctional fat cells, inflammation, and oxidative stress. Insulin resistance causes the cells to store sugars instead of using them. This makes cells (and people) tired and increases fat. Fat cells may become overactive and grow so large that they die, prompting an immune response. The immune system may cause inflammation and plaque build ups in the bloodstream. Inflammation can further cause skin problems and long-term damage. While it sounds like this is all the fault of insulin resistance, it is not that clear cut. There may be many pathways into metabolic syndrome. Inflammation can be caused directly through a dysfunctional molecule responsible for fighting tumors. The liver has an important role in guiding the insulin response of the body. Obesity can cause oxidative stress that damages fat cells. Several other processes can interrupt these systems. Additionally, each symptom can increase the risk of developing others. So what can we do about metabolic syndrome? There are no approved medications to cure the underlying condition. For medical solutions, doctors may prescribe symptomatic treatments. These treat the parts of metabolic syndrome that we can diagnose: high triglycerides, cholesterol, and hypertension. Currently, our best way to fight metabolic syndrome is through diet and exercise. This may seem overwhelming to some people and making solid changes takes time. Instead of exercise, many need to think of movement. Movement can look like walking in the neighborhood, gardening, housecleaning, or anything that gets you moving, gets your heart rate up and is something you enjoy. Changes in other lifestyle choices may include consuming less sugar and sugary drinks, cutting out smoking and drinking, and getting regular sleep! Lack of appropriate sleep can increase your appetite for high-calorie foods due to hormonal changes. There are two hormones that make you hungry or full. Ghrelin is the hormone that increases your appetite and makes you crave food. Leptin is the hormone that makes you feel full with little appetite. These hormones can become unbalanced with lack of sleep, leading to negative changes in appetite. There is no silver bullet for everyone, but it’s a good start to take steps towards healthier lifestyle changes. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
References: McCracken, E., Monaghan, M., & Sreenivasan, S. (2018). Pathophysiology of the metabolic syndrome. Clinics in dermatology, 36(1), 14-20. https://doi.org/10.1016/j.clindermatol.2017.09.004 Moore, J. X., Chaudhary, N., & Akinyemiju, T. (2017). Peer reviewed: Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Preventing chronic disease, 14. Zimmet, P., Alberti, K. G. M. M., Stern, N., Bilu, C., El‐Osta, A., Einat, H., & Kronfeld‐Schor, N. (2019). The Circadian Syndrome: is the Metabolic Syndrome and much more!. Journal of internal medicine, 286(2), 181-191. https://onlinelibrary.wiley.com/doi/full/10.1111/joim.12924
Listen to the article here:
With flu season on the horizon, reviewing the vaccine pathway and how we got to where is worthwhile. We have an amazing and complex immune system. It has several specialized cells, but detection is the first line of an immune response. Detecting a harmful organism that has invaded the body can be surprisingly tricky. This is because cells have to chemically discover specific proteins or sugars on the outside of pathogens. These proteins or sugars can (and do) mutate in quickly-replicating pathogens. Luckily, our immune system can learn the danger of closely-related pathogens. Vaccines have a long and storied history. From the first records of vaccines in China hundreds of years ago to the first inoculation against smallpox (using cowpox) to today’s cutting-edge mRNA vaccines, the technology is constantly improving. Here are some of the major ways vaccines are made: The cowpox-smallpox vaccine was an example of a live, whole-pathogen vaccine. This is a type of vaccine where doctors inject small amounts of live viruses into the body. The body responds and becomes inoculated against large doses of the virus in the wild. In the 1950’s live-attenuated vaccines became available. In these, the virus is weakened in a lab so it does not cause serious disease in people. This type of vaccine provides a strong and long-lasting response. Examples of live attenuated vaccines include measles, mumps, and rubella vaccine (MMR), smallpox, chickenpox, and yellow fever. There are other methods to mitigate the problems of live viruses. An inactivated vaccine uses dead virus or bacteria. This makes the vaccine much safer and comes with fewer side effects, but is less effective. The current yearly flu vaccines are inactivated vaccines. Some manufacturers use hen’s eggs to grow the vaccine before inactivation. The resulting vaccine can contain very small amounts of egg protein as a result. The CDC still recommends those with egg allergies get the flu vaccine. Subunit vaccines are pieces of a pathogen – generally protein or sugar pieces. These aren’t whole viruses and have fewer side effects as a result. Additionally, these subunits may be able to grant protection against many forms of a pathogen. The Hepatitis B vaccine is an example of a protein subunit vaccine. Toxoid vaccines such as DPT can help lessen the damage of infection because some bacteria do their damage by releasing dangerous toxins instead of attacking cells. Toxoid vaccines train the body to recognize these toxins as dangerous. Diphtheria and tetanus vaccines are examples of toxoid vaccines. Nucleic acid vaccines are a new and different approach that has many benefits. Instead of using a weakened or inactivated pathogen to trigger our immune system, nucleic acid vaccines employ the body to make the vaccines in house. DNA, mRNA, and vector virus vaccines use genetic code created in a laboratory; there is no virus needed to develop the vaccine. Messenger RNA (mRNA) vaccines are the best known and use mRNA, a blueprint for creating specific proteins. When injected into the body, they provide the instructions for our body to produce antigens (proteins) that trigger an immune response. The T-cell and antibody response that follows can fight the disease. This can provide long-lasting, stable, relatively low symptom responses. The real benefit, however, is the time it takes to develop a new vaccine is drastically reduced. This was evident with COVID-19, when researchers created a brand-new vaccine in less than a year. Equally important was distributing it to hundreds of millions of people one year after. A typical vaccine takes 10-15 years to develop – and even longer to scale production. New studies are coming to compare the effectiveness of mRNA-based vaccines to inactivated vaccines for viruses and diseases beyond covid. Keep a lookout to join this new and developing vaccine research. Written by Benton Lowey-Ball, BS Behavioral Neuroscience
References: NIH, National Institute of Allergy and Infectious Diseases. (2021). Flu vaccine and people with egg allergies. https://www.cdc.gov/flu/prevent/egg-allergies.htm NIH, National Institute of Allergy and Infectious Diseases. (2019). Vaccine types. https://www.niaid.nih.gov/research/vaccine-types Greenwood, B. (2014). The contribution of vaccination to global health: past, present and future. Philosophical Transactions of the Royal Society B: Biological Sciences, 369(1645), 20130433. Boylston, A. (2012). The origins of inoculation. Journal of the Royal Society of Medicine, 105(7), 309-313.
Listen to the article here:
Use a weak virus
Use a dead pathogen
Use part of a virus or bacteria
Target a dangerous product
Get the body to do the work
Earlier this year, a bipartisan bill was introduced in the US congress to increase diversity in clinical research trials. The DEPICT act, as it’s called, has many major changes to how clinical trials would be conducted. These changes would affect sponsors, the government, and clinical research sites. Sponsors are the companies which develop new drugs and devices in clinical trials. The bill would require new demographic analyses for drug and device trials by sponsors. Demographic data includes age, sex, race, and ethnicity. Sponsors would investigate the rates of a disease among demographic groups before starting a trial. They would then devise a diversity action plan. This ensures the clinical trial includes a representative sample of the affected population. Let’s say a drug targeted lung cancer, for example. The sponsor would have to find out who has increased chances of getting lung cancer. If they found that Black Americans were at higher risk, they would make a plan to ensure this group was included in any research trials. Plans could include community outreach, specific site selection, and diversity training. A key aspect of the bill is discovering how to best reach diverse communities. Research sponsors would need to submit annual reports. These would outline how successful their studies were at reaching the demographic goals. If they failed to meet goals, they would give possible reasons they did not. The Food and Drug Administration (FDA) would compile and analyze the reports. The FDA would issue public reports on diversity and enrollment targets. They would also publish justifications for failure to meet targets and recommendations to solve this. Additionally, the National Institute of Health (NIH) would provide outreach. For sponsors, they would issue best practices for increasing diversity. They would engage with minorities to bring awareness of clinical research trials. They would also help local organizations inform their community about research trials. The final piece of the bill is increasing access. The bill would enhance clinical research infrastructure in underserved communities. The bill provides grants to expand clinical research facilities. These would be in rural areas, on Indian tribal lands, and in federally recognized underserved communities. The grants would help facilities conduct research trials in these areas. Altogether, this bill addresses the shortcomings of clinical trials in diverse communities. It closes the gap between who suffers from medical conditions and who participates in clinical research trials. It helps find out which methods increase clinical trial diversity. It also helps expand access to clinical trials in underserved communities. There is still a long way to go before this bill makes it to the voting floor, but it’s a good step. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Source: Text – H.R.6584 – 117th Congress (2021-2022): DEPICT Act. (2022, February 3). https://www.congress.gov/bill/117th-congress/house-bill/6584/text
Listen to the article here:
Hypertension is one of the most prevalent conditions on the planet. Scientists estimate that it affects 30-45% of adults, somewhere over a billion people! Hypertension is the chronic elevation of blood pressure. The CDC defines it as above 130 mmHg systolic or above 80 mmHg diastolic. For short periods of time, elevated blood pressure can be useful – for exercise, say. People can have high blood pressure for years without symptoms. For long periods of time, however, hypertension is deadly serious. Unfortunately, living with high blood pressure can lead to a host of problems. Hypertension can lead to heart attack and stroke, and damage to the heart, brain, kidneys, and even eyes! Everyone is at risk of high blood pressure. In America, men have a higher likelihood of hypertension. There are also differences in ethnicity and race, non-Hispanic Black or African American adults are at the highest risk. Unfortunately, even the lowest risk categories still have around a 40% prevalence of high blood pressure. Clearly this is a large issue in America and around the world. The big culprit behind hypertension is the Renin–angiotensin–aldosterone system (RAAS). RAAS is a critical system for maintaining blood pressure. It regulates two primary factors: the amount of blood and how constricted blood vessels are. It does this through the kidney, liver, and adrenal gland (just above the kidneys). In response to body signals, the kidneys release an enzyme to the liver. In response, the liver produces the hormone angiotensin I. Another enzyme, angiotensin-converting enzyme (ACE) converts this to angiotensin II, which goes to work. Angiotensin II has wide-ranging effects to increase sodium and water retention. It also causes blood vessels to constrict. Angiotensin II is very short-lived, only lasting 1-2 minutes. One of its many effects is to get the adrenal gland to produce aldosterone. Aldosterone has similar effects as angiotensin II, but instead of a few minutes, it takes hours or days to take effect. The end result is that two major hormones – one fast-acting and one slow-acting – cause high blood pressure. There are many medications available to fight hypertension. Most of these, such as diuretics or beta-blockers, have wide-ranging side effects. This is because they are system-wide, indiscriminate actors on the body. Beta-blockers, for instance, slow the heart. This is helpful in lowering blood pressure but obviously leads to other effects on the body. RAAS-acting specific medications may be more helpful in combating hypertension with minimal side effects. ACE inhibitors, for instance, stop the fast-acting angiotensin II from having its effect on the body. This targeted approach to hypertension can lead to fewer side effects in some patients. Unfortunately, by acting on only the fast-acting portion of RAAS, they must be taken daily. Even worse, a few missed doses can have longer-term effects on blood pressure. Luckily, researchers are investigating other targeted methods of reducing the effect of RAAS, and blood pressure! Keep an eye out for a clinical research study to help investigate this exciting part of the fight against hypertension. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Sources Fountain, J. H., & Lappin, S. L. (2017). Physiology, renin angiotensin system. National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. (September 27, 2027). Facts about hypertension. U.S. Department of Health and Human Services. https://www.cdc.gov/bloodpressure/facts.htm
Listen to the article here:
Celiac disease is one of the major health issues on our planet, affecting around 1% of the population (that’s about 80 million people!). Celiac disease is more likely to occur in females. Though onset can occur at any age, it is most likely to be discovered around age two or during young adulthood. Celiac disease is commonly known as gluten intolerance and is classically characterized by its gastrointestinal symptoms including diarrhea, loss of appetite, weight loss, and other digestive issues. Additionally, there are other symptoms that are unrelated to the digestive system. These include anemia, bone density issues, neurological symptoms, skin rash, and more. Together these make for a severe detriment in the quality of life of most celiac sufferers. Like most autoimmune disorders, the leading symptoms come from the body’s immune system overreacting and causing damage. Celiac disease is unusual in that the reason for the immune response is gluten, which we eat. Gluten is a structural protein found in wheat, rye, barley, spelt, and kamut. Gluten isn’t fully digestible, and some intact protein pieces make it through the stomach into the intestines. In celiac patients, the protein pieces cross the intestinal lining and are mistaken for dangerous particles or microorganisms. This can trick the immune system into action, causing inflammation and damage. The number of people with celiac disease has been growing significantly. Five times as many people had the condition in 2000, compared with 1975. Scientists are still unsure why the disease has been growing worldwide. Better clinical testing, a spread of high gluten Mediterranean diets, and new varieties of grain are leading theories. Scientists have been able to discover much of the underlying mechanism of how celiac disease occurs, thankfully. It is genetic, and the key player appears to be HLA-DQ2 or HLA-DQ8 antigens which mistake gluten for danger. The presence of HLA-DQ2/DQ8 isn’t enough to guarantee celiac disease, but it is required. Additional contributors are thought to be other genes, environmental factors, and gut microbiota. Regardless, 95% of celiac patients have one of these dangerous antigens. Currently, the only treatment for celiac is a strict gluten-free diet. This can be difficult to maintain, and even with a gluten-free diet, some patients continue to have symptoms. Additionally, contaminants can be unknowingly present in food and even low amounts of gluten can cause a resurgence of symptoms. Scientists are looking for new ways to combat this disease and participating in clinical trials is the best way that you can help move celiac disease medicine forward. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Source: Caio, G., Volta, U., Sapone, A., Leffler, D. A., De Giorgio, R., Catassi, C., & Fasano, A. (2019). Celiac disease: a comprehensive current review. BMC medicine, 17(1), 1-20.
Listen to the article here:
My buddy recently bought an e-bike on the internet. It has an enormous battery, goes pretty fast, and is salt air resistant – an important feature at the beach. It’s the perfect bike. Or at least it would be, except it is still on a dock in China, waiting for a cargo ship to deliver it. The bike is no good if it can’t get to where it needs to be. The same is true of drugs: a drug is only as good as its delivery system. Usually, the “buyer” of a drug is a cell somewhere in the body. Sometimes they are in specific areas, and sometimes they’re all over the place. Regardless, getting the drug to the target cells has always been a challenge. Our main delivery routes currently are swallowing, inhalation, skin absorption, and injection. Each has different uses, benefits, and drawbacks, but the route isn’t enough. Ingested medicines, for example, need to survive the harsh stomach acid but still be absorbable by the intestines. Injected medications are cleared by the liver at high speeds, reducing the effectiveness of a drug. Effective drug delivery means getting medicine to the right place at the right time, intact. One of the best-known developments in medications has been the use of mRNA in COVID vaccines. Actually getting the delicate molecules inside cells for an immune response was one of the unsung heroes of this vaccine. Scientists implemented lipid nanoparticles to get the job done. This was no easy challenge. Lipid nanoparticles are teeny packages of fat that protect the mRNA vaccine until it can get into target cells. They are small and strong to enter cells without disintegrating in the bloodstream. The development of lipid nanoparticles was just in time for the COVID pandemic and has shown to be very effective. The drawbacks are that they must be produced perfectly every time for billions of doses and must be kept extremely cold, at least currently. A much less widespread development has been the creation of microneedles. These are already in use for cosmeceutical applications. Microneedles are generally smaller than one or two millimeters and don’t puncture the skin all the way to the blood layer. This allows for simpler delivery and at-home administration of some medicines. Microneedles can also be coated with a dry version of medicines, allowing for shelf-stable drug delivery. This could be particularly helpful in areas with inadequate infrastructure and a lack of medical personnel. Researchers are developing many other new and exciting delivery methods. Targeted organ delivery is the practice of delivering medicine to specific organs. One example is coating a medicine in a urine-resistant coating for injection into the bladder. Cellular delivery uses living cells to carry medication to the target site. These living cells may be red blood cells or beneficial cyanobacteria. Attaching medicine to red blood cells can help drugs resist the powerful cleanup mechanism of the liver. This may allow for lower doses to have bigger effects. Attaching to beneficial spirulina platensis cyanobacteria may help medicines cross the stomach intact and deliver medicine straight to the intestines. This can allow for targeted organ delivery or for longer release of medicines. Finally, some scientists are experimenting with physically squeezing cells. This opens temporary pores for direct drug delivery. Such a system could enable scientists to deliver medicine to billions of cells per minute. All these exciting new delivery systems will have a big impact. Medicines of the future may be delivered in lower doses and with fewer side effects. We can also expect new uses for old medicines, as they will be able to be used in new ways and able to target new organs. Several of our clinical trials at Encore Research Group use these new methods. It’s an exciting time to help be on the cutting edge of what new medicine delivery will look like in the future. With luck, these new delivery methods will open new doors for medicines to help save lives and heal conditions. With even more luck, my buddy might get his bike by the end of the year. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Sources: May, M. (2022). Why drug delivery is the key to new medicines. Nature Medicine, 28(6), 1100-1102. National Institute of Health, National Institute of Biomedical Imaging and Bioengineering. (October, 2016). Drug delivery systems. U.S. Department of Health and Human Services. https://www.nibib.nih.gov/science-education/science-topics/drug-delivery-systems-getting-drugs-their-targets-controlled-manner
Listen to the article here:
Heart disease is the leading cause of death in the United States. Though there are several types of heart disease, one of the main ways the heart actually dies is through congestive heart failure, when the heart fails to pump effectively. Ineffective pumping causes blood and other fluids to build up throughout the body. Eventually, the fluid buildup may keep the heart from functioning at all, a condition called acute decompensated heart failure. This is an emergency condition, and without rapid medical treatment quickly leads to death. Fortunately, with early intervention, several patients can recover – at least temporarily. Clearly, one of the keys to saving people is early intervention. The vocal cords and lungs may be affected by congestive heart failure. As these fill with fluid, there are changes in how the voice sounds. These changes are difficult for people to hear, but technology might be able to help out. One type of technology looking to tackle the topic is a deep neural network called HearO. Deep neural networks are a subset of artificial intelligence. These systems learn how to make predictions from examples. The HearO system, made by the company Cardio Medical, analyzed the voices of people with congestive heart failure. The system learned by comparing people’s voices while they were “wet” (fluid-filled while in the hospital) and “dry” (after hospital treatment and discharge). Using this, the system learned to detect voice differences in the severity of the condition. The HearO system has now been packaged as a smartphone app. Patients talk into the app every day and it compares their voice to itself. It scans for changes that indicate a fluid build-up (and danger!). The hope is that HearO will help detect changes in the voice before acute decompensated heart failure occurs. Clinical trials are currently underway to test the HearO’s effectiveness and some of our ENCORE Research Group sites are enrolling for this. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Sources: Amir, O., Abraham, W. T., Azzam, Z. S., Berger, G., Anker, S. D., Pinney, S. P., … & Edelman, E. R. (2022). Remote speech analysis in the evaluation of hospitalized patients with acute decompensated heart failure. Heart Failure, 10(1), 41-49. Brooks, M. (2015, December 15). Smartphone app could give voice to congestion in heart failure. Medscape. https://www.cordio-med.com/wp-content/uploads/2021/12/smartphone-app-could-give-voice-to-congestionin-heart-failure.pdf Tomov, N. S., & Tomov, S. (2018). On deep neural networks for detecting heart disease. arXiv preprint arXiv:1808.07168.
We’ve all heard enough about COVID-19, but it’s worth remembering that other viruses still try to get cozy in our respiratory system. One virus that is very prevalent in the United States is Respiratory Syncytial (“sin-sish-ul”) Virus, or RSV for short. It’s so widespread that the CDC states that nearly all children will get RSV before their second birthday. The oldest (above 65) and youngest (under 5) populations are most at risk of complications. Those most in danger are premature children, those with compromised immune systems, and those with underlying heart or lung diseases. All told, RSV accounts for around 177,000 hospitalizations of seniors (65+) and 58,000 children (under 5) each year. RSV is easily transmissible. It passes from person to person through coughs, sneezes, or indirect means, like touching a doorknob and then your face. Most patients experience mild, cold-like symptoms. These include runny nose, fever, cough, sneezing, etc. Symptoms usually come in stages over a couple of weeks. Very young children and those at higher risk may experience more severe symptoms. In children under six, RSV might present as irritation, decreased activity, and breathing difficulty, which can be severe – and very scary! In adults over 65, severe symptoms can include a worsening of asthma or COPD, pneumonia, and the development of Congestive Heart Failure – a fluid buildup in the heart that prevents it from pumping effectively. Much like the flu, RSV is seasonal. In most of the United States, the season is from September to February. The Florida Department of Health notes that Florida has a longer season than the rest of the nation. Here, the season for RSV is from August through April. The CDC has found that all across the south the year-round RSV cases increased. 2021 saw an unexpected surge of RSV over the summer. This is in part because the same tactics used to stem COVID-19 also protect against RSV. These protective measures include wearing masks, washing hands and surfaces, and social distancing. As these restrictions were lessened, cases of RSV rose to unprecedented summer levels. Unfortunately, there is no cure for RSV. As it’s a virus, antibiotics are ineffective. Most patients will recover naturally. For others, best practices are treating symptoms by managing fever, pain, fluid intake, and any complications. For children and infants at severe risk, monthly Palivizumab injections may be available. Unfortunately, there are no publicly available vaccines for adults at increased risk. There are vaccines currently being researched that are going through clinical trials. With your help, we can find an effective RSV vaccine and help protect those at risk. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Sources: Centers for Disease Control and Prevention. (2019). Respiratory Syncytial Virus Infection (RSV). Atlanta, USA. Centers for Disease Control and Prevention. (2021). Increased interseasonal Respiratory Syncytial Virus (RSV) activity in parts of the southern United States. Atlanta, USA. Florida Department of Health. (2022). Respiratory Syncytial Virus (RSV) in Florida. Tallahassee, USA
Vision is our main way of interacting with the world, and it can be debilitating when our vision deteriorates. Unfortunately, presbyopia – the gradual loss of ability to focus on nearby objects – is basically inevitable. Presbyopia affects nearly 25% of the world population; almost 2 billion people. People usually see symptoms in their 40s, but the path starts in childhood. The exact cause of presbyopia is unknown, but the effects are well documented. The eye’s lens is the bit that changes shape, allowing us to focus at different distances. During childhood, the lens gradually becomes less flexible. Since it can’t change shape as easily, we stop being able to focus as rapidly and accurately. It gets more difficult to focus at close or mid-lengths. There are four broad methods suggested for increasing focal range, each with its own trade-off. Changing focus over time is the first method. Think of it like having several pairs of glasses. When focusing on close things you might use readers. Different glasses may be used for mid-length, or distance viewing. This is what our eyes do naturally (when we’re young at least!). So far there are no pharmaceutical or implantable devices that can accomplish this. Using several glasses is a good – if bulky – approximation for millions of people, however. Changing focus depending on where you look is the second method. Bifocals are the classic example. This solution is quick and convenient. There are downsides, however. Changing from near to mid-focus can be jarring, vision can be blurry, and eye strain occurs sometimes. One often overlooked issue is that bifocals can introduce other dangers, such as falls due to unfocused areas near the feet when walking. Changing focus between eyes is an interesting method. With this approach, one eye is corrected for close vision, and the other stays focused at a distance. Each eye only focuses narrowly, but together you can see across a wide range. Even though this is easy to try by putting in only one contact lens, it can be hard to get used to and lead to a loss of binocular vision. Judging distances of objects may be more difficult with this method, and it can be uncomfortable for some people. The final method is to increase the focal range across distances. This is an innovative method where the eyes are changed to have more in-focus at the same time. If you’ve ever had an eye exam where they dilate your pupils, this is the opposite. The pupils are artificially constricted. This extends your depth of field, making it easier to focus on things near and far at the same time! Some side effects may include a loss in quality and contrast, and a loss of low-light sensitivity. One of the big hurdles researchers have is the precision required to pull this off successfully. Methods to induce increasing focal range can be permanent, such as with implanted lenses; but mitigation of side effects may be easiest with special eye drops. Some of these eye drops are being tested currently in clinical trials. With so many different angles to attack presbyopia, and volunteers helping with clinical trials, we may be looking at a universal treatment soon! Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Source: Chang, D. H., & Waring, G. O. (2021). Presbyopia Treatments by Mechanism of Action: A New Classification System Based on a Review of the Literature. Clinical Ophthalmology (Auckland, NZ), 15, 3733.
Have you ever had a headache that you couldn’t shake, even for hours or days? One that may make you nauseous or unable to function? Then you may have had a migraine. And you’re not alone. A survey from 1990 to 2010 found that about 15% of the world’s population have migraines each year. That makes migraines the third-highest source of long-term injury! Women are around twice as likely to get migraines than men. Migraines can be broadly lumped into two categories based on frequency, episodic and chronic. People with episodic migraines experience between 0 and 14 days with migraines a month. More than that and the condition is called chronic migraine. The difference between these two categories isn’t set, and a small percentage of those with either condition may evolve or degrade into the other. Either way, migraines are debilitating. They last hours to days and may be accompanied by an aura: a visual indication of an impending bad day. The exact underlying causes of migraines are unknown, but there are some areas where intervention is possible. The pain and debilitating effects of migraines are caused, at least in part, by something called vasodilation. This is just a fancy term for when blood vessels expand, allowing more fluid to pass through. Vasodilation can occur for many reasons, but one of the main suspects in migraines is a protein called CGRP (calcitonin gene-related peptide, for the curious). This protein acts on the coverings of the brain, causing vasodilation that inflames this area. It is unclear exactly what happens after this, but the end result is debilitating pain. It has even been shown that injecting CGRP can cause a migraine to start. Interventions against this vasodilation are possible through a couple of different routes. One of the classic ways of tackling a migraine is through a medication called Dihydroergotamine, or DHE for short. This medication causes some arteries in the brain to constrict, counteracting the vasodilation from CGRP. This can “interrupt” the migraine and provide relief. This relief often effectively ends the migraine. DHE has been available for injection in the US for some time, though in other countries it is available as a nasal spray. Researchers are working to get approval for this method in the US as well. Another intervention being researched is stopping the vasodilation at the source. There is ongoing research in stopping CGRP from acting on the brain coverings at all. This is a new avenue that may help provide migraine relief with fewer side effects. Research in this field is also ongoing, ask us about the different ways you can help provide research insight into relief for this real headache of a condition. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Sources: De Matteis, E., Guglielmetti, M., Ornello, R., Spuntarelli, V., Martelletti, P., & Sacco, S. (2020). Targeting CGRP for migraine treatment: mechanisms, antibodies, small molecules, perspectives. Expert review of neurotherapeutics, 20(6), 627-641. Marmura, M. J. (2018). Triggers, protectors, and predictors in episodic migraine. Current pain and headache reports, 22(12), 1-9. Shafqat, R., Flores-Montanez, Y., Delbono, V., & Nahas, S. J. (2020). Updated evaluation of IV dihydroergotamine (DHE) for refractory migraine: patient selection and special considerations. Journal of Pain Research, 13, 859. Vos, T., Flaxman, A. D., Naghavi, M., Lozano, R., Michaud, C., Ezzati, M., … & Harrison, J. E. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet, 380(9859), 2163-2196.
Listen to the article here:
Ulcerative colitis (UC) is a chronic and progressive autoimmune disorder that causes inflammation and ulcers to develop in the intestines, which can be very uncomfortable or debilitating. Ulcers are breaks or holes in the protective lining that can cause bloody diarrhea, with or without mucus. One of the significant symptoms of UC is a high urgency of bowel movements. Other symptoms include abdominal pain, bowel inflammation, and constipation. UC is not a fun condition to experience, to say the least! It is usually experienced in cycles of remission and relapse with periods of terrible high and thankfully low (or no) symptoms. The high periods can even lead to hospitalization. UC can develop at any age but is more likely to develop in people 15 to 30 years old. Interestingly, there seems to be a lower chance of developing UC if your appendix has been removed or if you are a smoker. This disease doesn’t play favorites, so there is no difference between men and women developing UC. Racial differences may be minimal compared to differences in diet and lifestyle. For example, a diet that includes eating refined sugars and processed grains may increase the likelihood of developing the disease. As mentioned above, diet can be a risk factor; this may be because of an immune response to the food. Research continues to show that the food you eat can affect all parts of the body. People with genetic factors have an immune system that attacks non-harmful gut bacteria, and low gut microbiota diversity may also be a risk factor. Ulcerative colitis often presents with other diseases. Data suggests that there is a relationship between UC and rheumatoid arthritis. Some experts think joint pain and swelling may be part of the same immune response responsible for ulcerative colitis. Other comorbidities include acute hepatitis (liver inflammation) and occasional skin conditions. Treatments for UC aim at inducing a period of remission. All of them come with side effects, so your doctors, specialist and primary care, should all be informed about the medications that you are taking. A particularly unpleasant and severe treatment is a colectomy or bowel resection, which removes part of the affected colon. 20-30% of people with UC may have to undergo this procedure. The good news is that researchers continue to look for better ways to treat UC. With your help, we can make a difference! Visit our enrolling studies page to get involved in the latest clinical research. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Sources: Gajendran, M., Loganathan, P., Jimenez, G., Catinella, A. P., Ng, N., Umapathy, C., … & Hashash, J. G. (2019). A comprehensive review and update on ulcerative colitis. Disease-a-month, 65(12), 100851. Lee, S. H., eun Kwon, J., & Cho, M. L. (2018). Immunological pathogenesis of inflammatory bowel disease. Intestinal research, 16(1), 26. Attalla MG, Singh SB, Khalid R, Umair M, Epenge E. Relationship between Ulcerative Colitis and Rheumatoid Arthritis: A Review. Cureus. 2019;11(9):e5695. Published 2019 Sep 18. doi:10.7759/cureus.5695
The liver is a critical organ that has many functions. It balances the body’s energy budget, filters blood, and metabolizes drugs, for a start. Since the liver is so imperative, it goes without saying that when the liver starts to fail, a lot can go wrong. It is widely known that excessive alcohol consumption can damage the liver, but there are also other pathways to liver damage. One particularly dangerous pathway for liver disease is Non-Alcoholic Steatohepatitis or NASH which is the most severe form of non-alcoholic fatty liver disease. The exact cause of NASH is unknown. NASH is a disease characterized by an accumulation of fat in the liver coupled with liver enlargement due to chronic inflammation and cell death. It is difficult to diagnose NASH. The symptoms, tiredness and/or pain in the upper right side of the abdomen, are not very specific to NASH or helpful in diagnosis. Most often, patients do not have symptoms at all until the later stages of the disease. NASH is widespread, affecting between 3-5% percent of the worldwide population. It has been referred to as a modern lifestyle disease, with things like overeating and sedentariness contributing to it. There are several risk factors for developing NASH: NASH is a progressive liver disease, meaning it gets worse over time without treatment or lifestyle changes. The first step of NASH is fibrosis, where repeated scarring occurs. This scarring forms when the liver is repeatedly damaged and healed. NASH patients develop more severe forms of fibrosis about twice as fast as those with alcohol-induced liver damage. In NASH, unlike with alcoholic liver disease, the cause of damage is not always known. Fibrosis is scarring that is reversible with treatment. If NASH progresses further, cirrhosis may occur. This is scarring and liver failure that is permanent, though people can live with it for years. In cirrhosis, the cells of the liver themselves suffer damage. The final two stages of NASH are hepatocellular carcinoma, a type of liver cancer, and death. Tackling NASH early on is vital to those suffering from this disease! Unfortunately NASH is an understudied disease with few routes to recovery. Currently, the most effective treatment appears to be weight loss, accompanied by dietary and lifestyle changes. In scientific studies, this has been only achievable by about 50% of those with NASH. With this in mind, and only the early fibrosis stage of NASH being reversible, the search for medications that can treat NASH has been described as the “Quest for the Holy Grail.” There are currently no FDA-approved drugs to treat NASH. Several clinical trials exist and will continue to enroll and may lead to a treatment soon. If you have NASH, it’s important to consider participating in clinical trials to help find effective treatments. Find out which clinical trials are enrolling near you by visiting our enrolling studies page. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Sources: Povsic, M., Wong, O. Y., Perry, R., & Bottomley, J. (2019). A structured literature review of the epidemiology and disease burden of non-alcoholic steatohepatitis (NASH). Advances in therapy, 36(7), 1574-1594. Sharma, M., Premkumar, M., Kulkarni, A. V., Kumar, P., Reddy, D. N., & Rao, N. P. (2021). Drugs for non-alcoholic steatohepatitis (NASH): quest for the holy grail. Journal of Clinical and Translational Hepatology, 9(1), 40.
Listen to the article here:
Ahoy ye mateys! Have you ever wondered which enemy was the most dangerous to sailors during the 1700’s? James Lind, a Royal Navy surgeon, described a foe which “proved a more destructive enemy, and cut off more valuable lives, than the united efforts of the French and Spanish arms.” In order to conquer this threat, Lind employed a brand new weapon. This weapon was previously unknown to science, and has now been used to defeat countless foes. The enemy was scurvy, and the weapon was a clinical trial. May 20, 2022 marks the 275th anniversary of that first clinical trial. Scurvy could lead to muscle pain, gum disease, fatigue, jaundice, and death. Remedies at the time varied widely and only anecdotal, word-of-mouth evidence for them was available. Every sailor who was afflicted with scurvy sought a cure, but the overall disease was caught in the doldrums without a solution for 150 years. Lind had bigger ambitions. His big insight wasn’t trying to treat just a few individuals for scurvy, but instead trying to solve the problem of scurvy on the scale of public health. Though he only had 12 participants in that first trial, how Lind compared different remedies showed his big-picture thinking. He sought not to give relief to just those 12 patients, but to quantify and share his results to cure the whole of the Royal Navy. In this effort Lind laid the groundwork of the modern clinical research study. He started with a set of 12 patients with conditions “as similar as I could have them.” He controlled extraneous variables, giving all patients the same diet during the study and keeping them on the same boat. He split them into 6 random conditions: The results were clear; citrus gave quick and significant relief. Importantly, Lind didn’t leave his findings high and dry. He recorded and reported what he saw. Probably the most important aspect of Lind’s clinical trial was that he looked at the results in an unbiased way. He wrote extensively on the need to remove personal and societal bias: “it is no easy matter to root out old prejudices, or to overturn opinions which have acquired an establishment of time, custom, and great authorities; it became therefore requisite for this purpose, to exhibit a full and impartial view of what has hitherto been published on scurvy.” Today the same core ideas guide clinical trials, but there are many more safeguards for participants. A good clinical trial today is grounded in science, provides benefits to patients that should outweigh any risks, and treats patients with respect. Critically, clinical trials have informed consent; all participants join voluntarily and must have full knowledge of any risks before signing up. Trials also have oversight from Institutional Review Boards and have medical staff on site to help with any adverse reactions. Following Lind’s example, clinical trials also target specific conditions, have randomized patients, control conditions (as much as possible), and dutifully record and report their findings. Though his aim was to blow scurvy out of the water, Lind ended up making waves in how scientists solve medical problems in general. His quantitative, balanced approach gave the world a system to tackle medical problems. On this International Clinical Trials Day we can help keep up the bounty of Lind’s legacy by volunteering as a clinical research trial participant and send some diseases to Davy Jones’ Locker! Written by Benton Lowey-Ball, BS Behavioral Neuroscience
Lind, J. (1753). A treatise of the scurvy: in three parts, containing an inquiry into the nature, causes, and cure, of that disease, together with a critical and chronological view of what has been published on the subject. Bulletin of the World Health Organization: the International Journal of Public Health 2004; 82 (10): 793-796.From https://www.jameslindlibrary.org/lind-j-1753/
Listen to the article here:
Attention-deficit hyperactivity disorder (ADHD) is a disorder that is often diagnosed in childhood. When most people think of ADHD, they envision young children with an overabundance of hyperactivity and impulsiveness. However, there are three kinds of ADHD: hyperactive, inattentive, and combined presentation (inattentive and hyperactive). Researchers feel that inattentive ADHD is underdiagnosed because the symptoms present quite differently and are less noticeable. It is a chronic condition that causes attention difficulties, hyperactivity, mood swings, and impulsiveness.
In more recent years, it has come to light that ADHD might be associated with some memory loss. Other common reasons for memory loss include brain injuries, illnesses like Alzheimer’s or depression, effects of drugs and alcohol, and nutritional deficiencies. Other examples that can cause memory loss are age, stress, or lack of sleep.
Many people with ADHD go undiagnosed, especially if they have inattentive ADHD. Adults with ADHD do report memory loss, especially long-term memory. More recent studies have focused on why adults with ADHD have memory loss.
An article under the National Library of Medicine states that “it is well documented that adults with ADHD perform poorly on long-term memory tests. ”Their study concluded that adult ADHD reflects “a learning deficit induced at the stage of encoding.”
Researchers aren’t clear about ADHD and memory loss or whether having ADHD as an adult puts you at higher risk for developing dementia. Another study done in 2017 discussed the overlapping symptoms of ADHD and a type of dementia called mild cognitive impairment.
Continued research is essential to increase understanding of ADHD and the link between memory loss. ENCORE Research Group sites do not currently have any research studies for ADHD, but you can find some by searching clinicaltrials.gov. If you are experiencing memory loss, it’s vital to speak with your doctor about your symptoms. If you are over 50 and have memory loss, Jacksonville Center for Clinical Research offers a free memory screening assessment. You can contact us at (904)-730-0166.
Sources:
Skodzik T, Holling H, Pedersen A. Long-Term Memory Performance in Adult ADHD. J Atten Disord. 2017 Feb;21(4):267-283. doi: 10.1177/1087054713510561. Epub 2016 Jul 28. PMID: 24232170.
Callahan, B. L., Bierstone, D., Stuss, D. T., & Black, S. E. (2017). Adult ADHD: Risk Factor for Dementia or Phenotypic Mimic?. Frontiers in aging neuroscience, 9, 260. https://doi.org/10.3389/fnagi.2017.00260
Listen to the article here:
Could our guts affect how smart we are? A new study of over 14,000 women provides evidence. The study followed middle aged, 50-60 year old women over seven years from 2014 to 2018. It found that the longer a person used antibiotics, the greater the mental decline. At the high end, two months of antibiotic use was correlated with a mental decline equal to aging an extra 3-4 years.
This study does not imply causation. All participants self-reported their data, meaning they answered questionnaires. This does not allow scientists to see a direct cause-effect relationship. Other confounding effects may have been in play. One is that participants who used more antibiotics were more likely to have been sick. The scientists in charge of this study attempted to account for these differences. Study scientists adjusted for:
- Age and socioeconomic factors (education level, spousal education level)
- Lifestyle (smoking, alcohol use)
- General health (weight, physical activity, eating habits, multivitamin use)
- Mental health (depression, antidepressant use)
- Cardiovascular health (heart medication, blood pressure, cholesterol, history of heart attack)
- Other big health issues (stroke, diabetes, emphysema)
After this they still found that antibiotic use was the leading indicator of mental decline.
The link between the gut and the brain is an area of intense and active investigation. Information can travel back and forth between the gut and the brain along a special route called the gut-brain-axis. This takes advantage of a large nerve, the vagus nerve. The vagus nerve directly links the digestive tract and the brain. Animal studies show that altering the gut bacteria can alter a host of mental processes. In developing animals, reducing gut bacteria alters how their brains develop. Animal stress hormone levels also vary in response to changes in gut bacteria levels. Several of these changes reverse or decline when normal bacterial levels are restored. More experimental information could help solidify the link between the gut and the brain.
Mehta, R. S., Lochhead, P., Wang, Y., Ma, W., Nguyen, L. H., Kochar, B., … & Chan, A. T. (2022). Association of midlife antibiotic use with subsequent cognitive function in women. Plos one, 17(3), e0264649.
Sources:
Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of gastroenterology: quarterly publication of the Hellenic Society of Gastroenterology, 28(2), 203.
Heijtz, R. D., Wang, S., Anuar, F., Qian, Y., Björkholm, B., Samuelsson, A., … & Pettersson, S. (2011). Normal gut microbiota modulates brain development and behavior. Proceedings of the National Academy of Sciences, 108(7), 3047-3052.
The eye is a fragile and carefully balanced organ. At the very front of the eye is a fluid-filled chamber called the anterior chamber. This is located between the clear cornea at the front and the pupil, where light enters the rest of the eye. The fluid that fills this area is called the aqueous humor. The aqueous humor is critically important for cleaning and bringing nutrients to the lens. It is like a clear version of blood. Another key job the aqueous humor performs is maintaining eye pressure. The pressure in the eye needs to be maintained within a very specific range (12-22 mm Hg). Aqueous humor continuously flows through the front of the eye at a very slow rate (like blood, but slower). When the flow rate out of the eye gets disrupted, eye pressure increases. Doctors call high eye pressure ocular hypertension. The major characteristic is increased eye pressure without other symptoms. When eye pressure causes damage to the optic nerve, we call it glaucoma. Glaucoma can occur in two ways, closed angle or open angle. Closed angle is sudden and a medical emergency. Open angle makes up almost all cases of glaucoma and is gradual in onset. Typical symptoms of open angle glaucoma are vision problems in the middle of sight. These can include trouble with reading, seeing faces, walking, and driving. Both types will cause permanent blindness if untreated. Open angle glaucoma can happen to anyone, but is much more common with adults over 60 years old. Most cases are females, and black and Asian populations experience higher rates of the condition. There are several underlying reasons for open-angle glaucoma: vascular, anatomical, genetic, or immune. Because of this wide spread of causes, there are several risk factors: Several treatments are available for glaucoma. These include surgical and medication-based treatments, and surgically implanted medications. The goal of all treatments is to increase the flow of fluid out, decrease the amount of fluid coming in, or to decrease the volume of the anterior chamber. Medications are quite effective when taken properly. Unfortunately, fewer than one third of patients adhere to doctor recommendations for glaucoma eye drops after a year. This is in spite of the condition being progressive in nature and leading to blindness. Effective implanted medication delivery systems may provide better outcomes for patients. To get involved in the latest glaucoma research, contact our Nature Coast Crystal River office.
Sources: Allison, K., Patel, D., & Alabi, O. (2020). Epidemiology of glaucoma: the past, present, and predictions for the future. Cureus, 12(11). Li, F., Huang, W., & Zhang, X. (2018). Efficacy and safety of different regimens for primary open‐angle glaucoma or ocular hypertension: A systematic review and network meta‐analysis. Acta ophthalmologica, 96(3), e277-e284. Robin, A. L., & Muir, K. W. (2019). Medication adherence in patients with ocular hypertension or glaucoma. Expert Review of Ophthalmology, 14(4-5), 199-210.
Listen to the article here:
Chronic heartburn and acid reflux are symptoms of gastroesophageal reflux disease (GERD). This disease can result in the wearing away of the tube between the stomach and throat. When wearing away does not occur, a specific type of GERD occurs. This type is non-erosive reflux disease (NERD). The rates of GERD in the US are very large, affecting 1 in 5 people. Most of those cases are actually the NERD type. This works out to 14% of Americans experiencing NERD. It affects men and women at equal rates, and in the USA rates are constant across racial lines. Several factors can increase the chances of getting NERD. Your chances are increased with: NERD does not destroy the esophagus, but comes with its own host of issues. Heartburn and irritation of the food tube define NERD, and are uncomfortable on their own. It can also cause chest pain, vomiting, asthma, coughs, and sleeping problems. Furthermore, a major class of GERD-targeting drugs are less effective on the non-erosive form, NERD. These drugs are called proton-pump-inhibitors. Proton pump inhibitors are the most effective medications for treating GERD. Major name-brand proton-pump-inhibitors include Prilosec, Protonix, Nexium, Prevacid, and several others. The generic names are omeprazole, pantoprazole, esomeprazole, and others. All of these work by reducing the stomach’s ability to make stomach acid, lowering its ability to burn. As a result, GERD is both less painful and less destructive to the esophagus. Several people experiencing NERD are resistant to proton-pump-inhibitors. There are several possible reasons. In some patients, high concentrations of stomach acid isn’t the cause of their issues. In fact, only around half of NERD patients have abnormal acid levels, so lowering stomach acid may not be helpful as a treatment. These patients may have acid reflux even when acid levels are normal. They may also have a particularly sensitive esophagus. This could result in the feeling of heartburn even with lower acid levels. These patients need new treatments to help manage NERD. With luck, a clinical trial will pave the way to widespread adoption of an effective treatment soon!
Sources: Ang, D., How, C. H., & Ang, T. L. (2016). Persistent gastro-oesophageal reflux symptoms despite proton pump inhibitor therapy. Singapore medical journal, 57(10), 546. Dent, J., El-Serag, H. B., Wallander, M., & Johansson, S. (2005). Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut, 54(5), 710-717. Hershcovici, T., & Fass, R. (2010). Nonerosive reflux disease (NERD)-an update. Journal of neurogastroenterology and motility, 16(1), 8. ICRMD (2021, August 27). What is non-erosive reflux disease? ICRMD. Retrieved March 24, 2022, from https://icrmd.com/2021/08/27/what-is-non-erosive-reflux-disease/ Ribolsi, M., Cicala, M., Zentilin, P., Neri, M., Mauro, A., Efthymakis, K., … & Penagini, R. (2018). Prevalence and clinical characteristics of refractoriness to optimal proton pump inhibitor therapy in non‐erosive reflux disease. Alimentary Pharmacology & Therapeutics, 48(10), 1074-1081. Yamasaki, T., & Fass, R. (2017). Reflux hypersensitivity: a new functional esophageal disorder. Journal of Neurogastroenterology and Motility, 23(4), 495.
Listen to the article here:
Crohn’s disease is one of two types of irritable bowel disease. Unlike the more narrowly located Ulcerative Colitis, Crohn’s disease can be very widespread. Crohn’s disease is caused by inflammation of the bowel walls which can occur anywhere between the mouth and anus. This inflammation is frequently interspersed with healthy tissue. It affects the entire thickness of the bowel walls. Crohn’s is usually diagnosed by age 35 and affects 1.5 million people in the USA alone. Crohn’s disease is an autoimmune disorder. That means your body’s immune system is mistakenly attacking healthy cells. It is also a multifactorial disease. This means there are several possible underlying causes for it. Scientists know that the causes include genetic and environmental factors. Some risk factors are a low fiber diet, high carb diet, altered microbiome, and the use of NSAID medication. Lifestyle factors that influence Crohn’s include sleep, stress, exercise, and smoking. Unlike ulcerative colitis, smoking doubles a person’s chance of developing Crohn’s disease. Having such a large amount of possible causes makes Crohn’s disease very difficult to cure. So far researchers have only found ways to intermittently fix the symptoms of Crohn’s disease. Surgery has the best chance of providing long-term help however surgery comes with massive side effects. There are two classic drug-based solutions corticosteroids and immunomodulators. Corticosteroids reduce the body’s inflammatory response. Immunomodulators change how the immune system acts. The newest type of Crohn’s medication to market is biologics, which targets only specific parts of the immune system to keep effectiveness high and side effects low. Several of these are still in the research phase along with some brand new classes of oral drugs. To learn more about getting involved in Crohn’s disease research studies, visit our enrolling studies page or call your local ENCORE office today. Written by: Benton Lowey-Ball, B.S. Behavioral Neuroscience
Source Gajendran, M., Loganathan, P., Catinella, A. P., & Hashash, J. G. (2018). A comprehensive review and update on Crohn’s disease. Disease-a-month, 64(2), 20-57.
Listen to the article here:
Parkinson’s disease is a brain disease known for producing problems with muscle movement. These problems can include shaking tremors, muscle stiffness, and difficulty with balance and walking. The direct cause of these problems is a decrease in dopamine production. Dopamine is a chemical in the brain used to communicate information between nerves. It is also used to direct motor function. The motor coordination part of the brain, the basal ganglia, requires dopamine to function. Without dopamine, the basal ganglia cannot coordinate your muscles well. This means you cannot coordinate smooth, balanced, and nuanced movements. The stereotypical shaking in Parkinson’s patients is the result. It is akin to what would happen if the traffic lights in a city were not receiving enough power. Cars would still get through town, but traffic would be slow, backed up, jerky, and would only get worse. Parkinson’s is a progressive disease, meaning that it gets worse over time. It affects about 1% of those 65 and older and 3% of adults over 80. Additionally, it is expected that the number of people with Parkinson’s disease may increase by up to 30% by 2030. Though it can affect any older individual, it is more common in men. Genetic and environmental factors can increase the chance of getting Parkinson’s. These include being of European or South American descent, smoking, and exposure to pesticides. Surprisingly, there is also a link between Parkinson’s and your gut! Your gut has a direct link to the brain through the gut-brain axis via a special nerve called the vagus nerve. The vagus nerve travels from the brain and some important parts of the digestive system (stomach, large, and small intestine). This nerve communicates a lot of information. It is partially responsible for mood, hunger, energy, and helps coordinate immune responses. Though the brain is the thinking center of the body, it needs input from the body to make decisions. Interestingly, 90% of vagus nerve information flows from the gut to the brain! Therefore, disruptions in the gut can have massive effects on how your brain functions. This appears to be true with Parkinson’s disease. Research shows that misfolded proteins called alpha-synuclein may be able to travel through the vagus nerve. This may damage the part of the brain responsible for muscle control, called the basal ganglia. Research has found that disruptions of the gut can affect every system the vagus nerve touches. This might be one of the causes for some of Parkinson’s other effects, including non-motor disruptions. These can include rapid eye movement behavior disorder (RBD), mood disorders, cognitive problems like attention and learning, and even hallucinations. So far, there are no therapies that can reverse the effects of Parkinson’s Disease. Doctors prescribe l-DOPA to replicate dopamine production in the brain. This helps the basal ganglia coordinate movement to reduce the symptoms of Parkinson’s. Unfortunately, we cannot yet reverse the progressive nature of the disease. Fortunately, clinical trials are aiming to discover disease-modifying treatments!
Sources: Breit, S., Kupferberg, A., Rogler, G., & Hasler, G. (2018). Vagus nerve as modulator of the brain–gut axis in psychiatric and inflammatory disorders. Frontiers in psychiatry, 44. Kandel, E. R., Schwartz, J. H., Jessell, T. M., Siegelbaum, S., Hudspeth, A. J., & Mack, S. (Eds.). (2000). Principles of neural science (Vol. 4, pp. 1227-1246). New York: McGraw-hill. Kouli, A., Torsney, K. M., & Kuan, W. L. (2018). Parkinson’s disease: etiology, neuropathology, and pathogenesis. Exon Publications, 3-26. Lanciego, J. L., Luquin, N., & Obeso, J. A. (2012). Functional neuroanatomy of the basal ganglia. Cold Spring Harbor perspectives in medicine, 2(12), a009621. NIH, National Institute on Aging. (2017). Parkinson’s Disease. https://www.nia.nih.gov/health/parkinsons-disease Schwarz, P. B., & Peever, J. H. (2011).Dopamine triggers skeletal muscle tone by activating D1-like receptors on somatic motoneurons. Journal of neurophysiology, 106(3), 1299-1309. Shaik, L., Kashyap, R., Thotamgari, S. R., Singh, R., & Khanna, S. (2020). Gut-brain axis and its neuro-psychiatric effects: A narrative review. Cureus, 12(10).
Listen to the article here:
There are many good things about April. Spring is sprung, Easter egg hunts, and Earth Day. You may not have known, but April is also “Move More Month!” This April challenge is a great way to get into a good routine of getting up and moving! Exercise is such an excellent benefit for your health. Exercise has proven to help people sleep better, increase serotonin levels (happy hormone), and overall be healthier.
Some simple ways to get moving are going on walks, stretching, lifting small weights, riding a bike, and many more! It’s all about making small changes to get into a routine. Our ENCORE Research staff challenged themselves for April to get moving, even while at the office. Every hour we get up and move, doing a quick exercise. We find that setting a reminder alarm helps to keep us on track. We hope that you can follow along and get inspired to move more!
Here are some ideas to help get you started:
Easy:
- Walk in place
- Chair sits
- Countertop plank
- Countertop push-ups
- Step-ups
- Go for a walk
Medium:
- Chair squats (not fully sitting)
- Knees down Plank
- Knees down push-ups
- Hand slap step-up
- Go for a walk/run (alternating)
- Speed Clean (set a 5-minute timer)
Hard:
- Squats
- Planks
- Push-ups
- Stair (or bench) step-up
- Go for a run
Healthy eating and exercise can help with not only your waistline but also cardiometabolic health. Carrying around extra fat can negatively affect your whole body; some areas of concern include the liver, heart, and joints. Although many people can maintain a healthy diet and exercise routine to keep the weight off, some folks need extra help with medication.
The liver is the largest organ inside your body and is integral in filtering harmful substances from your blood. When too much fat builds up in your liver, this is called fatty liver disease. This can progress to damaging and scarring of the liver. The scaring can ultimately lead to liver failure. Lifestyle changes, like healthy eating and exercise, are currently the only treatments for fatty liver disease, although many clinical trials are currently looking for a safe and effective therapy.
Heart disease remains the world’s leading killer. While extra fat itself does not directly cause heart attacks, it leads to other causes that can. High cholesterol, high blood pressure, and diabetes are among those that build up plaque in the arteries leading to heart attacks. ENCORE Research Group offices have many clinical trials in these areas!
Being overweight can affect your joints by raising your risk of developing osteoarthritis. The extra weight puts additional stress on your weight-bearing joints, such as your knees, which can cause additional wear and tear. Additionally, inflammation associated with weight gain might contribute to problems in other joints such as the hands.
For the folks who need more than just a healthy diet and exercise to help with medical conditions, the good news is that many new cutting-edge treatments are being studied and are available to you. Call your local ENCORE Research Group office today to get involved in our research trials.
Sources:
heathline.com
health.clevelandclinic.org
health.harvard.edu
Diabetic peripheral neuropathy is a type of nerve damage associated with diabetes that most commonly affects the peripheries of the body (toes, feet, legs, hands, and arms). Symptoms can range from mild to severe and can be painful, debilitating, or even fatal. The most common neuropathy symptom people seek medical attention for is pain. Since diabetic neuropathy currently does not have a cure, the best thing people can do is treat the pain and make sure their blood sugar levels are well controlled.
Diabetic neuropathy symptoms are often worse at night. Symptoms include:
- Lack of sensation to pain or temperature in those areas
- A tingling, burning or needle pricking feeling
- Sharp pain or cramps
- Extreme sensitivity to touch
- Problems with balance and coordination
People who have had diabetes for at least 25 years have the highest rates of nerve damage. Neuropathies are also more common in people who cannot keep their blood sugar under control, have high blood pressure, or are obese.
Current treatment options for pain are limited by poor effectiveness and high rates of side effects, leaving many patients without adequate pain control. With chronic use, nonsteroidal anti-inflammatory drugs (NSAIDs) pose a potentially serious gastrointestinal and liver toxicity risk. Opioids are commonly prescribed for moderate-to-severe pain but are limited by safety and tolerability issues and have high abuse rates. Opioid-associated death rates have also increased over the past two decades.
Given the limited treatment options, combined with the risks and ineffectiveness of currently available treatments, developing new treatments is vital for better pain management and health outcomes. We are involved in many cutting-edge research trials at ENCORE Research Group, and some of our locations currently have research studies for painful diabetic peripheral neuropathy. To learn more about participating in our cutting-edge clinical trials, call our main office today! (904)-730-0166
What is EoE? What are the symptoms? How to get diagnosed. Current research on EoE.
Eosinophilic esophagitis (EoE) is a chronic disease of the esophagus. Your esophagus is a muscular tube that carries food from your mouth to your stomach. EoE is when white blood cells (called eosinophils) build up in your esophagus.
Some of the most common symptoms of EoE are:
Your doctor will most likely want you to have an endoscopy to diagnose EoE. An endoscopy is a procedure where an endoscope (a tube with a light and camera attached at the end) is inserted into the body to let your doctor look inside an organ. For an esophageal endoscopy, the endoscope is put in your mouth and down your throat to examine the esophagus. But don’t worry, you’re not awake for that part! Other ways you can be diagnosed are biopsies, blood tests, and an esophageal sponge.
Science continues to move forward for new treatments of eosinophilic esophagitis, and we are delighted to be involved in these cutting-edge research trials at some of our ENCORE Research Group locations. To learn more about participating in our cutting-edge clinical trials, call our main office today! (904)-730-0166
Alzheimer’s is a devastating disease that affects 5.5 million people of all ages in the United States. Along with the diagnosis and reality of living with this disease, the families of these patients are now left with the question, “how will we take care of our loved one?” For many families, the option is having a designated person take care of the patient on their own. A caregiver is someone that assists with the daily needs of another person. There can be a “formal” caregiver, considered a paid person along with training, and an “informal” caregiver is a family or friend who provides care without pay. It can be a challenge for informal caregivers, especially with no training. Around 65.7 million people in the United States are informal caregivers. With that large of a statistic affecting a specific population, there are always great tips that can be provided.
Asking For Help
Taking care of someone with Alzheimer’s can be challenging. If it becomes too difficult for a caregiver, sometimes they feel guilty in asking for help. If taking care of someone becomes too emotionally and physically draining, there’s no shame in asking for help or even hiring someone to come in and help. The most important thing is making sure that your loved ones can get the best care they can get.
Staying Connected
Studies show that caregivers who stay in touch with their families and friends have better emotional health than those who feel isolated. Reaching out to express your feelings about being a caregiver and the challenges that come with it can help relieve stress. Staying in contact with other family members and keeping them updated on their loved ones allows them to step in and support when needed.
Making Your Health A Priority
Caregivers, along with the patient, must make sure their health is a priority. Without the caregiver in good health, they wouldn’t be able to provide the optimum care the patient needs. Along with regular check-ups, making sure you get yearly Flu shots, testing, and staying active is important. Being a caregiver can be physically demanding, and your health is just as important as the Alzheimer’s patient’s health.
Participate in Research for Alzheimer’s
There is currently no cure for Alzheimer’s, but there are clinical studies that the patient and caregiver can participate in. Since the caregiver needs to assist the patient with all that comes with being in a study, both the caregiver and the patient would receive a stipend. The more participants in Alzheimer’s studies, the more research is done, getting us closer to a cure! For more information on our currently enrolling Alzheimer’s disease studies, give our office a call.
How Do You Know If You Have High Blood Pressure?
The truth is, you don’t. The only way to really know if you have high blood pressure is by getting your blood pressure checked regularly. High blood pressure or hypertension (HTN) is known as the “silent killer” because it causes sudden heart attacks or strokes resulting in serious injury or possibly death with no warning.
The Effects of Hypertension
HTN causes more than just heart attacks and strokes. Prolonged HTN can cause serious illnesses such as:
- Kidney Disease — HTN may cause damage to the arteries surrounding the kidney. The damage can affect the kidney’s ability to filter blood efficiently.
- Heart failure — Heart failure occurs when the heart has to work harder to supply blood to the body, and HTN can cause extra work for the heart.
- Loss of Vision — HTN can strain or damage blood vessels in the eyes.
- Sexual Dysfunction — HTN can lead to erectile dysfunction in men or lower libido in women.
- Angina — Over time, HTN can lead to heart disease or microvascular disease (MVD). Angina, or chest pain, is a common symptom.
- Peripheral artery disease (PAD) — Atherosclerosis caused by high blood pressure can cause a narrowing of arteries in the legs, arms, stomach, and head, causing pain or fatigue.
How to Prevent a Visit from the “Silent Killer.”
One way to decrease your risk of heart disease from HTN is to know your numbers. Below is a chart from the American Heart Association that accurately details healthy vs. unhealthy blood pressure numbers.
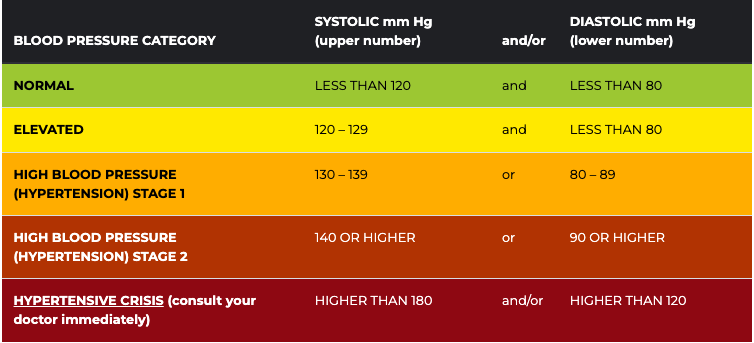
The second way is to be aware of your risk.
There are many risk factors for HTN and being aware of them can give you the knowledge to make healthy changes.
- Diet — Diet plays a considerable role in elevated blood pressure levels. Diets high in salty, fatty, and processed food increase your blood pressure, causing HTN. A good diet would be one that is high in vegetables, fruits, and lean meats.
- Physical Activity — Regular physical activity improves blood circulation and decreases your risk for HTN.
- Alcohol and tobacco use — Excessive alcohol and tobacco use can cause HTN and increase your risk of heart attack, stroke, and heart disease.
Other risk factors that you need to be aware of but are out of your control are:
- Family history
- Age
- Gender
- Race
Overcome Hypertension
How can you overcome hypertension? One way is to talk with your doctor about any medications or specific lifestyle changes you can make to reduce your risk. Another way is to participate in clinical trials. Clinical trials are a great tool to get to know your health more, receive one-on-one quality attention from a medical professional, and access to the latest therapies that are not currently on the market. ENCORE Research Group is currently enrolling in studies for hypertension. If you or someone you know would like to participate, please call 904-730-0166 or visit encoredocs.com.
In 2020 heart disease killed twice as many people as COVID-19 in the United States.1 Some may find this surprising due to the lack of news coverage on heart disease. Historically heart disease has always been one of America’s most serious epidemics. It has been a leading cause of death since the turn of the 20th Century. Following World War II, the National Heart, Lung and Blood Institute began a long-term study known as the Framingham study to identify the cause of heart disease. The Framingham study is an enormous observational study in Framingham, Massachusetts. Researchers conducted physical examinations on participants every two years to study contributing factors to heart disease and are now on their 3rd generation of participants. The Framingham study identified many currently known risk factors, such as high blood pressure and high cholesterol. Researchers began developing medications to combat cholesterol levels once high cholesterol was identified as a significant risk factor. Some of our most exciting research at ENCORE Research Group is for new cholesterol-lowering medications such as Antisense Oligonucleotides (ASOs), Small Interfering RNA (siRNAs), and Adnectins. Antisense oligonucleotides (ASOs) are short, synthetic single-stranded fragments of RNA that can reduce, restore, or modify protein expression. ASOs have been designed specifically to target high levels of LDL (bad cholesterol) in the bloodstream in a different way than current medications. They are also being studied to reduce lipoprotein a [Lp (a) or “Lp little a”] in patients with elevated levels by targeting a building block of the Lp(a). Small interfering RNA (siRNAs) are another type of RNA therapy that is being used in clinical trials to reduce the risks of cardiovascular disease. Unlike ASOs which are single-stranded oligodeoxynucleotides, siRNAs are double-stranded RNA molecules. SiRNAs are used in the silencing of disease-causing genes for the treatment of atherosclerotic cardiovascular diseases. Adnectins are a class of drugs used to target proteins. Adnectins can be rapidly developed to bind proteins or other necessary targets. Currently, adnectins are being used in clinical trials to bind with a human protein called PCSK9. This binding blocks the interactions between PCSK9 and LDL (bad cholesterol) receptors. As a result, the levels of LDL cholesterol in the body are lowered. We are optimistic about these new technologies; they may give us the arsenal to fight back against heart disease. If you have high cholesterol levels that are not being adequately managed by your current medications, we may be able to help you get involved in a research study that may help get you back on track! As many of our readers know, most research studies offer access to cutting-edge therapies at no cost to patients. Call us to find out how you can get involved today! [1] CDC, https://www.cdc.gov/nchs/products/databriefs/db427.htm
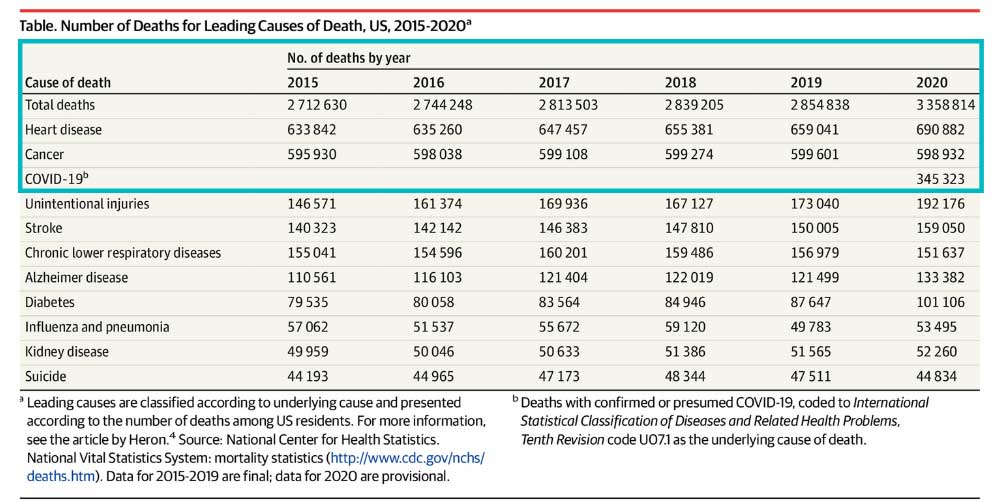
Lipoprotein (a), or Lp(a), pronounced “LP little a”
Lp(a) has been referred to as the evil twin of the more familiar LDL (bad) cholesterol.
It consists of an LDL-like particle with an extra protein coil that makes the particle more sticky to burrow into and damage the arterial wall.
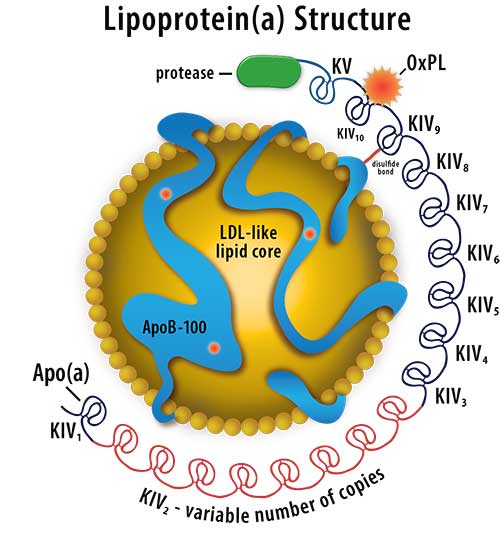
Lp(a) is a triple threat because it is:
- Pro-atherogenic causing a higher risk of producing plaque in arteries
- Pro-thrombotic meaning it promotes the formation of blood clots causing heart attacks and strokes
- Pro-inflammatory – inflammation can irritate your blood vessels, promote the growth of plaque, loosen plaque in your arteries, and trigger blood clots1
Lp(a) is determined by your genes. Exercise and dietary lifestyle changes have no effect on your level of Lp(a) but do contribute to your over health.
If you have experienced a heart attack or stroke before turning 60 years old, or have a family member who did, you could be at risk for elevated Lp(a).
As an ENCORE community perk, we can perform a complimentary blood draw to check your level of Lp(a).
To see a list of cutting-edge treatments for elevated Lp(a) currently enrolling in clinical trials, click the link below:
https://thefhfoundation.org/on-the-horizon-treatments-for-lipoproteina
If you are interested in participating in a clinical trial for elevated Lp(a), give our recruiting office a call today! (904) 730-0166
Daily habits can be hard to break, and if your daily habit is smoking, it can feel nearly impossible! However, when you understand the addictive nature of tobacco, it’s easier to understand why many just can’t quit. In fact, within the last couple of years, 50% of smokers attempted to quit, but only about 8% were successful.
Smoking cessation becomes easier if you have a plan in place. Below is a comprehensive list that will aid in your journey to a healthier lifestyle without tobacco. So let’s quit smoking together!
The Plan
1. List your Reasons for Stopping
Stay motivated by writing down a list of reasons you want to stop smoking. Frequently referring back to this list will keep you aware of why you are doing what you are doing when times get hard.
Reasons can include:
- Reducing your risk of heart disease. The risk of heart attack or stroke is decreased by 50% after two years of not smoking. After 15 years, your risk of heart attack is similar to that of a person who never smoked
- Saving money! Smokers can save between $1,380 and $2,540 annually (depending on where they live) by quitting a pack-a-day habit.
- Keeping friends and family away from second-hand smoke. Secondhand smoke causes nearly 34,000 premature deaths from heart disease each year in the United States among nonsmokers.
2. Pick a Quit Day
You control your destiny, so it is your responsibility to pick a quit day. If your quit day is too far out, you may find it hard to keep that motivation. But, on the other hand, you need to give yourself time to prepare.
Many believe it is best to wean off smoking, but studies have shown that the best results come from picking a day and quitting cold turkey.
3. Prepare for Your Quit Day
Research has shown that the best results come from counseling and medication for quitting smoking. These things take planning. Here is a list that may help you with that:
- Talk to your doctor about medications. Some treatments can lessen your craving. It is essential to talk to your doctor and begin one on your quit day. There are also clinical trials where you can receive medications for free with no health insurance needed.
- Find a support program. You can also talk to your doctor about support programs. There are many in-person or over-the-phone programs where you can speak with others about your journey.
- Find helpful online tools and apps. Online tools for creating and implementing a quit plan are available from the National Cancer Institute (https://smokefree.gov/build-your-quit-plan) and the Truth Initiative (www.becomeanex.org/). These websites and apps can increase smoking cessation success.
Other tips include:
- Making a list of triggers
- Telling your friends and family, you are quitting
- Cleaning your house of triggers
- Getting your teeth professionally cleaned
4. Make your Quit Day Easier
Your quit day is approaching quickly; let’s prepare a set of rules to follow.
- Don’t smoke, not even once
- Be sure you know how to use your nicotine replacement therapy if you’ve chosen that method.
- Read your “Reasons for Stopping” list
- Drink plenty of water
- Go for daily walks to stay active
- Avoid stressful situations
- Attend a class or call into a therapy/group session
EXTRA TIP: Find Clinical Trials near You
There are many reasons to join a clinical trial. First, it is free to join, you do not need insurance, and you may receive a stipend for time and travel. You will also get attentive care from a medical professional with frequent checkups to motivate you to stay on task. Lastly, you will feel good knowing you are improving your health and the health of future generations. For more information on clinical trials for smoking cessation, visit encoredocs.com or call 904-730-1066.
Alzheimer’s Disease is devastating. An estimated 6.2 million Americans age 65 and older are living with Alzheimer’s dementia in 2021. Alzheimer’s is a brain disease that causes a slow memory decline. It can also affect your thinking, problem-solving, and reasoning skills. There are ten signs that you or a loved one may be experiencing early stages of Alzheimer’s Disease. If any of these signs persist, you should schedule an appointment with your doctor and come in for a free memory screening at Jacksonville Center for Clinical Research (JCCR). A critical factor in spotting Alzheimer’s Disease’s early stages is noticing the memory loss of recently learned information. The memory loss examples include forgetting dates and events and asking the same questions multiple times. It can be difficult for a person in the early stages of Alzheimer’s to complete daily tasks. For example, they may find it difficult to find familiar locations or do simple things such as making a grocery list or remembering the rules to a favorite game. It can sometimes become difficult for those with Alzheimer’s to work with numbers. Tasks such as paying bills may get swept under the rug or have excessive errors. They also have difficulty planning things as simple as everyday errands. Alzheimer’s Disease can cause confusion and result in anxiety or panic. Frequently, they can forget where they are or how they got there. Alzheimer’s Disease and vision issues can go hand-in-hand. For example, they may show difficulty reading, balancing, or distinguishing the depth and color of objects. It can be difficult for someone with Alzheimer’s to join a conversation. They may stumble on their words. They may have trouble remembering names and often repeat themselves. Everyone loses their keys, remote, or wallet every once in a while. However, someone suffering from the early stages of Alzheimer’s may often lose these things or put them in strange places. For example, they are putting their keys in the fridge. Someone who has Alzheimer’s Disease may have poor judgment. Examples of this can be poor hygiene, trouble dealing with money, or acting irrationally. It can become difficult for people with Alzheimer’s to work or interact socially. You may notice them pulling away from normal social activities. They may start to have trouble keeping up with their favorite activity. Suffering from Alzheimer’s Disease can be extremely frustrating. It is common to experience sudden mood changes and sometimes act irrationally. They can quickly become confused, suspicious, depressed, or even fearful. It is important to remember that we can have a natural decline in cognitive ability as we age. However, when that decline disrupts daily life, it is time to see a doctor for a memory screening. Thankfully, there have been many breakthroughs in memory research, although there is still no cure for Alzheimer’s. Clinical trial studies are the only way to continue to learn about this disease in hopes of and finding a cure. If you or a loved one is currently experiencing any of these early symptoms of Alzheimer’s Disease, we encourage you to get a memory screening. ENCORE Research Group offers free memory screenings at our Jacksonville Center for Clinical Research location and has several studies enrolling for Alzheimer’s Disease. For more information, visit encoredocs.com or call 904-730-0166.
1.Memory Loss that Disrupts Daily Life
2. Difficulty Completing Normal, Daily Tasks
3. Trouble with Planning or Problem Solving
4. Confused about the Current Time or Place
5. Trouble with Vision and Depth Perception
6. Difficulty Pronouncing Words or Writing
7. Losing Important Items Often
8. Poor Judgement
9. Becoming Socially Distant
10. Mood Swings
The Hawthorne Effect is an interesting phenomenon where people alter their behavior due to the awareness of being observed. This effect was first discovered in the 1950s outside of Chicago. The experiment was done on factory workers, and it found that workers had a positive response to the extra attention given by managers who cared about them. This same phenomenon has been noticed in clinical trials as well. “When you’re doing a clinical trial, and you’re involved with something that is being observed, your patients tend to do better regardless of how they are being medically treated.” Dr. Michael Koren, CEO of ENCORE Research Group, says. For example, if a patient is in a clinical trial for weight management, they may be more likely to lose weight if they must keep a log of everything they eat and present it to their study coordinator. So what does that mean for you? It means that you have the chance to improve your health just by participating in a clinical trial, even if you happen to be on a placebo. Studies have shown that patients in clinical studies are more adamant and knowledgeable about their health in the first place. It is safe to say your health will likely improve no matter what study you participate in! To see what studies are available right now, visit our enrolling studies page!
*This assessment is only available at Jacksonville Center for Clinical Research* What is a Memory Assessment? A memory assessment tests for cognitive impairment. The assessment is a 30-point test widely used to assess dementia and Alzheimers. The type of test we use is the MMSE or mini-mental state exam. The MMSE assessment is a crucial step toward making a diagnosis. Who Should Be Tested? Memory loss can be a sign of aging. However, there are differences between typical signs of aging and memory loss, leading to dementia and other diseases. If you can still work or live independently, likely, you are just showing signs of age-related memory loss. On the other hand, if your memory loss disrupts your life, it is time for a memory assessment. Other signs to look out for include: How Our Free Memory Assessment Works If you are unsure or worried about yourself or a loved one, you can get an MMSE free of charge for ages 50 and up at our Jacksonville Center for Clinical Research location. If you decide to schedule an appointment, plan to be at our facility for about an hour and a half. During that time, one of our experienced clinical coordinators will ask you a series of specific questions about your memory. The MMSE assesses orientation to time, orientation to place, word recall, calculations, naming, repetition, comprehension, reading, writing, and drawing. At your appointment, your clinical coordinator will also have you go through a memory questionnaire, asking about your daily symptoms. Afterward, your results will be given to you, and there will be a clinical investigator on-site to answer any questions you may have. As mentioned, there is no cure for memory-loss-associated diseases, but the strides science has made in recent years have been astounding thanks to clinical trials. If you or a loved one is experiencing severe memory loss, you may consider a clinical trial. There are many benefits to participating, including one-on-one personal care from a physician and access to the latest experimental medication. Jacksonville Center for Clinical Research, a member of ENCORE Research Group, is enrolling in memory loss and Alzheimer’s disease research studies. If you want to learn more or schedule an appointment, call 904-730-0166.
If you are experiencing memory loss, you are not alone. According to the National Institutes of Health, roughly 40% of the population 65 and older experience associated memory impairment. Dementia is the broad category of cognitive impairment with subtypes like Alzheimer’s disease, Lewy Bodies, Vascular Dementia, and others. Although there have been many breakthroughs in memory research, there is still no cure for memory loss.
Psoriasis is a skin disease that can cause red, itchy patches on the skin. These patches are commonly found on the knees, elbows, and scalp. Psoriasis is an autoimmune disease, meaning it results from the body attacking itself. The red, scaly patches come from the body releasing white blood cells to attack a non-existent infection. This mistaken attack causes the skin cell process to multiply rapidly. As a result, the skin cells are pushed up to the skin’s surface, where they pile up. These extra skin cells create red, scaly, and inflamed areas at the skin surface. For many, these symptoms tend to go through cycles, flaring for a few weeks or months then subsiding. Although unclear as to the exact cause, decades of research have concluded that genetics and the immune system are two major risk factors for psoriasis.
It’s becoming more apparent that psoriasis affects more than just a person’s skin. In fact, recent studies have linked psoriasis to high cholesterol, heart attack, and stroke. One study notes a significant reduction in HDL, the good cholesterol, in psoriatic patients as well inhibited ability for the remaining HDL to do its job correctly. When this happens, the severity of psoriasis coverage increases.3 Another study, conducted by Northwestern Medicine and published in the Journal of Clinical Investigation, found that a specific category of immune cells called self-lipid reactive T-cells represent a yet to be determined link between high cholesterol and the symptoms of psoriasis. So one has to pose the question, will treating high cholesterol have a positive effect on the severity of psoriasis or vice versa? Science is moving forward in the realm of psoriasis and we are fortunate to be involved in the process. If you are suffering from psoriasis, you can help change medicine by participating in research. ENCORE Research Group patients enjoy; access to the latest medicines and therapies at no cost and one-on-one, attentive care from a medical professional. You can move medicine forward and create better healthcare for future generations by participating in clinical trials. New research studies are always coming in, so head on over to the enrolling studies tab to see what study you are interested in volunteering for. Source: plaquepsoriasis.com, American Journal of Managed Care, Northwestern Medicine https://www.ajmc.com/view/psoriasis-linked-to-high-cholesterol-levels-study-finds
Does Psoriasis Affect More Than Just Your Skin?
Novo Nordisk’s Wegovy (semaglutide) for weight loss
Biogen’s Aduhelm (aducanumab) for Alzheimer’s Disease
Pfizer’s PREVNAR 20 (pneumococcal 20-valent conjugate vaccine) for the prevention of pneumonia
https://www.nejm.org/doi/full/10.1056/nejmoa2102214 Novavax vaccine – Among a subgroup of HIV-negative participants, the vaccine was 60.1% efficacy against the B.1.351 South African variant. https://www.nejm.org/doi/full/10.1056/NEJMoa2103055
You may have heard that people with diabetes are at a higher risk of contracting COVID-19. This is not the case. The truth is, people with diabetes are more likely to experience severe illness, long lasting effects, or even death if they are infected with COVID-19. What We Know about Diabetes and COVID-19 In May, a nationwide multicentre observational study called the CORONADO study, observed the mortality risk in people with diabetes who were hospitalized for COVID-19. The study population was 88% type 2 diabetics and 12% type 1 diabetics. What they found was that one in ten diabetic patients hospitalized with COVID-19 died within seven days of hospital admission. One in five died within the first 28 days. How Can We Improve These Numbers?
5 Things to Know about Lp(a) Lipoprotein(a), or Lp(a), is an independent risk factor for atherosclerotic cardiovascular disease. Cardiovascular disease is the leading cause of death in both men and women in the US and globally . You may have heard of LDL cholesterol, or “bad cholesterol,” as a risk factor for heart disease, but Lp(a) can be just as dangerous. Lp(a) flies under the radar of many physicians. This is because the awareness of Lp(a) is still very low, very little is understood about the protein and the treatment options are limited. What is LP(a)? Lp(a), pronounced “LP little a,” is a protein that is attached to LDL cholesterol. It is composed of an LDL-like particle, but it has a second protein coiled around it. Recent studies have shown that people born with elevated Lp(a) can be two to four times as likely to have a heart attack or serious cardiac related risk. Lp(a) is present in 20% of the population. What differentiates LP(a) from other heart disease risk factors? LP(a) is so unique because it is a completely genetic risk factor. Meaning, having an elevated LP(a) is almost entirely determined by the genes you inherit. There is no evidence that a healthy lifestyle will lower your Lp(a). However, that does not mean those with high levels shouldn’t practice healthy habits. Reducing other risk factors that are determined by quality of health can still reduce the overall risk of heart disease. Another risk factor that sets LP(a) apart is that it is an independent risk factor. It has been linked to heart disease in younger adults who are otherwise healthy and have no prior cardiovascular risks. Elevated LP(a) has affected the lives of many who are otherwise healthy. For example, Tennis legend Arthur Ashe, who had his first heart attack at age 36. Bob Harper, a celebrity fitness trainer was also affected and nearly died of a heart attack at age 52. Who should be tested for Lp(a)? Studies show that there is a higher risk of a cardiovascular event if Lp(a) levels start to rise above 30 mg/dl. There is an even greater risk at levels 50 mg/dl and higher. There are an estimated one in seven people at or above this threshold. If you’ve had a cardiac event but your cholesterol levels are normal, or you have a family member with heart disease at an early age, have a cardiovascular event despite normal lipid levels, have a family history of Lp(a), or have aortic valvular disease at an early age then you should get tested for Lp(a). As mentioned, Lp(a) is a genetically mediated risk factor. “This means it runs in families,” Albert Lopez, MD, DO, FASPC, internal physician and lipid specialist in Jacksonville, FL says. “Those individuals that have it, you have a 50% chance of giving to your children.” Dr. Lopez believes there should be cascade screening, meaning asking family members if they have it and then getting tested. No FDA approved remedies for Lp(a) Currently there are no FDA approved remedies for elevated Lp(a). Statins, a widely known and used therapy that lowers LDL cholesterol does not reduce Lp(a) and has been shown to sometimes result in a slight increase. One therapy that has been shown to work is asphersis. This process filters a patient’s blood by circulating it through a machine and removing Lp(a) particles. However, this process is reserved for high-risk patients because it is extremely expensive, requires weekly visits and involves risks. After stopping apheresis, the Lp(a) levels begin to rise again. New Advancements in Science regarding Lp(a) Luckily, there are new drugs on the horizon that could potentially help those suffering from elevated Lp(a) levels. “What is exciting is that we are in totally nerd, sci-fi treatments now,” Dr. Lopez says. “We can actually stop your genes from making this protein by using a little snip that crinkles it up and doesnt let it read.” In other words, new studies are using gene silencing techniques to achieve a large and durable reduction of Lp(a). These therapies and medicines are still in clinical trials now. ENCORE Research group is conducting research studies for people with elevated Lp(a) in hopes to find a drug that will lower Lp(a) levels. It is up to the public to participate in these research studies to help those suffering from elevated Lp(a) levels.
A colonoscopy is used to detect any changes in the large intestine and rectum. A long flexible tube, called a colonoscope, is inserted into the rectum during the exam. At the end of the tube is a tiny video camera that allows the provider to view the inside of the colon. During the colonoscopy, your provider may also remove some abnormal tissue or take tissue samples if needed. It is common practice to receive a sedative before the exam to make you feel more comfortable, relaxed and decrease the chance of any pain. Both men and women need colonoscopies around the age of 50. If you are at a high risk for developing colorectal cancer, cancer that affects the colon and the rectum, your provider may ask you to receive a colonoscopy at an earlier age. You should reach out to your healthcare provider if you are having any symptoms of colorectal cancer because getting a colonoscopy could help prevent serious illness or even death. Symptoms include: There are many reasons why a colonoscopy is important. The main reason, as mentioned previously, is to test for colon cancer. Secondly, a colonoscopy investigates any problems with your intestines. If you are experiencing any abdominal pain or intestinal problems, let your doctor know beforehand. This way, your doctor can assess and find the answers to why you may be experiencing these issues. A colonoscopy also looks for abnormal tissues called polyps. A follow up colonoscopy might be necessary to remove all polyps to reduce your risk of colon cancer. Colon cancer is the third most common cancer among men and women over the age of 50. More clinical trials are needed in order to reduce this number and save lives. If you are in need of a colonoscopy, you may qualify for an enrolling study at one of our ENCORE Research Group locations. Participating in research trials have many benefits, including free medical attention, access to new technology and the chance to move medicine forward creating a healthier nation. Source: Borland Groover, American Cancer Society
What is a Colonoscopy?
Who Needs One and When?
Why are They Important?
Are there any Enrolling Studies at ENCORE Research Group?
There are many reasons someone may think it’s scary to participate in a clinical trial. However, if you become more informed about how clinical trials work then those fears will vanish! Below are some common misconceptions about clinical trial participation.
“I won’t be able to quit if I change my mind about participating.”
Many believe that once you sign the informed consent papers to participate, you are locked in until the trial is complete. This is a common misconception. Clinical trials rely on participants who volunteer. You are always able to leave a clinical trial. After you have taken an investigational injection or drug, you are allowed to leave. However, it is important to be open and honest with your clinical team about leaving the trial.
Research participants are guinea pigs.
Thinking about yourself strapped down in a lab while people poke you with needles sounds like a scene right out of a horror movie. It is far from the truth. There are strict guidelines for each clinical trial, and all require special attention to health concerns. There are also ethical and moral guidelines put in place by a committee for each trial, called the Institutional Review Board (IRB). This is a committee made up of health professionals to ensure each trial is ethical. There is a robust screening and preclinical testing process which can take up to six years to complete before a drug is ever given to a patient.
Will it Hurt?
This depends on the type of clinical trial you are participating in. Each process is different. The trials can include taking an investigational pill, undergoing a new procedures or getting an injection. One thing you can be sure of, your health will be closely monitored and you will be aware of all risks and procedures before participating in the trial. You will review and sign the “informed consent” document. This will ensure you know all the risks. The document ensures the patient knows everything involved and is free to choose whether or not to participate. If you ever feel unsure, do not be hesitant to ask your provider any questions!
Will I experience major side effects?
There is some risk when participating in a clinical trial.An investigational drug goes through a robust testing process. Before is is given to a patient, the results must suggest that it is highly likely to be safe and effective. Patients are closely monitored once given an investigational drug to ensure their safety. The informed consent and IRB both take part in ensuring the safety and ethics of every clinical trial.
We asked, “What motivates you to participate in clinical trials?” With over 160 responses, the answer is clear. People who participate in clinical trials are dedicated to helping others by improving medicine for future generations.
We also found that very few were participating in order to receive the stipend for time and travel. This says a lot about the type of people who are willing to participate in clinical trials. They are in it for the cutting edge treatment, and the need to help others.
There is truly only one way to improve healthcare, and that is to participate in clinical trials. Thank you to everyone who responded to our survey, and everyone who participates in these trials.
Can a type of seaweed really be used to treat Alzheimer’s disease? Some scientists think so, and it’s even being tested in clinical trials today. Oligomannate is extracted from seaweed and can be used as a potential therapy for Alzheimer’s. It is being developed by Shanghai Green Valley Pharmaceuticals and has been given conditional approval by China. Oligomannate is in clinical trials in the U.S., Europe, and other countries, pending approval. Alzheimer’s disease is a neurodegenerative disease that worsens over time and is the most common form of dementia. Amyloid plaques and tau tangles are widespread in Alzheimer’s and physically change the brain. Neurons die over the course of the illness, and neural networks become sparsely connected. This leads to the atrophy, or wasting away, of brain matter. This is a visible, significant loss of brain volume. So how does Oligomannate work to stop these proteins from forming plaque? In the preclinical studies, oligomannate was able to decrease the build-up of beta-amyloid protein in the brain, which in turn can improve cognitive function. Furthermore, oligomannate may be able to regulate the connection between microbiomes from the gut to the brain, reduce harmful metabolites produced by these microbiomes, and lessen inflammation. All of which help to reduce the symptoms of Alzheimer’s disease. More research needs to be done before it is FDA-approved in the US. Want to play a part in finding a possible treatment for one of the most devastating diseases? Consider participating in a research study! To see what is enrolling, visit our enrolling studies page. Your help is needed to move medicine forward. Source: Alzheimer’s News Today
The questions that have many people puzzled are finally going to be answered: What is gluten and is it actually bad for you? Gluten is a mixture of two types of proteins. It is responsible for the elastic texture of dough. These proteins are commonly found in wheat, rye, oats and barley. Gluten helps food keep its shape and acts like a glue that holds certain foods together. For those with celiac disease, gluten can be particularly dangerous. Gluten triggers an immune response in people with the disease, resulting in damages in the lining of the small intestine. These damages can obstruct a person’s ability to absorb nutrients from food and lead to problems like osteoporosis, infertility, nerve damage, and seizures. Adults with celiac disease show many digestive and other symptoms including: Digestive symptoms: Non-Digestive Symptoms: Gluten can be found in many different kinds of foods. It may be present in more foods than you think. The main foods to look out for which contain high amounts of gluten are processed foods, such as canned or boxed items, sweets, including cakes, pies and candies, cereals, bread, beer, pasta and more. Currently, the only treatment for celiac disease is to completely eradicate gluten from a person’s diet, which can be difficult. In order to help those suffering from this disease, it is imperative to do more research including participating in clinical trials. If you have celiac disease and want to be at the forefront of medicine, click the “enrolling studies” tab for more information about current clinical trials. Source: Harvard Health, Celiac Disease Foundation
The flu is a respiratory infection caused by a group of viruses. Symptoms range from mild to severe and most commonly include body aches, cough, fever, headache and sore throat. The flu is contagious, spreading through tiny droplets from a cough, sneeze or even talking. We hear about it every year in the fall and winter because the viruses tend to survive longer in those seasons. The flu vaccine is created to protect against influenza strains A and B. Once an individual is vaccinated, the body’s immune system responds by developing antibodies that will be ready to combat future infection. It takes about two weeks after a person has been vaccinated to gain protection. It is not unusual to briefly experience mild fatigue and muscle aches soon after injection as this represents an appropriate immune response, but because the ingredients in the flu shot have been inactivated, it is not possible to get “the flu” from the vaccine. The flu vaccine is recommended for most people over six months of age and is given every year because: The Circulating Flu Viruses Change Influenza viruses undergo structural antigenic change and even mutation. Each February, flu experts gather and review the data to best decide what strains are predicted to circulate in the Northern Hemisphere during the upcoming flu season. Once the top 3 or 4 strains are identified, the viruses are grown then the vaccines manufactured using varying methods to create the safest and most effective flu shot. Typically, there is at least one and usually more than one new strain coverage included each year. Immune Protection Declines Over Time Over time, the antibodies created in response to that year’s vaccine begin to lose their effectiveness, though some individuals who received annual flu shots over many years maintain reserve immunity capable of preventing or softening the blow of a new infection even if challenged with a novel strain. The CDC recommends a yearly flu shot around October. Another advantage to getting the flu shot is that you are less able to carry and spread the virus to others that may have an altered immune status. Due to the fact older individuals don’t mount as robust of an immune response following vaccination, it is especially important for those over 65 years old to get the vaccine annually. The CDC estimated that in the 2018-2019 flu season there were approximately 490,600 hospitalizations and 34,200 deaths from the flu. It’s safe to say the flu is a dangerous but preventable illness. We thank all volunteers that have contributed to now FDA approved and currently enrolling flu vaccine programs. Your participation has helped to save lives. Visit our enrolling studies page for more information as we work together to further develop the best prevention for this serious disease. Source: Centers for Disease Control and Prevention https://pubmed.ncbi.nlm.nih.gov/9360364/ https://www.cdc.gov/flu/prevent/keyfacts.htm https://www.sciencedaily.com/releases/2019/03/190320110619.htm
What is H. pylori? H. pylori is short for helicobacter pylori, and it is a type of bacteria that grows in the stomach and can cause infection. This infection might be a lot more common than you think. With approximately 30-40% of the United States’ population containing the bacteria, there is no question as to how important more research needs to be done to combat it. If left untreated, H. pylori may cause peptic ulcers, gastritis, or stomach cancer. However, it often does not have any symptoms at all. What are the signs and symptoms? Many who contract H. pylori experience no symptoms at all, however when symptoms do occur, here is what you can expect: How do I get H. Pylori? Contracting H. pylori is common, and even more prevalent in developing countries. Some factors may increase your risk of infection like sharing a small, crowded living space, no access to clean water, and living with someone who has H. pylori. Some ways to reduce your risk of infection are to wash your hands before eating and after using the bathroom. Eat food that has been properly prepared and drink clean water. When should I see a doctor? As a good rule of thumb, you should always see a doctor if you have worsening stomach pains. You should also see a doctor if you have: Researchers are studying new ways to treat H. pylori infection and ENCORE Research Group is conducting some of these clinical trials. If you would like to help move research and medicine forward, visit our enrolling studies page to see clinical trials that are enrolling now in your area. Source: U.S. National Library on Medicine, Everyday Health, American Journal of Gastroenterology
Adjuvant- Adjuvant is an element used in some vaccines that helps build a stronger immune response in patients receiving the vaccine. Essentially, it adds an extra boost to the vaccine and helps it work better. Antibody- Antibodies is a blood protein that combines with substances the body believes to be foreign, such as bacteria, viruses and other alien substances in the blood. The antibodies work to combat these foreign substances. Antigen- An antigen is a name given to a foreign substance in the body whose presence creates an immune response in the body. A good example of the body creating an immune response is the production of antibodies. Placebo- A placebo is a harmless pill or vaccine that is given to patients in a clinical trial as a controlled group. When given a placebo, researchers can then determine if there is a psychological effect or physical one, compared to the actual vaccine or medication. Titer- A titer test is a simple blood test to check for the presence of certain antibodies in the bloodstream. Vaccination- A vaccination is a treatment using a vaccine to create an immunity to a certain disease or diseases. Vaccine- A vaccine is a substance that is used to create the production of antibodies to produce an immunity against one or more diseases in the body. It is prepared by using an agent of a disease, its products, or a synthetic substitute to act as an antigen without actually inducing the disease. Pathogen- In a broad sense, a pathogen is anything that can produce a disease. It is anything that can cause illness to the host. Quadrivalent– a quadrivalent is a type of vaccine that works by creating an immune response against four different antigens, or foreign substances in the body such as viruses. A popular quadrivalent is Gardasil, which protects against 4 different strains of HPV. Egg-Based- Egg-based vaccines are vaccines that are injected into fertilized eggs and then incubated for several days. This allows the virus to replicate and then the fluid containing the virus is harvested from the egg. Cell-based- Cell based vaccines are created from mammalian cells lines rather than egg-based. The benefit of cell-based vaccines is the ability to mass produce vaccine supplies at a quicker rate. Recombinant Vaccine- Instead of taking a strand of the virus, a recombinant vaccine involves inserting a DNA coding of an antigen which will stimulate an immune response from the body. Conjugate Vaccine- This is a type of vaccine that contains a combination of weak and strong antigens. The weak antigen is paired with the strong antigen to produce a stronger immune system response from the body. Efficacy- Efficacy is the ability for a medication or vaccine to produce the intended result. Immunity– When you are immune to something, it means your body has a significant amount of biological defences to avoid infection, disease, or other unwanted antigen. Inactivated Vaccine- Can also be called a killed vaccine. An inactive vaccine consists of virus particles, bacteria, or other pathogens that have been killed by heat or chemicals. The dead cells are then introduced into the body. The immune system can still learn from the inactivated virus’s antigens and learn how to fight the live version in the future. Investigational- During a clinical trial’s investigational phase, the drug or medical procedure in question is not yet approved for general use. However, it is undergoing phases in clinical trials in hopes to become approved. Live Vaccine- Live vaccines are a weakened form of the antigen that causes a disease. Since the vaccines are so similar to the original disease, the body forms a long-lasting immune response. Source: CDC, National Institutes of Health, Healthline
Eosinophilic Esophagitis (EoE) is a chronic, immune-mediated disorder. It occurs in approximately 1 in 10,000 people and affects people of all age groups, with males being affected more frequently. EOE is associated with food allergies or other allergens, causing eosinophils (type of white blood cell) to migrate from the bone marrow (via blood) and settle in the esophagus causing inflammation to the esophagus. No one knows exactly why EoE occurs. People with EoE tend to have allergic conditions such asthma, seasonal allergies, allergic rhinitis, and eczema. Symptoms of EoE: EoE symptoms can overlap with symptoms of a condition called gastroesophageal reflux disease (GERD). Patients with EoE experience symptoms described as, If EoE is not controlled, the eosinophils will cause damage to the esophagus. Sometimes food that gets stuck in the esophagus (food impaction) may require emergency removal. How is EoE Diagnosed? If you have symptoms of EoE, your doctor will order a procedure called an endoscopy (EGD). An EGD is required to confirm the diagnosis and is performed by a specialist called a gastroenterologist. Patients are sedated for this procedure and a small flexible tube with a light and camera on the tip is inserted into the patient’s mouth. During the endoscopy, several biopsies of the esophagus will be taken and sent to the laboratory for analysis under a high-power microscope. EoE is confirmed when 15 or more eosinophils per high-power field are found (≥15 Eos/hpf). How is EoE Treated? Many patients with EoE are initially treated for GERD using a medication called a proton pump inhibitor (PPI). However, most EoE patients do no respond to anti-GERD treatment. Treatment with PPIs is given for a minimum of 8 weeks followed by a repeat EGD and biopsy. If the eosinophil count remains elevated (≥15/hpf), the diagnosis of EoE is confirmed and a different treatment is given. Patients with EoE are often referred to an allergy specialist for evaluation. Allergy testing can be done to identify which foods are triggering the EoE. Treatment for EoE usually includes dietary management and/or medication, or treatment on a clinical trial. If you have symptoms of EoE, it is important that you seek medical care and discuss your symptoms with your doctor. You can also learn more about EoE from advocacy organizations such as Apfed (apfed.org), or by joining an on-line patient communities such as Healtheo360 (healtheo360.com). Research is currently being conducted around the United States for this condition. Here at ENCORE Research Group we have 3 research sites with a new opportunity for people who have Eosinophilic Esophagitis. If you’re interested in learning more about this research, please contact your local research office below! Jacksonville: ENCORE Borland Groover Clinical Research 904-680-0872 Fleming Island Fleming Island Center for Clinical Research 904-621-0390 Inverness: Nature Coast Clinical Research 352-341-2100
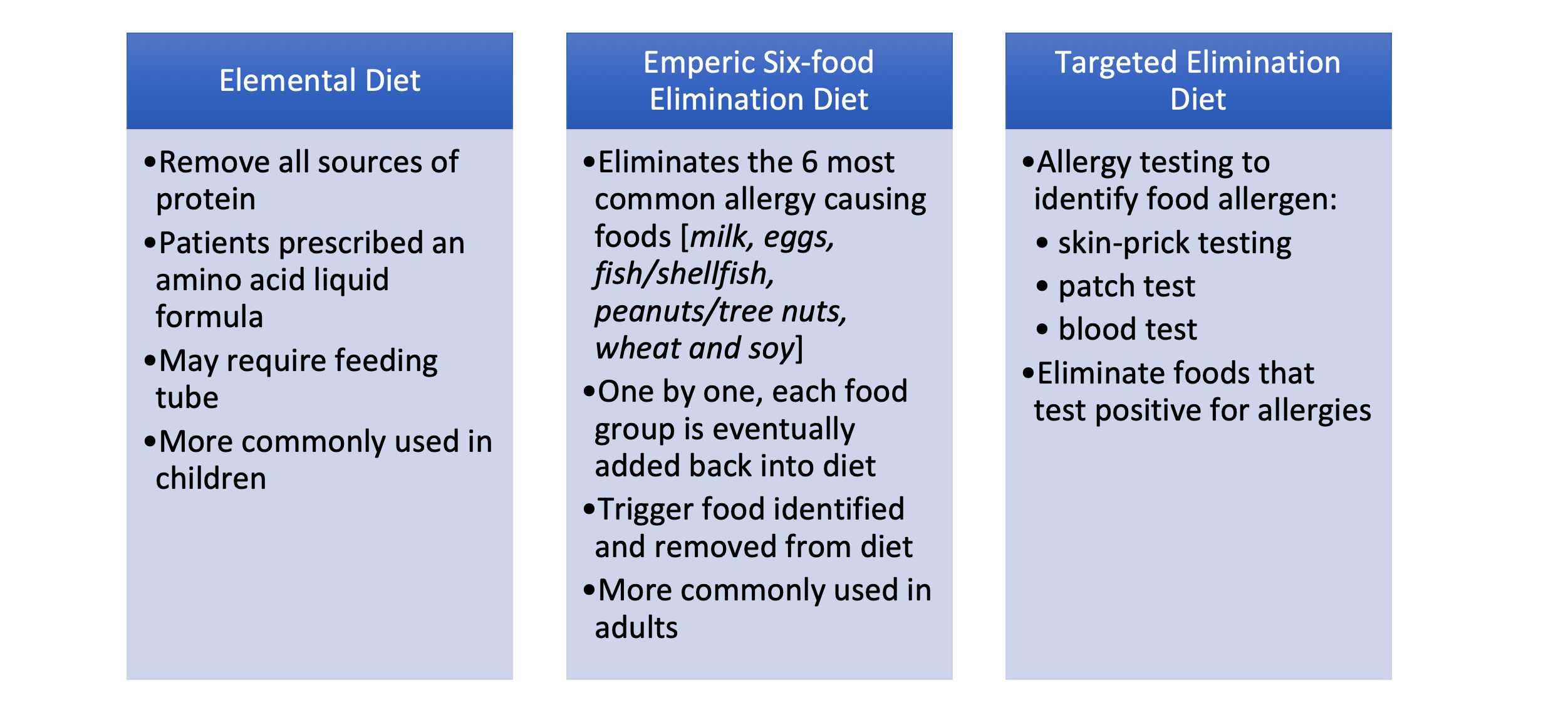

Plantar Fibromatosis, or Ledderhose disease, is a rare condition. It stems from a disease called plantar fibroma, where the tissue hardens and a growth begins in the arch of your foot. Plantar Fibromatosis is diagnosed when the tissue hardens to an excessive amount, and many lumps form on the bottom of the foot. The disease can affect one or both feet. It also can affect anyone at any age, but it is more prevalent in middle-aged or older people. The growths are not cancerous but can cause severe pain. As mentioned, plantar fibromatosis can cause pain and any out-of-the-ordinary pain should be a cause for concern resulting in a talk with your doctor. Other symptoms include: When it comes to treatment, we still have more to do in order to fully treat and relieve the pain for those suffering with plantar fibromatosis. Some current treatments are: There are newer treatments and research on plantar fibromatosis, including a treatment that uses injections on an enzyme, called collagenase, to break down the thicker tissue on the bottom of the foot. This exciting research is one of the few treatments being tested that would actually resolve these painful lesions. More research is needed in order to cure plantar fibromatosis for good, so those with the disease can live their lives without the painful lumps. Currently, ENCORE Research Group is conducting clinical trials for plantar fibromatosis. For more information on our current studies click the “enrolling studies” tab. Sources: Healthline, National Library of Medicine , FootCareMD
Should I be concerned?
How is the disease treated?
At some point in our lives we have all experienced acid reflux. Maybe it was after eating something spicy, or any acidic food like a tomato or certain dairy products and you felt a burning sensation in your throat. GERD, or gastroesophageal reflux disease is similar to acid reflux. GERD is a long-term condition where acid from your stomach overflows into the esophagus. If you experience acid reflux that occurs more than twice a week, your doctor may diagnose you with GERD. If you are experiencing these below symptoms more than twice a week, it may be time to see a doctor. Although GERD is a common condition affecting over 3 million Americans per year, if left untreated, it can lead to serious medical conditions. With certain lifestyle changes and medication, GERD can be treated. However, more research is needed to understand why there is a steady increase in Americans with GERD. Currently, ENCORE Research Group has enrolling studies for GERD taking place in Crystal River and Jacksonville. Visit our Enrolling Studies page to see what’s enrolling at a research site near you. Source: Medical News Today, Medline Plus
Low testosterone levels in men, or hypogonadism, may affect more men in the U.S. than you think. In fact, it is estimated the 4 to 5 million men in the U.S. have experienced this. Hypogonadism is a deficiency in male gonadal function resulting in insufficient testosterone secretion. This can be caused by testicular failure or hypothalamic-pituitary axis dysfunction, or both. As a result, it is difficult for a man to maintain testosterone-dependent functions. Men can be diagnosed with hypogonadism at any age, but it is more prevalent in older males. Some of the signs and symptoms of low testosterone include: As a man ages, their testosterone levels start to decrease by 1 to 2% naturally every year beginning at age 40. The higher the percent, the worse the symptoms. However, there are risk factors that can speed up this process. These risk factors include: In order to diagnose low testosterone a doctor must give a physical exam, review the symptoms, and review the results of multiple blood tests. Once diagnosed, low testosterone therapy could be an option, but not the first choice. This is because increased levels of testosterone are a major risk factor for prostate cancer. However, there are other ways to help slow hypogonadism, such as a skin patch or injections. The latest studies suggest that low testosterone levels in adult men is often underdiagnosed and under tested. This could be due to easily attributing these symptoms to age, or it being looked over by both medical professionals and patients. Participating in clinical trials is the best way to help increase knowledge and find new treatments for low testosterone. Sources: Harvard Health, Boston University School of Medicine
There are five forms of antibodies that the human body makes. There are two forms that are relevant for COVID 19, Igm and IgG. Igm is a big molecule, which is the first molecule that your body makes when you are exposed to a particular antigen or virus. This is an acute phase type of antibody. IgG is a long-term antibody that has memory for your immune system and also protects you long-term. The actual length of long-term protection is not known. Typically, when you have antibody testing, you are tested for both Igm and IgG. These tests are not perfect. If someone tests positive for Igm but not IgG, we’re not sure if they are protected. If someone has no Igm antibodies and lots of IgG antibodies, they’re likely protected due to the long-term memory of IgG. The length of time the antibodies remain detectable following an infection is not known. Source: cdc.gov Amgen Powerpoint
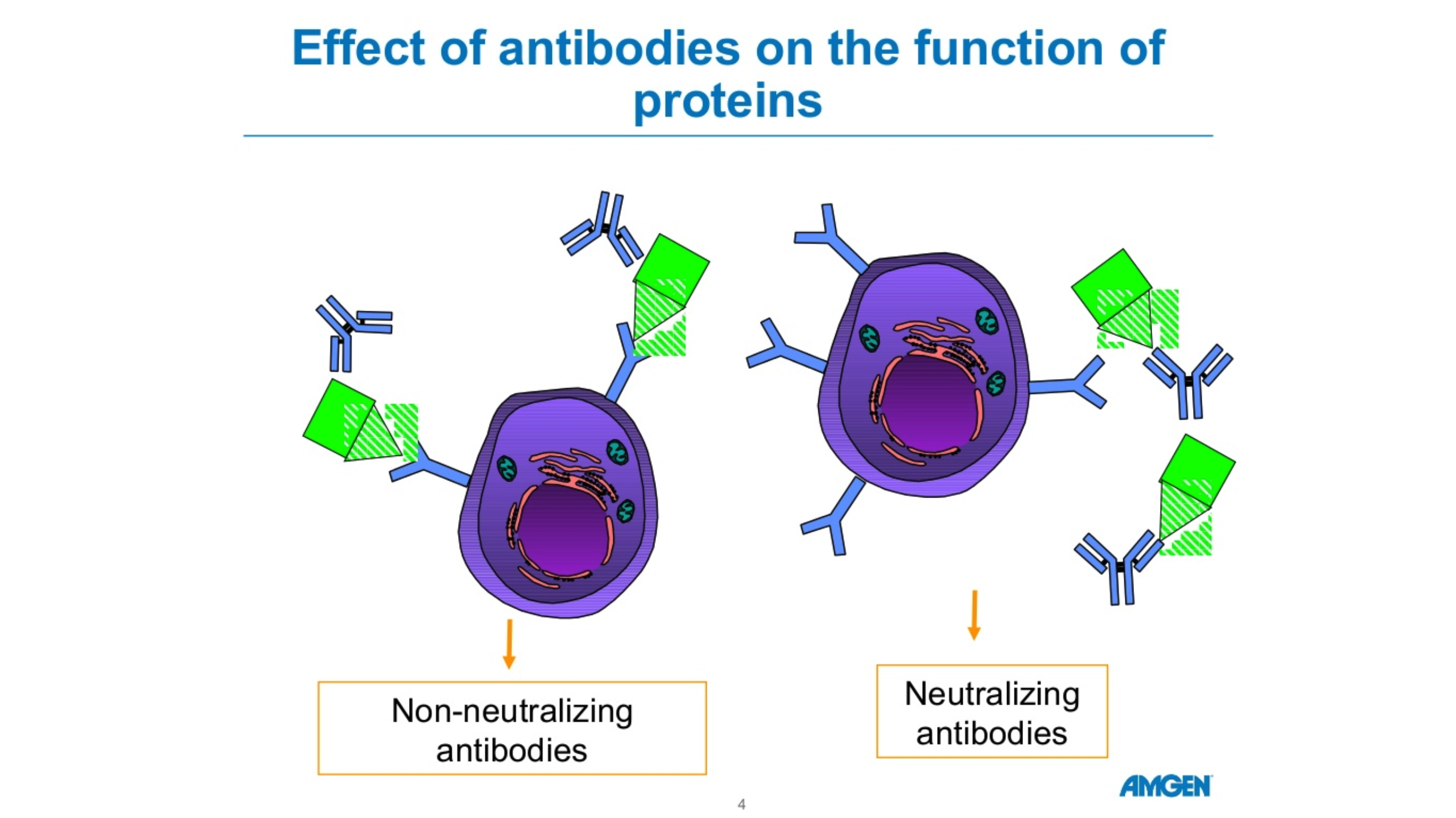
Ulcerative Colitis is a rare inflammatory bowel disease (IBD) with less than 200,000 cases per year. Ulcerative colitis can cause long-term effects on the body including inflammation and ulcers in the digestive tract. This can affect the innermost lining of the large intestine as well as the rectum. The symptoms of ulcerative colitis can range from mild to severe. Symptoms include rectal bleeding, bloody diarrhea, abdominal cramps and pain. Those who have Ulcerative Colitis are also at a greater risk of developing colon cancer. Doctors usually diagnose the different types of ulcerative colitis according to its location in the large intestine. The different types of ulcerative colitis include: Ulcerative Proctitis This is when the inflammation is in the area closest to the rectum. Rectal bleeding may be a sign of this disease, and it tends to be the mildest form. Proctosigmoiditis This type of ulcerative colitis is confined to the rectum as well as the lower end of the colon (sigmoid colon). Symptoms include abdominal cramps, bloody diarrhea, and the inability to move bowels, even though you feel as though you need to. Left-sided colitis If you have sharp pain on your left side, bloody diarrhea, abdominal cramping or weight loss, you may be experiencing left-sided colitis. This happens when inflammation extends from the rectum through the sigmoid and descending colon. Pancolitis Pancolitis often affects the entire colon. This can cause severe bloody diarrhea, abdominal cramps and pain, fatigue and weight loss. Acute severe ulcerative colitis This form of colitis is rare. It is a severe form and it affects the entire colon. It can cause severe pain, profuse bloody diarrhea, fever and complete loss of appetite. Although rare, ulcerative colitis can cause an abundance of health problems. It is imperative to participate in clinical trials in order to move medicine forward and help find effective treatments for ulcerative colitis sufferers. Resources: Cleveland Clinic, Crohn’s and Colitis
Crohn’s disease is a chronic irritable bowel disease (IBD). In those with crohn’s disease, an abnormal immune system causes chronic inflammation in the digestive tract. IBD affects nearly 3 million Americans, and there is still no known cure.
Symptoms of Crohn’s Disease
A person living with crohn’s disease can experience many symptoms and the severity can range from no pain at all to immobilizing. The symptoms include:
- Diarrhea
- Abdominal pain
- Cramping
- Weight Loss
- Blood in Stools
- Fatigue
- Nausea and vomiting
- No appetite
- Anemia
- Fever
Long-Term effects of Crohn’s Disease
Living with crohn’s disease can take its toll on the body long term. If left unmanaged, crohn’s disease can worsen and cause extreme pain and health concerns. Over time, crohn’s disease can cause severe damage to the GI tract. This can lead to:
- Fistulas. When excessive inflammation causes ulcers to form on the intestine, a fistula can form. A fistula is when two parts of the intestine connect to form a tunnel to drain the pus from the infected area.
- Intestinal Abscesses. This is caused by an excess of bacteria in the abdomen.
- Intestinal Blockages. This is a blockage that keeps food or liquid from passing through the small or large intestine. Symptoms can include severe abdominal pain, vomiting and inability to pass gas or stool.
- Internal Bleeding. This internal bleeding is caused by tears in the bowel wall due to inflammation in the colon. It is often the cause for diarrhea or bloody stool, a common symptom of crohn’s disease.
Crohn’s disease can be managed and those with the disease can live a very fulfilling life. The main goal of management is to treat the inflammation, which should reduce the severity of the symptoms and hopefully lead to long-term remission.
As mentioned, there is no known cure for crohn’s disease. The only way to find a cure and help those living with crohn’s disease is to participate in clinical trials to further research and hopefully, find a cure.
Resources: Centers for Disease Control and Prevention, Crohn’s and Colitis Foundation, Bladder and Bowel
Chronic pancreatitis is inflammation of the pancreas that does not heal but worsens over time. When you have chronic pancreatitis, your digestive enzymes begin to digest the pancreas itself. The pancreas is a small gland behind the stomach that secretes digestive juices into the small intestine. Eventually, chronic pancreatitis can damage a person’s digestive system and ability to make pancreatic hormones.
Some common causes of chronic pancreatitis are, but not limited to:
- Alcoholism
- Family history
- Autoimmune diseases
- A blocked pancreatic duct
- A genetic mutation such as mutations of the cystic fibrosis
Chronic pancreatitis, if unmanaged, can lead to:
- Diabetes- Chronic pancreatitis causes damage to the insulin-producing cells resulting in diabetes, a chronic condition where there is an abnormally high level of sugar in the blood.
- Pancreatic Cancer- If you have chronic pancreatitis, you are at an increased risk of developing pancreatic cancer by two to three
- Malnutrition- Chronic pancreatitis can cause your pancreas to produce fewer enzymes that are needed to break down and process nutrients from your Overtime, this may lead to malnutrition and significant weight loss.
Although there are many complications that may arise if you are living with chronic pancreatitis, the disease is treatable if caught in time. For chronic pancreatitis the treatments can be a hospital visit to treat dehydration, pain medication and a lifestyle change to a low-fat diet.
According to the type of pancreatitis that you have, other surgeries may be required.
One of the worst symptoms of pancreatitis is the severe abdominal pain. Currently, the only remedy for this is pain medication. In order to better understand and treat this pain more research needs to be done. The goal is to improve the quality of life and the risk of complications when living with pancreatitis.
Sources: MedlinePlus, Pancreatic Cancer Action, National Institute of Diabetes and Digestive and Kidney Diseases, National Pancreatitis foundation
What Are Triglycerides? Triglycerides are a type of fat (lipid) found in your blood. You get them in two ways – from the food you eat and from what your liver makes. Eating too many calories, especially from high carbohydrate foods, could lead to high triglycerides (hypertriglyceridemia), as could certain medications. High triglycerides could also be a sign of diabetes or thyroid problems, or be genetic. Almost 1 in 3 Americans have high triglycerides. When you have excess triglycerides, they are stored in the fat cells for later use. When they are needed, your body releases them as fatty acids, which fuel body movement, create heat, and provide energy for the body processes. A fasting blood test can tell where your triglyceride level falls. For good health, your triglyceride level should be less than 150 mg/dL. Borderline high levels are 150-199 mg/dL. High is 200-499 mg/dL. Very high is more than 500 mg/dL Diet and Lifestyle Changes to reduce High Triglycerides Consume less sugar and refined carbohydrates – limit white breads, white rice, white potatoes, sweetened beverages, sugary cereals, cakes and cookies. Instead choose whole grain breads, quinoa or wild rice, and fresh fruits and vegetables. Aim for 30 grams of fiber a day. Choose Healthy fats – use unsaturated fats such as olive and avocado oils. Eat fish, poultry, less red meat, and enjoy some meatless meals. Limit your intake of alcohol – for some people drinking even a little bit can have a big effect on triglycerides. One of the best ways to lower triglycerides is with regular exercise. Aim for an average of 40 minutes of moderate to high intensity exercise on 3 to 4 days a week. Taking a brisk walk every day works for many people. When Healthy Lifestyle Changes Are Not Enough Your doctor may recommend medication to help lower your high triglycerides, such as nicotinic acid (niacin), fibrates, omega-3-fatty acids (fish oil) or statins. There are also some new medications being developed that may not only lower your triglycerides, but reduce your risk of heart disease overall. Many of our research sites are participating in these important clinical trials. We invite you to contact one of our sites near you to see if you could benefit from one of these programs. Lori Alexander, MSHS, RDN, CCRC, CLS, FNLA Director, ENCORE Lipid Center of Excellence
Idiopathic hypersomnia (IH) is a rare neurological sleep disorder that can drastically affect a person’s life. Those suffering from IH have a hard time staying awake and alert during the day. They may fall asleep at inappropriate times and not notice. There is no FDA approved treatment for IH. Some can take medication, typically taken for narcolepsy, to improve symptoms. Unlike narcolepsy, scheduled naps will not help those suffering from IH. A key symptom that differentiates IH from other sleep disorders is long naps that are not refreshing with no known cause. Symptoms IH’s symptoms are severe and typically disrupt daily activities. It can be difficult to drive, work, go to school and do other daily tasks we take for granted. To better understand IH we need to learn the symptoms. Common symptoms include: Treatment As mentioned, there is no known FDA approved treatment for IH. The treatment is usually aimed at addressing the excessive daytime sleepiness over other symptoms, typically with medication. What really sets IH apart and differentiates it from other sleeping conditions is that it usually can not be improved through lifestyle changes. Those with IH do not have energizing sleep, so frequent planned naps and improving sleep at night typically do not work. Participating in clinical trials is one of the best ways to find a cure for IH, or improve the symptoms and create a better quality of life. Source: Generic and Rare Disease Information Center, Medline Plus
Narcolepsy is a sleep disturbance characterized by a disabling level of daytime sleepiness. It is estimated that one in every 2,000 Americans suffer from narcolepsy, yet about 25% have been diagnosed and are receiving treatment.
Those suffering from narcolepsy can experience “sleep attacks” that are repeated throughout the day. They can even occur during daily routines like eating, walking or driving and are not as a result of inadequate sleep.
Going undiagnosed, narcolepsy can be socially disabling and isolating leading to depression. Type 2 diabetes can also occur in people with untreated narcolepsy. Unfortunately, only about 5% of patients seen in a sleep lab are narcolepsy patients. In order to improve these numbers and better diagnose narcolepsy, it is vital to know the early symptoms.
Symptoms of narcolepsy usually occur in young adults ages 15 to 25. Symptoms can include:
- Excessive daytime sleepiness (EDS): This is the primary symptom of narcolepsy. You may have sudden urges to fall asleep, even if you have had a full night’s sleep.
- Hallucinations: Some narcolepsy patients experience very real hallucinations while sleeping. These hallucinations are typically a presence in the room and can be very disturbing and disruptive.
- Sleep paralysis: You might lose the ability to move while either falling asleep or waking up. Sleep paralysis can be paired with hallucinations.
- Disturbed nighttime sleep: About 50% of people with narcolepsy have troubles sleeping through the night, often times waking up frequently.
- Memory problems: EDS can cause memory problems. You may not remember something someone told you because you were not fully awake at the time.
- Cataplexy- Is a sudden loss in muscle tone and only happens if you have narcolepsy coupled with cataplexy. Cataplexy can occur when there is extreme emotion, for example being surprised. Your muscles can become weak or even paralyzed.
Seeking a doctor for treatment of narcolepsy is vital, but there are lifestyle changes that can be made to manage the disease as well. Examples include maintaining a consistent sleep schedule and planning to take frequent naps throughout the day. Otherwise, treatment for narcolepsy involves medication.
With a new understanding of narcolepsy, researchers are creating different ways for treating the disorder. Some programs are experimenting with ways to increase brain levels of histamine, a brain chemical that is effective in improving alertness.
Other researchers are working on ways to improve hypocretin, which are neurotransmitters that promote wakefulness and regulate sleep. Narcolepsy coupled with cataplexy is caused by a loss of brain cells that produce these neurotransmitters. The goal is to improve narcolepsy symptoms by restoring hypocretin production in the brain.
Sources: American Academy of Sleep Medicine, Narcolepsy Network, Sleep Education, Harvard Medical
Sleep apnea affects approximately 22 million adults in the US, yet 80% of sleep apnea cases remain undiagnosed. If undiagnosed, sleep apnea could lead to cardiovascular disease and diabetes. With cardiovascular disease being the number one killer of both men and women, it is vital to be seen by a doctor for treatment.
What is Sleep Apnea?
Sleep apnea is an obstructive condition that prevents your body from receiving an adequate amount of oxygen causing interruptions in regular sleeping patterns. There are two main types of sleep apnea, obstructive and central. Obstructive sleep apnea occurs when there is a blockage in the airway. The tongue relaxes and blocks the back of the throat while sleeping.
Central sleep apnea occurs when the brain fails to communicate to the muscles to breathe.
Both of these conditions can cause the body to lose oxygen and wake up frequently throughout the night. This can result in daytime fatigue and sleepiness. Other symptoms include loud snoring, morning headaches and insomnia.
How is Sleep Apnea Treated?
The only way to properly diagnose sleep apnea is through a sleep study. Sleep studies are done at a sleep laboratory or can be taken home depending on the physician’s orders. Once diagnosed, the patient may be given a positive airway pressure (PAP) machine. This machine is worn over the mouth and pumps air through the nose and throat to ensure airways stay open. Other treatments include mouthguards to keep the tongue from blocking airways, weight loss, and avoiding sleeping on one’s back.
For best practice, always talk to your doctor if you are having trouble sleeping through the night.
Already diagnosed with sleep apnea? Consider participating in clinical research trial. It is one of the best ways to help improve medical treatments and increase the knowledge that researchers have about sleep apnea.
Chikungunya (chik·un·gun·ya) virus or CHIKV is an infection spread by a two types of Aedes mosquitoes, the yellow fever and Asian tiger species. These are the same mosquitoes that transmit Dengue and Zika virus. The name “chikungunya” derives from the Tanzanian word meaning “to become contorted”, and describes the stooped appearance of sufferers with joint pain. The virus is spread when a mosquito bites (feeds on) an infected individual then passes it on to a non-infected person on a subsequent bite. The Asian tiger mosquito has gradually become the dominant species in the US and is recognized for its ability to survive colder temperatures, therefore posing risk for infection spread into Florida and southeast USA. In 2019, Chikungunya virus infections were identified in 26 US states.
Symptoms:
Most patients who become infected develop high fever and joint pains within approximately a week. The severity varies but some patients experience debilitating aches which continue for years. The pain is caused by the immune system attacking itself causing inflammation of the tissue. Other symptoms of CHIKV viruses include:
- Headache
- Rash
- Muscle pain
- Pink eye
- Bent posture
Rare complications can occur. Infants and elderly adults are at highest risk for:
- Retinitis (inflammation of the retina in the eye which can cause permanent damage)
- Myocarditis (inflammation of the heart muscle which can lead to heart failure)
- Cranial nerve injury leading to facial pain, dizziness, hearing loss, facial twitch
Prevention:
Prevention methods include:
- Mosquito repellent (DEET, picaridin, or lemon eucalyptus applied to skin; permethrin applied to clothing)
- When practical, wear long sleeves and pants when exposed to Aedes mosquitoes
- When traveling to other countries, stay in places with air conditioning, window and door screens, netting
- Isolate the infected person from mosquitoes to prevent a fresh bite which can lead to spread to the next person
Treatments:
There is currently no antiviral therapy approved for Chikungunya. Treatments are focused on helping to relieve symptoms and spread.
Due to public health concerns over the potential for disease outbreak, the FDA granted “Fast Track” status in 2018 for development of the first effective and safe vaccine to prevent virus spread. You can help improve the future of medicine by participating in clinical trials. To learn more about participating in clinical research, visit our enrolling studies page or call us today!
References:
- https://www.who.int/news-room/fact-sheets/detail/chikungunya
- https://www.cdc.gov/chikungunya/hc/clinicalevaluation.html
- http://edis.ifas.ufl.edu/in696
- https://www.mosquito.org/page/repellents
The old saying goes: Men are from Mars and Women are from Venus. This exaggeration is- well… an exaggeration, but there are some differences between male and female heart health that causes an inkling of truth to shine out through the expression. The most common kind of heart disease, among both men and women, is coronary artery disease. Coronary artery disease is caused when cholesterol plaque is built up inside the arteries, and if left untreated coronary artery disease can obstruct blood flow to the heart muscle and lead to a heart attack.
When experiencing a heart attack, the individual will usually experience chest pain, shortness of breath, and pain in their left arm, but these symptoms are not universal. Remember when we were talking about the differences between men and women? Women are more likely to experience uncommon heart attack symptoms than men are! These symptoms can include indigestion, pain in both arms, unusual fatigue and abdominal discomfort. Physicians are still uncertain why women are more likely to experience unusual symptoms. There are some theories about hormonal changes and the difference in valve and vessel sizes, but for the most part it is still unknown.
Lowering your risk of a heart attack, however, is not a mystery. Research shows staying active, eating healthy, and monitoring your blood pressure and cholesterol levels regularly leads to decreased cardiovascular risk. Research also shows that individuals involved in clinical research have better health care outcomes than those who are not.
We are currently enrolling in studies that may help you lower important factors like elevated triglycerides and cholesterol which may help lower your risk of cardiovascular events.
References:
https://www.hopkinsmedicine.org/heart_vascular_institute/centers_excellence/womens_cardiovascular_health_center/patient_information/health_topics/menopause_cardiovascular_system.html
https://www.lahey.org/article/differences-between-mens-and-womens-hearts/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3018605/
https://www.clinicaltrials.gov
Glaucoma is a common eye disease that can gradually steal your vision. The term glaucoma refers to a collection of eye diseases that damage the optic nerve. This damage can lead to permanent vision loss or even total blindness. Glaucoma is considered a major cause of blindness in the general population.
A major concern is that glaucoma often presents no early symptoms but continues to cause gradual, un-reversable damage. In most cases, glaucoma is diagnosed in people who are older than 40 but can still develop at an earlier age. An estimated 3.54% of adults between 40 and 80 years have been diagnosed with some type of glaucoma.
Causes Of Glaucoma
In most types of glaucoma, the eye’s drainage system becomes clogged so the intraocular fluid cannot drain. As the fluid builds up, it causes pressure to build inside the eye. High pressure damages the sensitive optic nerve and results in vision loss.
People are more likely to develop glaucoma if they:
- Are over the age of 40
- Have a family history of glaucoma
- Have high blood pressure, heart disease, diabetes, or sickle cell anemia
- Are of African American, Irish, Russian, Japanese, Hispanic, Inuit, or Scandinavian descent
- Take certain steroid medications such as prednisone
- Have had an injury to your eye or eyes
- Have high eye pressure (ocular hypertension)
Current Treatments Available
Unfortunately, there is not currently a cure for glaucoma. However, there are several therapies that can help reduce eye pressure and the rate of damage to the optic nerve. Current approved treatment options for glaucoma include eyedrops, oral medications, laser surgery, or microsurgery.
Clinical Research Advancements
New clinical trials for glaucoma are focused on more innovative ways to treat the disease. Researchers are studying everything from electric current stimulation to slow release eye implants to help find relief for patients with glaucoma.
You can help advance medical research by participating in a clinical trial! Contact any of our offices to see what clinical trials are enrolling today.
References:
https://www.aaojournal.org/article/S0161-6420(14)00433-3/abstract
https://www.mayoclinic.org/diseases-conditions/glaucoma/symptoms-causes/syc-20372839
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4927811/
Cholesterol has earned a bad reputation over the years. However, it is required by every part of your body for day to day functions. In fact, cholesterol is so important to daily function, that every cell in the body can make cholesterol from basic materials, except your eyelashes! So how do you reconcile these two completely different ideas? The cholesterol that circulates in your blood stream is the extra stuff that your body is trying to get rid of. This extra cholesterol is what can cause damage to arteries, heart disease, and increase your risk for stroke.
So, what is cholesterol? It is a type of waxy, fat-like substance, also called a lipid. Since cholesterol is a fat, it can’t travel alone in the bloodstream. It would end up as useless globs (imagine bacon fat floating in a pot of water). To get around this problem, the body packages cholesterol and other lipids into minuscule protein-covered particles that mix easily with blood. These tiny particles, called lipoproteins (lipid plus protein), move cholesterol and other fats throughout the body.1
LDL (low-density lipoprotein) is considered the “bad”, unhealthy cholesterol that can build up in the arteries and form deposits called plaques.
HDL (high-density lipoprotein) is the “good”, healthy kind of cholesterol that transports excess LDL cholesterol to the liver to be removed from the body.
PCSK9 is a protein in our body that regulates the circulating levels of LDL “bad” cholesterol. Decreasing the PCSK9 proteins in the body will reduce LDL levels and reduce the risk of heart attack and stroke.
There are currently two FDA approved medications that have been very successful in blocking the PCSK9 protein once it has been made. They are Repatha and Praluent. However, the medications are expensive and not approved for all patients under their insurance.
Scientists believe it would be even more powerful to prevent the PCSK9 protein from being made in the first place. Currently being studied are a new class of molecules called antisense oligonucleotides (ASO). ASOs are pieces of DNA that short-circuit the production of PCSK9, resulting in reduced LDL levels and associated risks.
When you participate in a clinical research study, you gain access to these types of cutting-edge therapies at no cost and before the general population. Contact us to schedule a free consultation to see if you qualify for one of our clinical research studies. If you qualify for one of our clinical trials, your health will be closely monitored by our team of expert medical professionals throughout the trial.
Reference:
- https://www.health.harvard.edu/heart-health/how-its-made-cholesterol-production-in-your-body
According to current studies, more than 8 million Americans suffer from psoriasis, but what is it really? By definition, psoriasis is a condition that causes skin cells to multiply rapidly, and consequently build-up on the surface of the skin. This can cause scaly, red patches that are often itchy, painful, and sore. While the exact cause is unclear, psoriasis is thought to be related to an immune system issue with T-cells and other white blood cells, called neutrophils, in the body. T-cells normally travel through the body to defend against internal intruders, such as viruses or bacteria. But if you have psoriasis, the T-cells attack healthy skin cells by mistake, as if to heal a wound or to fight an infection, thus causing a scaly build-up of skin cells on the surface.
While it is considered a chronic condition, fortunately psoriasis can be managed through a variety of methods. Check out our top tips for managing psoriasis and its symptoms below!
-
Avoid Stressors
While stress is never 100% avoidable, you can give your body a fighting chance and help prevent psoriasis flare-ups by staying away from certain internal and external stressors. It’s a well-known fact that tobacco and alcohol can compromise even the healthiest of immune systems, but if you suffer from psoriasis, you’ll want to avoid that second glass of wine or after supper cigarette. Additionally, why you may not be able to avoid stress at work or home, adopting some easy stress release practices, such as yoga or meditation, may help reduce stress enough to prevent your immune system from going into overdrive.
-
Treat Your Skin Right
Did you know bathing or showering in hot water could make your psoriasis worse? Hot water is notorious for drying out the skin and causing flare-ups. We recommend soaking or showering in lukewarm water to help prevent a painful trigger. Additionally, a lukewarm bath with epsom salts, milk, or olive oil could help relieve the painful symptoms of psoriasis. In fact, mixing a tablespoon of olive oil with your body moisturizer actually helps to seal in essential moisture, and adds an additional layer of topical protection when applied to active psoriasis breakouts.
-
Consider Participating in a Clinical Trial
Modern medicine continues to make incredible strides in helping to manage psoriasis, with Jacksonville Center for Clinical Research on the front lines of exploring new and exciting treatments. Contact us to schedule a free consultation to see if you qualify for one of our clinical research studies. If you qualify for one of our clinical trials, your health will be closely monitored by our team of expert medical professionals throughout the trial. It is an accepted statistic that people who participate in clinical trials generally improve their overall health, as they are given access to cutting edge clinical techniques and healthcare experts dedicated to their individual needs.
More than just diarrhea…
Inflammatory Bowel Diseases include Crohn’s Disease and Ulcerative Colitis. These diseases cause inflammation in the digestive tract. Both diseases can have similar symptoms such as diarrhea, urgency, abdominal pain and cramping, fatigue, and rectal bleeding.
What’s the difference between Crohn’s and Ulcerative Colitis?
Crohn’s Disease can cause inflammation anywhere in the digestive tract, from the mouth to the anus. Ulcerative Colitis (UC) affects only the colon (also known as large intestine or large bowel). UC causes ulcers along with the inflammation and puts those affected at a higher risk of developing colon cancer.
What causes Ulcerative Colitis?
Physicians used to believe that stress and diet choices caused ulcerative colitis. Physicians now believe that UC was already present, and can be aggravated by these factors.
Research has shown that the immune system plays a role in developing Ulcerative Colitis.
My own immune system is giving me this disease?
There is no clear cause of UC. Medical science shows that an overactive immune system may be to blame. This can lead to continuous inflammation of the colon, and Ulcerative Colitis.
Many of the medicines currently prescribed to treat UC suppress (decrease the activity of) the immune system.
Is there a cure?
There is currently no medical cure for UC. Medical treatment is available to help manage it. American hospitals experience 500,000 visits per year and 46,000 hospitalizations for Ulcerative Colitis. In severe cases, surgical removal of the colon does cure ulcerative colitis.
The Good News
New medicines are now being studied with ENCORE Research to find a cure for UC. Please call for more information, or to schedule an evaluation to see if this is an option for you.
We look forward to talking with you!
Hot flashes are sudden feelings of warmth. Your skin might redden, as if you’re blushing. Hot flashes can also cause sweating, and if you lose too much body heat, you might feel chilled afterward. Although other medical conditions can cause them, hot flashes most commonly are due to menopause. Hot flashes are the most common symptom of the menopausal transition. Frequency of hot flashes can range from a few a week to several an hour. They can be mild or severe enough to interfere with qualify of life. There are a variety of treatments for particularly bothersome hot flashes.
Symptoms
During a hot flash, you might have a sudden feeling of warmth, a flushed appearance with red blotchy skin, rapid heartbeat, perspiration, a chilled feeling as the hot flash lets up.
Causes
The cause of hot flashes isn’t known, but it’s likely related to several factors. These include changes in reproductive hormones and in your body’s thermostat, which becomes more sensitive to slight changes in body temperature.
Complications
Nighttime hot flashes (night sweats) can wake you from sleep and, over time, can cause chronic insomnia. There is some association with hot flashes and increased risk of heart disease and bone loss.
Don’t suffer in silence!
Diagnosis
Your doctor can usually diagnose hot flashes based on a description of your symptoms. Your doctor might suggest blood tests to check whether you’re in menopausal transition. Before your appointment: make a list of your symptoms, how many hot flashes you have a day and how severe they are, medications, herbs, vitamins and supplements you take, including doses, questions to ask your doctor.
Treatment
Discuss the pros and cons of various treatments with your doctor. There are prescription and non-prescription medications available. Hot flashes subside gradually for most women, even without treatment, but it can take several years for them to stop.
Lifestyle and home remedies
If your hot flashes are mild you may be able to manage them with lifestyle changes without medication. Keep cool. Dress in layers so that you can remove clothing when you feel warm. Use a fan or air conditioner. Lower the room temperature. Sip a cold drink. Watch what you eat and drink. Hot and spicy foods, caffeinated beverages, and alcohol can trigger hot flashes. Relax. Meditation; slow, deep breathing; or other stress-reducing techniques may help. Don’t smoke. Smoking is linked to increased hot flashes. as well as your risk of many serious health conditions, Lose weight. If you’re overweight or obese, losing weight might help ease your hot flashes.
Mind and body approaches
A growing body of evidence suggests that certain techniques can help ease hot flashes. Mindfulness meditation: This type of meditation has you focus on what’s happening from moment to moment. Acupuncture: Some studies indicate that acupuncture might reduce the frequency and severity of hot flashes. Hypnosis: Some research indicates that hypnosis might help relieve hot flashes. Cognitive behavioral therapy: This type of talk therapy may help you cope better with hot flashes.
Dietary supplements
People often assume that “natural” products cause no harm. However, all supplements may have potentially harmful side effects, and supplements can also interact with medications you’re taking for other medical conditions. Always review what you’re taking with your doctor.
Clinical trials
Research is underway to find new and better treatments for managing hot flashes. This may be an especially attractive option if your hot flashes are frequent and severe enough to interfere with your quality of life. Research can give you an option other that hormone therapy, for those that wish to avoid hormones.
Written by: Julia Baker, RN, CCRC
Resource: www.mayoclinic.org
A contagious virus that can cause infections in the lungs and respiratory tract.
You may have heard of the respiratory syncytial virus, in fact most people encounter RSV more than once, sometimes within the same year. Throughout older childhood and most of adulthood you may catch RSV during the winter and experience symptoms similar to the common cold. Symptoms range from mild to severe and include nasal congestion, cough, fever, wheezing, lethargy, and difficulty breathing.
What is so concerning about RSV?
It’s known that RSV shows severe symptoms in infants. However, recent studies have seen an increasing percentage of infected older adults with severe respiratory complications requiring hospitalization and occasional fatality.
I’ve had RSV before, so my immune system knows how to respond.
As we age, we encounter a natural degradation of our immune systems. While you may have encountered RSV in the past, infection after 65 years of age could entail severe respiratory complications as the immune system loses its ability to fight the virus. Studies show that RSV causes approximately 170,000 hospitalizations and around 14,000 deaths per year among older adults.
What can I do if I get infected?
There is currently no vaccine for the prevention of RSV, and because it’s a virus, antibiotics do not work. There are some treatments available, though usually pricey and used in extreme cases if you are already hospitalized.
The good news is there are several new preventative vaccines currently being developed. As an ENCORE Research community member, you have access to our cutting-edge research trials and are the first to know about new research. If you are interested in getting involved in any of our research studies, call your local office today!
Written by: Lana Borema
You may know that having normal cholesterol levels in your blood are important for helping prevent heart attacks and strokes. But you may not know that there is another factor in your blood work that can be just as important! It’s a blood test you can request, and the result will tell you if it’s important for you.
Lipoprotein(a) is a particle in your blood which carries cholesterol, fats, and proteins. The amount your body makes is inherited and determined by the time you are born. It does not change very much during your life and is not affected by diet or exercise.
Lipoprotein(a) is also known as Lp(a), L-p-a, Lipoprotein-little-a, and L-p-little-a. Some cholesterol and Lp(a) in your blood is normal. A high level of LDL, the bad cholesterol, increases your risk for heart attack or stroke. High levels of Lp(a) also increase your risk, even if your cholesterol numbers are normal! About 20 percent of people, or 1 in 5, have high levels of Lp(a). This blood test is not done as part of your usual blood testing but can be requested.
Here are some reasons an Lp(a) blood test may be important for you:
- Having high levels of LDL, even while taking medicine to treat it.
- You or a family member have had a heart attack or stroke at an early age, men younger than 55 years old and women less than 65 years old.
- You or a family member developed high blood pressure at an early age.
- A family member has high Lp(a). If an adult has high Lp(a), their children have a 1 in 2 chance of inheriting it.
- Having FH, Familial Hypercholesterolemia, an inherited condition of very high cholesterol levels.
Get tested, ask your nurse or doctor if you have questions.
- Join a clinical trial. Jacksonville Center for Clinical Research currently has an enrolling study, call 904-730-0166 for more information. If you are eligible for this study, Lp(a) testing is provided at no cost to you.
- Ask your Doctor to order the lab test. Several labs perform it:
- Cleveland Heart Lab / Quest
- HDL labs
- Boston Heart Diagnostics
Be aware of your personal risks.
Reach healthy goals for your cholesterol results with dietary choices, exercise, and medication if needed.
Stay healthy, stay active, exercise, eat naturally, have fun, love, laugh!
Written by: Julia Baker, RN, adapted from a presentation by Albert Lopez, MD
On a sailing ship in 1747, twelve sailors who had begun the voyage feeling fine were overcome with fatigue. Their gums were swollen and sore, making it difficult to eat. Their teeth were falling out. Their legs were swollen and purple from bruising.
Dr. James Lind was a passenger on that ship, and he set out to find the cause. He set up what may have been the first clinical nutrition experiment. He decided on six groups of treatments, 2 sailors in each group:
- drank one quart of cider a day
- gargled with sulfuric acid
- had two spoonfuls of vinegar, 3 times a day
- drank ½ pint seawater a day
- drank barley water
- ate two oranges and 1 lemon a day
Within six days, the sailors who ate the oranges and lemon felt better and were able to work again. The other sailors in the experiment felt worse. The ill sailors were suffering from a lack of vitamin C, now known as Scurvy. They had plenty of fresh fruits and vegetables when they first set out on the voyage. But fresh foods ran out on the long voyage, and they suffered symptoms from this lack. After this finding, sailors often brought lime juice aboard ship because it could be stored longer. This is how sailors earned the nickname “limey”.
1747 was well before the requirement of informed consent of the patient, detailed eligibility criteria, protocols and regulations, which are a foundation of today’s clinical research. Nevertheless, it is an interesting example of a method of discovering the best treatment for a disabling condition.
Scientific minds are still seeking solutions for medical problems. Modern clinical research is strictly regulated for the safety and well-being of the research volunteer. Great progress has been made in medical science over the last decades. This progress could not happen without dedicated volunteers. Participation in clinical trials can be a rewarding endeavor for both investigators and volunteers alike.
Written by: Julia Baker, RN, CCRC
Resources:
https://askabiologist.asu.edu
https://www.umass.edu/nibble/infofile/limey.html
Gastroenterology is the medical specialty concerned with the structure and function of the digestive tract (also called gastrointestinal [GI] tract). Some symptoms that can indicate disease or dysfunction of the GI tract include nausea, vomiting, weight loss, heartburn, regurgitation, abdominal pain, abdominal bloating, rectal bleeding, constipation, and diarrhea. Digestion of food and fluids is a very complex process, so persistent symptoms may require a gastroenterologist’s evaluation to determine the cause. Knowing the cause of symptoms can then lead to proper treatment and control or management.
What’s the Difference between IBS and IBD?
Irritable Bowel Syndrome (IBS)
IBS is a common GI disorder that can considerably reduce the quality of life. It affects as many as 5%-20% of individuals worldwide. It occurs more often in women than in men, and is more commonly diagnosed in patients younger than 50 years of age. Symptoms range from diarrhea to constipation, or a combination of the two. Abdominal pain or discomfort often exist alongside abdominal distension.
Diagnosis of IBS is made after obtaining a medical history, physical exam, and diagnostic testing to learn if any disease process is causing the symptoms. There is evidence to show that IBS can be a result of genetics, environment and social learning, dietary or intestinal microorganisms, low-grade inflammation and/or dysfunction of muscular movements, secretions and sensation.
Many patients with IBS ignore their symptoms, believing they are a normal part of everyday life. The good news is that with proper diagnosis, there are ways to treat or manage the symptoms. Don’t ignore persistent symptoms, there is help available.
Inflammatory Bowel Disease (IBD)
IBD is not the same as IBS, and understanding the difference is important for proper treatment. The symptoms can be the same, but the problem causing the symptoms is very different. Inflammatory bowel disease includes Crohn’s Disease (CD) and Ulcerative Colitis (UC). Crohn’s Disease can cause inflammation through the walls of the GI tract and can affect any part of the GI tract. Ulcerative Colitis commonly includes inflammation of the GI mucosa and is limited to the colon (large intestine). Recent research showed that some factors that can lead to IBD includes genetic susceptibility, environment, intestinal microorganisms, and immune responses. Medications are directed at treating the active inflammation, which can then decrease or control the symptoms.
Conclusion
Since symptoms of many GI disorders can be the same, a thorough medical history, physical exam, and proper diagnostic testing is crucial to obtaining a correct diagnosis and treatment. Open communication with your gastroenterologist and health care providers is essential to appropriate management and treatment. Be sure to tell your doctor about symptoms that concern you and new problems that arise. Do not hesitate to ask questions to ensure your understanding of your diagnosis and any treatment prescribed. Being a partner in your health care can lead to a healthier, happier life!
Written By: Julie Baker, RN
Resource: World Journal of Gastroenterology
“Pneumonia” the old man’s friend. The most frequent “sendoff” in the pre antibiotic era. In the US infectious disease remains a leading cause of death primarily due to pneumonia. Each year the bacteria Streptococcus pneumonia (pneumococcal) disease kills thousands of adults. It is spread from person to person through, coughing, sneezing and close contact. People can carry the bacteria in their throat, nose and sinuses and show no symptoms of infection and still spread the bacteria to people who do become ill. Illness can range from upper respiratory tract infections; sinus, ears and throat to much more severe disease (invasive pneumococcal disease, IPD) defined as pneumonia, blood stream infection and meningitis. There are dozens of different types of pneumococcus that vary by polysaccharides in the capsule that surrounds them.
Vaccination against pneumococcal disease started in the pediatric age group and was quickly shown to be highly effective and then introduced to the adult population with similar results. It has been proven that vaccines against pneumococcus are safe and effective and DON’T CAUSE autism. Current recommendations are that adults 65 years old should receive 2 vaccines separated by at least one year. Re-vaccination with the same vaccine is generally not recommended. PCV13 followed by PPSV23 after 1 year. The number on the vaccine tells you how many different types of pneumococcus are covered. Long term studies have shown a 75% reduction in IPD in adults after one dose of PCV13 or PPSV23 for the covered types and an overall 45% reduction against pneumococcal infections in general. Estimates for the U.S. project a vaccine related reduction of 3,000 deaths and 30,000 cases of IPD over the next 3 years.
Monitoring pneumococcal sub-types in the community allows us to produce more effective vaccines based on the sub-types identified. ENCORE Research Group is excited to participate in new pneumonia vaccine research! If you or someone you know may be interested in participating in our research, call our office to find out more!
Written By: Mitchell Rothstein, MD
What causes a heart attack?
A heart attack (myocardial infarction) means that blood flow to the heart muscle has been decreased enough to cause damage to the heart muscle. Some causes of blocked blood flow include blood clots, cholesterol build up, and rupture of plaque within the blood vessel. For those who have already suffered a heart attack, it is important to reduce the risk of recurrent attacks. Research has shown that there are several steps that can be taken to help reduce the risk of recurrent heart attacks.
Proven things you can do to prevent heart attacks
- Lower cholesterol
- Lower triglycerides
- Lower blood pressure
- Stop smoking and avoid secondhand smoke
- Eat fish
- Increase physical activity as allowed by your doctor. Inactive people have nearly twice the risk of heart disease as those who are active.
- Talk with your doctor about medicines that can decrease blood clotting
Medications that can reduce risk of heart attack
- Cholesterol lowering medication, which include statins and non-statins
- Triglyceride lowering medications
- Medications that decrease inflammation
Current research is underway to study improving health after a heart attack
- Weight loss: Heart attack is three times higher in those who are obese than in those who are lean.
- New medications for those with unique cholesterol metabolizing problems.
- Anti-inflammatory medications targeting inflammation in blood vessels.
At ENCORE Research Group we have clinical research studies for many of the risk factors mentioned above. Participating in a research study can help keep you motivated on your journey to better health. If you are interested in participating in any of our research studies, call your local office today!
Thank You for a Great Year!
As an ENCORE community member, we hope you have enjoyed hearing from us this year. Each month we strive to provide you with accurate information on health topics that are relevant to you and our enrolling studies. 2018 has been a momentous year for us and has seen complete many trials for novel medications that we believe will improve global health. We are thankful for dedicated volunteers like you that make this possible!
This month we would like to do something a little different and provide you with insight into clinical trials. A lack of clinical trial education is routinely cited as the number one barrier to enrolling trial participants. Clinical trials are required by the FDA to prove the safety and effectiveness of new medications and volunteer participants are necessary to complete these trials. We understand that this concept is often intimidating. However, there are several measures in place to make our trials as safe as possible, including:
- Physicians in charge of all study activities
- Pre-Clinical Testing
- Institutional Review Boards (IRBs)
- Informed Consent Forms
- Routine Participant Labs and Clinical Assessments
- Clinical Trial Data Safety Monitoring Boards
Investigational products are thoroughly studied during pre-clinical testing before the trials are designed and the first human participant is enrolled. Pharmaceutical companies spend millions of dollars to bring medications to market and they want to be nearly certain that the medication will fulfill its intended purpose. However, volunteers are needed to complete the FDA clinical trials. When designing the trial protocols, participant safety is always the number one priority!
Every trial is overseen by an Institutional Review Board (IRB). The purpose of the IRB is to protect the rights and welfare of human research participants. The IRB evaluates the possible risks and benefits of the trial before it is allowed to open. They are also responsible for approving the trial protocol and the informed consent. Along with the consent form, a discussion with our medical staff allows you to make an informed decision on whether or not the trial is in your best interest. Lastly, participants in the study are continuously monitored for safety and there are many tests completed during the trials to alert researchers at the first sign of potentially serious side effects. We hope that every patient that has worked with us has felt that it has been a safe and positive experience!
Thank you again for helping us improve global health and find new ways to treat medical ailments! 2019 is going to be another exciting year at ENCORE Research and we hope to get the chance to work with everyone reading this letter.
Happy Holidays,
ENCORE Research
Is GERD just heartburn, or is it something more? Check out our PowerPoint to find out the latest information and gain some tips on how to help reduce symptoms.
Researchers are continuing to study GERD and new ways to treat it. Currently, some of our ENCORE research sites have new GERD research studies enrolling. If you or someone you know has GERD, and are interested in participating, call your local office to find out more!
Click here to view the GERD powerpoint
Gluten Free. This has become a household term. Everyone has heard of gluten free diets, but not everyone comprehends why this distinction is necessary. For people with celiac disease, gluten can be devastating, and it is essential for food labeling to be correct. Celiac disease is an autoimmune disorder where the ingestion of gluten leads to damage in the small intestine. (1) Even ingesting minuscule quantities of gluten, such as crumbs from a toaster, can trigger intestinal damage. This damage can prevent the body from properly absorbing nutrients. Celiac disease is hereditary and is estimated to affect 1% of people worldwide.
There are more than 200 known symptoms of celiac disease, which can make it a nightmare to diagnose. It is estimated that there are 2.5 million undiagnosed Americans. When you mention celiac, most people think of digestive symptoms however, only around one-third of adults with the disorder experience digestive symptoms like diarrhea. Common symptoms include: fatigue, joint pain, arthritis, fatty liver, depression or anxiety, peripheral neuropathy, migraines, canker sores, and skin rash. If left untreated, Celiac disease can lead to many long-term health complications. Unfortunately, the only way to accurately diagnose celiac disease is to have an endoscopic biopsy. Once a diagnosis is made, the challenge of managing the condition begins.
Currently, the only effective treatment for celiac disease is to follow a strict gluten-free diet. However, the future is not bleak. Researchers from around the world are working to find effective pharmaceutical treatments. COUR Pharmaceuticals is researching a drug which aims to reprogram the body’s immune system to tolerate gluten subsequently reversing the signs and symptoms of Celiac disease.(2) Additionally, the Journal of Biological Chemistry notes that scientists have discovered a protein associated with celiac disease can be inactivated, paving the way for new treatment possibilities.(3)
References:
- https://celiac.org/celiac-disease/understanding-celiac-disease-2/what-is-celiac-disease/
- https://www.courpharma.com/pipeline-and-programs/
- https://www.sciencedaily.com/releases/2018/02/180223122343.htm
The heart is vital (literally), so it’s important to keep it in tip-top shape! The rest of the body depends on the heart to deliver blood and oxygen to all its cells and organs. If the heart becomes damaged, it can lead to what is known as heart failure. Keeping your heart healthy not only involves proper diet and exercise, but also involves making sure conditions that can cause heart damage are properly managed.
Some conditions that can damage the heart are:
- cardiomyopathy
- coronary artery disease
- diabetes
- heart attacks
- high blood pressure
During heart failure the heart is unable to pump blood effectively enough to meet the body’s demands. Because the heart cannot fulfill its primary duty, it will try to compensate by enlarging itself, increasing muscle mass or pumping faster. The body can also react by narrowing blood vessels and diverting blood away from less important tissues and organs. As heart failure worsens the compensations and symptoms begin to show.
Common symptoms of heart failure include: shortness of breath, fatigue, coughing, racing heart, excessive tiredness, loss of appetite, and chest pain. Risk factors for developing heart failure include diabetes, poorly controlled high blood pressure, high cholesterol, or family history of heart failure. If you think you might have symptoms of heart failure, it’s important to speak with your doctor as soon as possible.
There are about 5.7 million adults in the United States who have heart failure and it’s the leading cause of death in diabetics. In most cases, heart failure cannot be reversed once diagnosed. However, researchers are continuing to study ways to reverse heart failure as well as new and better ways to treat it. Currently, many of our ENCORE research sites have new heart failure research studies enrolling. If you or someone you know has heart failure, and are interested in participating, call our office to find out more!
Sleep is essential for the body to repair and restore itself. In fact, sleep is so important that humans spend approximately 30% of their lives sleeping. However, since the beginning of recorded time and undoubtedly before that, some people have struggled to sleep. Fortunately, over the last 50 years our understanding of how to improve and correct the body’s sleep systems has advanced tremendously. This research has led to new understanding of how people sleep and why about 30% of the US population struggles with sleep disorders such as insomnia.
Insomnia is defined as dissatisfaction with sleep quantity or quality associated with difficulty falling asleep or staying asleep, even when there is adequate sleep opportunity (7-8 hours). This can cause significant social or functional distress and impairment. The most common sleep disorder in the US is Insufficient Sleep Syndrome, in which sleep deprivation occurs from an inadequate amount of sleep. Insufficient Sleep Syndrome is voluntary, but unintentional, unlike insomnia. 1 A recent poll of US adults suggests an average sleep time of just over 6 hours which is 2 hours less than we were sleeping 100 years ago, however, our sleep need has remained constant.
In order to achieve quality sleep, many insomniacs often self-prescribe antihistamines and alcohol. These treatments often have negative short and long-term outcomes. The first recommended treatment is Cognitive Behavioral Therapy (CBT), but this involves a trained therapist as well as a significant time commitment. These aspects combined with the fact that it is not well reimbursed by insurance can make it prohibitive for many individuals. A more cost-efficient alternative can be self-directed computer-based programs. Traditional pharmaceutical sleep products (hypnotics) have focused on depressing the central nervous system directly, but these medications have limitations due to adverse effects such as hangover, amnesia, abuse liability and dependence.
To end on a positive note, new research is focusing on some different ways to treat insomnia. We are excited to be involved at two of our North Florida ENCORE Research Group offices. If you are interested in getting involved in any of our research studies, call your local office today!
- http://www.sleepeducation.org/sleep-disorders-by-category/hypersomnias/insufficient-sleep-syndrome
The liver is the second largest organ in the body. Its function is to process everything we eat or drink and filter out any harmful substances from the blood. When there is too much fat in one’s liver, the filtration process is interrupted and can become a health problem.
It is estimated that 25% of the world has Non-alcoholic Fatty Liver Disease (NAFLD), a precursor to NASH or Non-Alcoholic Steatohepatitis. NASH is associated with obesity, cardiovascular disease, type 2 diabetes and metabolic syndrome. It is now the most common liver disorder in the United States and the number one reason for liver transplants.
Starting as Fatty Liver Disease and then progressing to NASH, the buildup of fat in the liver can lead to inflammation of the liver and liver cell damage. Progression of NASH leads to fibrosis or stiffening of the liver and cirrhosis or scarring of the liver. NAFLD and NASH are both silent diseases with few symptoms even if the diseases progress to cirrhosis.
Physicians can monitor liver function blood tests as well as abdominal ultrasounds and liver Fibroscans to determine if you are at risk of developing NAFLD and NASH. However, the only way to definitely determine of you have NASH is to perform a liver biopsy.
The most common treatment for fatty liver disease is weight loss to reduce the fat in the liver. It is estimated that losing up to 3 to 5% of your body weight can help reduce the fat in the liver. Losing 10% of body weight may help reduce inflammation and even fibrosis in the liver. Currently, there are no medications which have been approved to treat fatty liver disease; however, many are in late stage development with promising results.
To learn more about current clinical trial opportunities for fatty liver disease and NASH, please contact us.
Why do our volunteers want to participate in clinical trials? Volunteers are often motivated by a combination of several reasons. Here are 6 of the top reasons to participate.
-
The potential of finding relief from their symptoms
We can’t promise relief from symptoms due to placebo and efficacy of the medication being tested. However, the Hawthorne Effect proves that patients who participate in a research trial have better outcomes than those not participating.
-
To learn more about their condition
You might argue that to learn about a condition you can just look it up on the web, and we all do that. However, often these websites can be misleading or provide the worst-case scenario results, which don’t apply to most of us. Another option is to ask your primary physician, and that is a good thing to do. Unfortunately, physicians are often rushed or running behind and questions are forgotten. Participating in a clinical trial provides you ample one on one time with a research professional and physician so that all your questions can be answered.
-
Access to new cutting-edge treatments
When participating in a clinical trial, there is access to new cutting edge treatments that are not available yet to the public. There can even be access to medications that have been newly FDA approved, but are much too expensive to afford. Study required medications are most often provided at no cost!
-
Receiving medical care at no cost
Sponsors such as pharmaceutical companies, governments and foundations fund medical research through study grants. The grants fund local research sites for conducting the study so you don’t pay a thing. In fact, we don’t even ask you for your insurance information! Can you believe most studies compensate patients for time and travel?
-
Making a difference
Clinical Trials help shape the future of medicine and healthcare. Volunteer participation helps researchers discover more about health conditions and find better ways to treat them!
-
Moral and emotional support
Having medical conditions that others don’t necessarily understand can make some people feel alienated. When involved in research, support staff understand the patient’s condition and what they may be experiencing and can provide moral and emotional support.
We will do everything we can to help find a trial that is a good fit for interested volunteers. New clinical trials are constantly enrolling so do not be discouraged if we don’t currently have the perfect trial for you. The majority of volunteers who completed a clinical trial are interested in participating in another one, so call us and find out your reason to participate!
When patients are diagnosed with an autoimmune disorder they often have many questions. How did this happen? What is happening inside me? What treatments are available? Autoimmune diseases can be extremely complex and are the subject of much current research. The immune system’s purpose is to identify and destroy threats to the body such as viruses, bacteria or parasites. However, when a person has an autoimmune disease such as Crohn’s Disease, Lupus, Sjogren’s (show-grins) syndrome the immune system becomes unable to distinguish foreign bodies from the body’s own healthy tissue. When this happens, the immune system begins to target healthy cells causing inflammation. Almost any aspect of the immune system can malfunction causing a plethora of conditions.
One such condition is Crohn’s Disease. Crohn’s is an autoimmune disease where the immune system specifically targets the gastrointestinal tract. Crohn’s can be difficult to diagnose due to the variety of symptoms associated with the disease. The symptoms vary from person to person and by which component of the GI tract is being targeted. If a doctor suspects Crohn’s Disease, diagnosis is confirmed via an upper and/or lower endoscopy. Those living with Crohn’s disease will agree that we need to find a cure ASAP!
Systemic Lupus Erythematosus(SLE) is a chronic autoimmune disease in which the immune system can cause damaging inflammation to any part of the body. Skin, joints and organs can all be affected. Flares can cause a wide variety of symptoms. Around half of those affected by lupus have what is called a butterfly rash on their face. Other common symptoms include inflammation or swelling of the joints, and fatigue.
Another inflammatory autoimmune disease is Sjogren’s Syndrome. Sjogren’s is typically identified by its most prevalent symptoms, which are dry eyes and dry mouth. These symptoms occur because the immune system targets the glands that produce saliva.1 In the past treatment has almost entirely consisted of treating the symptoms of the disease. However, new research is showing that Sjogren’s can lead to other complications and scientists are now working on specially devised treatments to nip the problem in the bud!
According to JCCR’s Steven Mathews, MD “the last generation of autoimmune treatments worked further down the mountain so to speak and focused on treating the avalanche of symptoms. Current treatments are looking at treating conditions higher up the mountain at the source and preventing the avalanche from occurring.” Richard Smith, RN elaborated that, “general immunosuppressants act like a hammer on the immune system, whereas the current drugs we are researching act like a fine scalpel only targeting the rogue immune cells.” Our mission at ENCORE Research Group has always been to help get cutting edge treatments approved by the FDA. We want to help deliver safe and effective treatments to everyone. This is only possible by conducting research studies on new investigational medications. If you are interested in taking part in one of our research studies call today.
At ENCORE Research Group it is our mission to help every patient that walks through our doors qualify for the clinical trial of their choice. Often times we get to experience the thrill of telling our patients that they successfully qualified and will soon enroll in the study. However, this is not always the case and we understand our patients’ frustration when they decide to commit to a trial only to later find out that they do not qualify. Here at ENCORE Research Group we were curious how this situation affected their thoughts about applying for future studies. This month, curiosity got the best of us and we reached out to some of our community members to find out!
Thomas recently came to Jacksonville Center for Clinical Research (JCCR) to have an evaluation for a high triglyceride and weight loss study. Fortunately for Thomas, he was not eligible for the trial because his triglyceride level was too low. Thomas stated “it’s good that I am healthy enough not to be in this research study. But they are looking at another study that I may be interested in.” As you can see, Thomas was not discouraged that he did not qualify, but optimistic that he may qualify for a different study.
We also reached out to Latasha, who is new to research, and may qualify for a study that has a waiting list for interested participants. When discussing with her how some patients are not eligible to join a trial, she stated “I would want to know why I did not qualify, but that would not prevent me from trying to get in another trial.” Fortunately for Latasha and all of our participants, ENCORE Research Group is very transparent about the screening process and explains exactly why they may have been ineligible. Hopefully she will receive a spot in the study she applied for!
Mark was passionate about participating in a Sjogren’s research trial but did not qualify. He said “it’s not unusual for someone with Sjogren’s Disease not to qualify for studies with systemic therapies if they do not have the antibodies. But when you’re sick, your driving force is to get better for yourself and your family. I tried the conventional way but it did not work for me.” After doing more research on the specific clinical trial, Mark decided to pursue the FDA Expanded Access program. “It’s a relatively new program to help people get access to new medications.” Fortunately for Mark, he had the resources and insight to look into alternative treatment options.
We also asked an experienced researcher how she saw things. Linda Gray, site manager of the Nature Coast Clinical Research site in Inverness, Florida, has many gastrointestinal (GI) studies currently enrolling. Linda acknowledges that “some of our patients are not eligible for a study because they have mild disease, and the sponsors are looking for moderate to severe disease. If the disease is not measurable enough for objective data, we will not be able to tell if we’ve reversed it or slowed the progression. Our NASH studies include a liver biopsy to determine the extent of the disease to see if the patient is eligible.” It is unfortunate that this can limit access to drugs for those in need, but we have to believe that obtaining clear and objective data will help a greater number of people in the future.
The reality is, every clinical trial is different and has unique qualifying criteria. The pharmaceutical companies that sponsor clinical trials create the criteria in order to make the strongest case possible to the FDA on the drug’s safety and efficacy. While we would love to involve every one of our community members that are interested, it is just not always possible. The good news is that all seven of our research sites are always getting new clinical trials to enroll in! So, just because you didn’t qualify the first time doesn’t mean you won’t qualify for the next one! We look forward to working with you in the ENCORE community.
As I was perusing an ancient text I came across an excerpt on the disease known as diabetes. The earliest mention of the disease I could find was by a Greek physician called Aretaeus in the first century AD. Aretaeus identified diabetes and named it after its symptoms of thirst and sweet urine. When I researched the period I was astounded to find the diagnosing physicians were called “water tasters” and would either taste the urine or see if insects were attracted to it.
My research revealed that diabetes wasn’t well understood until the 20th century. It was then that researchers discovered insulin from the pancreas helped control blood sugar levels. A few decades later in 1961 the researchers at Ames Diagnostics created the first blood sugar monitor. This monitor was called Ames Reflectance Meter and was only available in doctor’s offices and hospitals due to its cost. Around this time a pioneering man named Richard Bernstein mounted a campaign to make blood sugar monitoring at home acceptable and easy. He was so passionate about the cause, at the age of 45 he went to medical school and became an endocrinologist. His efforts here led to millions of people being able to monitor their blood sugar at home. Now information about diabetes is growing exponentially. The thought that all of this diabetes research led from tasting urine to affordable blood sugar measuring is amazing!
At ENCORE research, we are passionate about advancing health care. Without research, we wouldn’t have these advances in diabetes management!
Heart disease currently accounts for 1 in 4 deaths in the United States.[1] However due to new research breakthroughs there are now treatments available that may finally give us the means to fight back against heart disease. Historically heart disease has always been one of America’s most serious epidemics. It has been a leading cause of death since the turn of the 20th Century. Following World War II the National Heart, Lung and Blood Institute began a long term study known as the Framingham study to identify the cause of heart disease.
The Framingham study is an enormous observational study in the town of Framingham, Massachusetts. Researchers conducted physical examinations on participants every two years to study contributing factors to heart disease and are now on their 3rd generation of participants. The Framingham study identified many of the currently known risk factors such as high blood pressure and high cholesterol. Once high cholesterol was identified as a major risk factor, researchers began developing medications to combat cholesterol levels. Some of our most exciting research at Encore Research Group is for these new cholesterol lowering medications such as PCSK9 inhibitors.
PCSK9 inhibitors are an amazing class of drugs that allow us to lower LDL or “bad cholesterol” to previously unachievable levels. These drugs are usually injectable and have many advantages over traditional statin drugs. One such advantage is we are not seeing the muscle cramping associated with statin therapy. This is truly a breakthrough.
How low is too low? It is a question that researchers are actively addressing. So far we have not seen complications or health risks as a result of very low LDL. Some large studies that Encore Research has participated in will be releasing their results within the next year to more definitively answer this question. For now, there are many patients that have cholesterol levels that are difficult to budge but may respond to these new therapies.
Currently we are studying the effects of PCSK9 drugs in high risk populations such as diabetics. If you have high cholesterol levels that are not being adequately managed by your current medications, we may be able to help you get involved in a research study that may help get you back on track! As many of our readers know, most research studies offer access to medication at no cost to patients. Call us to find out how you can get involved today!
[1] CDC, NCHS. Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released 2015. Data are from the Multiple Cause of Death Files, 1999-2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed Feb. 3, 2015.
Growing up, we’ve all heard the saying, “An apple a day, keeps the doctor away” and in most cases, an apple is a great fruit to eat! However, if you have Crohn’s Disease that might not always be the case. Those afflicted with Crohn’s Disease actually have to peel the skin off of fruits and vegetables with edible skin, however delicious it may be! The skin is an insoluble fiber that can aggravate Crohn’s symptoms causing more gas, bloating, diarrhea and pain. In severe cases, can even cause blockages.
The cause of Crohn’s Disease is still unknown. Scientists believe the cause to be a mixture of environmental, and genetic factors. Crohn’s Disease causes inflammation of the wall of the gastrointestinal (GI) tract. The GI tract is continuous starting at the mouth and ending at the anus. An interesting fact about the GI tract is, it can be considered to be outside of the body. The body changes the environment of the GI tract to be conductive to digesting and absorbing food to the inside of the body. If we followed the journey of the apple discussed earlier after masticating and swallowing the apple is moved down the esophagus, and into the stomach where it will be digested. Next the apple will pass through a sphincter and into the small intestine where the nutrients from the apple will be absorbed. Crohn’s most commonly occurs in the small intestine and during a flare up it is difficult to absorb necessary nutrients before the bolus is moved to the large intestine.
While the small intestine is most commonly affected, with Crohn’s, any part of the GI tract explained above can be affected. The inflammation caused by Crohn’s produces flare ups and can lead to many uncomfortable symptoms. A few of which are: diarrhea, pain, unintentional weight loss, ulcers, malaise, anemia, and anal fissures.
Research has produced many significant advances for Crohn’s Disease, but there are still many unanswered questions. Our research sites are devoted to finding answers to those pressing questions and providing a better outlook for the future of Crohn’s health management. You can be an integral part of shaping the path for future medicine, by participating in a clinical trial.
The practice of medicine has changed in major ways in recent years. Though many of these changes reflect good intentions, the real world consequences to patients often don’t match expectations. To understand this divide between reasonable intentions and the less salubrious reality from which we may collectively suffer, I’d like to share a recent anecdote that occurred at the airport when regulations ran amok.
During recent travel, I witnessed an unfortunate incident that you may have seen before. An airline gate agent stopped a member of our party and reprimanded her for carrying a small overnight suitcase, a computer bag and her pocketbook. The gate agent, working on behalf of the airline, stated that she had to follow FAA (Federal Aviation Authority) rules and only allow two bags on board even though the computer bag and pocket book were small. Unfortunately, when asked to “consolidate” the three bags into two, we had a problem. No bag really fit into any of the other bags. The agent wouldn’t “gate check” any of the bags so that we could pick it up when exiting the plane and running off to our next flight. Further, our discussion with the gate agent failed to alleviate our concern that, if checked to its “final destination,” we wouldn’t see a checked piece of luggage any time soon given the shortness of time for our connection.
The solution that followed satisfied no one. Over the next 10 minutes, embarking passengers stepped around the contents of the three bags which littered the entrance to the Jetway. At first, the gate agents ignored the situation, but as tempers flared due to the obstruction of foot traffic, an agent “helped” by aggressively stuffing the computer bag into the overnight bag. A busted zipper later, the bulging overnight bag limped down the Jetway led by a very unhappy customer.
Does this scenario prove airline excellence because the agents showed how well they can comply with government rules? Hardly! Most folks would conclude that this messy scenario wasn’t necessary. In complex situations, the empowerment of professionals to act judiciously given a set of circumstances leads to excellence. The above scenario required the gate agents to apply context while making an overall effort to comply with government regulations. Unfortunately an excellent result didn’t happen in this case.
Similarly, we face the issue of context and judicious interpretation every day in medicine. As a common example, computerized medical records, a well-intended effort to characterize complex information, often fail to convey the true story of a patient or the nuances that make each of us unique. Summarized, bullet point information can easily miss the point. The great composer Mozart famously observed that musical excellence doesn’t lie in the notes but actually in the space and timing in between the sounds. Medical excellence involves a similar concept. Health care providers must read “in between the lines” and understand and respond both to what is and isn’t stated.
What this concept means to the average patient depends on the circumstances. For example, some people with neck pain may need consideration for a heart condition (angina) whereas others should check in immediately for an MRI of the spine and others should book a massage. Distinguishing the underlying cause of the neck pain relies on both a description of the nature of the symptom and on understanding the quiescent pauses of relief between episodes of pain. Excellent clinicians make this distinction by asking the right questions. Excellence during the medical evaluations of headaches, arthritis, and memory problems, among other things, also require this same commitment to careful questioning.
Clinical research promotes excellence by demanding great attention to detail. During research programs, physician investigators and their staff members must extensively analyze many aspects of our patients’ health. This thorough analysis usually exceeds that which occurs at the time of general physician visits, a setting during which time pressed clinicians must limit their focus and move on to the next patient. Research also requires the deployment of state of the art technology. The combination of technology and attention to detail of symptoms, signs and lab values leads to an experience which most patients highly value and describe as a demonstration of medical excellence.
In sum, medical excellence involves more than compliance or automatically matching a disease with a drug. Medical excellence is a philosophy of understanding the needs of a patient and putting those needs in context through the development of an individual treatment plan. Clinical research promotes medical excellence by demanding a culture of detail and caring.
Let’s not dance around the issue: for many years now, news sources like CBS, CNN, The Atlantic, and The New Yorker have called research volunteers guinea pigs. You’ve probably said it yourself. I’m here today to tell you why we need to call research volunteers by another name: Heroes.
The term “guinea pig” is condescending to both volunteers and researchers. For volunteers, it takes away the enormity of their contribution by sounding like they have no choice in the matter. If you have ever taken a prescription medicine for any reason, even an antibiotic; someone has chosen to volunteer to make sure the medicine is safe and works. If medicines down the road are to work better, we need volunteers to keep agreeing to test them.
Calling subjects “guinea pigs” also disdains the research coordinators and doctors that supervise drugs trials. Before any volunteer is admitted into a trial, coordinators fully explain what the trial entails, making sure to answer any questions or concerns of the volunteer. If the volunteer agrees, they go through a screening process to make sure they are a good fit for the trial and that the trial is safe for them. During the trial, the volunteer tells the coordinator or doctor about any medical events, including colds, broken toes, or headaches. This is also for safety, and if anything happens, the volunteer is free to stop the study or change their mind about participating. Throughout the study, the volunteer’s health is closely monitored; patient safety is always first. If a volunteer decides they no longer want to be in a clinical trial, they can withdraw from the trial at any time and will not be coerced to stay.
Before any medicine hits the market it is tested for years, with data constantly being reviewed in between trials. New medicines will go through 3 – 4 clinical trials over many years, with safety and effectiveness being the top concerns.
So, why are volunteers not guinea pigs? Guinea pigs (or any animal for that matter) don’t willingly sign up to be a part of future healthcare that could save lives. Guinea pigs are cute, fat, fuzzy, and they eat their own poop (Coprophagy). But, they do not willingly agree to be part of a trial that could save lives down the road.
So I urge you, quit using the term guinea pig for volunteers, use the term hero instead! We can’t cure diseases without heroes.
If you have volunteered for a clinical trial before, YOU ARE A HERO! If you have never participated, become a research HERO today!
Recently, I had my first experience as a clinical research volunteer. Going in, I wasn’t quite sure what to expect, but it was better than I thought!
I have Multiple Sclerosis. I also have asthma, arthritis, hypothyroidism, high blood pressure, and migraines. I live with chronic pain, I’ve had multiple surgeries, and the list goes on. With all these illnesses and conditions I need prescription medications to function on a daily basis.
I’m your average Google symptoms and side effects checker. I think it’s very important since I’m on over 10 daily medications to treat my health issues. I see multiple specialists; and I can’t expect them to research and remember all the ways those medicines interact with the others I’m already on. So I try to be smart about it.
Being a research volunteer has some bad stigmas attached to it. Some people think you might grow a second head or something! I’m here to tell you, don’t believe those outlandish tales! Without volunteers like me, the drugs I’m taking that stop horrible leg cramps or make my migraines back off- wouldn’t have made it to the pharmacy shelves.
When a friend of mine mentioned that her daughter works at Jacksonville Center for Clinical Research, for some reason that statement humanized the whole idea of prescription medications for me.
So I googled them and found they had SO many opportunities for many of the medical problems I currently have. I filled out an online form to be contacted, and a bubbly, friendly lady called me. I wasn’t even sure what to say but she dove right in talking about the different issues I mentioned on the form. She gave me an idea of what they were looking for in the studies, and I answered her questions. It was easy. In no time she had singled out a study I might be perfect for and set up an appointment. We talked through most of it over the telephone and she had it all together when I arrived. It turned out I WAS the perfect fit. It was a study that only required me to come to 3 appointments over a 6 week period and paid me $400. Wow! Did that extra cash come in handy! While I was there everyone treated me like an old friend.
I am doing my part to help put good drugs on the shelves for myself and millions of other people.
Now I know what it’s like to be a hero.
Tracy
Alzheimer’s disease is a degenerative brain disorder that was first described in 1906 by Dr. Alois Alzheimer. Since that time, Alzheimer’s disease has become the most common cause of dementia (accounting for 60-80% of cases). It is estimated that in 2016, 5.4 million American’s of all ages have Alzheimer’s disease. One in nine people age 65 and older has Alzheimer’s. JCCR has participated as a research center in clinical trials over the past several years to limit the devastating consequences of this difficult to treat disease.
The number of American’s with Alzheimer’s is anticipated to escalate rapidly with the aging of our population, with estimates ranging from 13.8 million to 16 million by 2050. This estimate assumes no medical breakthroughs to prevent or cure the disease.
Alzheimer’s is a slowly progressive brain disease that begins well before clinical symptoms emerge. The persistent accumulation of abnormal proteins in the brain lead to death of brain cells over time, which causes decline in cognitive function. Thus, a significant amount of protein accumulates in the brain over many years before a sufficient amount of brain injury has occurred to cause symptoms noticed by the patient or family/friends.
The medications currently approved by the U.S. Food and Drug Administration (FDA) for the treatment of Alzheimer’s temporarily improve symptoms by increasing the amount of specific neurotransmitters in the brain. However, they do not address the accumulation of abnormal proteins or brain cell injury and, thus, do not treat the underlying cause of the disease. The first medication approved by the FDA for the treatment of Alzheimer’s was donepezil in 1996. The last was memantine in 2003. There have been no new/novel treatments approved by the FDA for the treatment of Alzheimer’s since 2003. From 2002-2012, 244 drugs for Alzheimer’s were tested in clinical trials, and only one went on to receive FDA approval.
Currently, a worldwide quest is underway to find new treatments to stop, slow or even prevent Alzheimer’s. The last 10-years have seen tremendous growth in research on early detection, and researchers believe that early detection will be key in preventing, slowing and stopping the disease. There is a new wave of optimism in the scientific community about Alzheimer’s treatments.
As eloquently stated by Bill Thies, PhD, Senior Scientist in Residence with the Alzheimer’s Association: “Despite increasing momentum in Alzheimer’s research, we still have two main obstacles to overcome. First, we need volunteers for clinical trials. Volunteering to participate in a study is one of the greatest ways someone can help move Alzheimer’s research forward. Second, we need a significant increase in federal research funding. Investing in research now will cost our nation far less than the cost of care for the rising number of Americans who will be affected by Alzheimer’s in the coming decades.”
Here at JCCR, we understand the importance of recognizing cognitive decline and identifying Alzheimer’s in its early stages. Recent scientific breakthroughs provide hope that new treatments can prevent accumulation of abnormal proteins in the brain and markedly slow the disease. We want to help individuals and their healthcare providers identify the early signs of memory changes so that effective interventions can be initiated promptly. We want to help individuals maintain their memory function and their independence. We also want to facilitate participation in clinical trials that will help our understanding of memory disorders and lead to treatments that will help maintain memory function. We look forward to working with you and your healthcare providers.
Erin G. Doty, MD
Neurologist, Board Certified
Memory issues occur commonly and when they begin, one may worry about the onset of Alzheimer’s disease. While Alzheimer’s may cause memory loss, memory loss is also a symptom of many reversible conditions. Early memory testing is crucial to determine the cause of memory loss to help reverse it before it becomes permanent.
For example, certain over-the-counter medications have been associated with dementia. A recent study came out this month linking Benadryl to dementia. Benadryl has many uses, including allergy symptom relief. The active ingredient in Benadryl is diphenhydramine. This drug blocks the action of acetylcholine (anticholinergic effect) and is used as a sedative because it causes drowsiness. 1 Diphenhydramine is used in most over-the-counter sleeping pills, for motion sickness, and other allergy medications.
A study completed in 2015 at the University of Washington showed the longer and more consistently people took anticholinergics, the more likely they were to develop dementia. Other drugs that contain anticholinergics are used to treat diseases like asthma, incontinence, gastrointestinal cramps, and muscular spasms. They are also prescribed for depression and sleep disorders. 2
While we do not fully understand dementia, we do know that the neurotransmitter acetylcholine is important in brain processing and memory. We know that the acteylcholinesterase inhibitors (drugs like Aricept (donepezil), Exelon (rivastigmine) and Razadyne (galantamine) which inhibit the breakdown of acetylcholine, do provide symptomatic improvement in affected patients.
It would seem that taking a combination of acetylcholinesterase (cholinergic) with an anticholinergic drug (such as Benadryl) is probably not a good idea. In fact a recent study showed 16% of Alzheimer’s patients living independently were doing just that.
This 2015 study is backed up by another study that came out this month offering the most definitive proof yet, that anticholinergic drugs are linked with cognitive impairment and increased risk of dementia. Using brain imaging they found that patients taking anticholinergic drugs indeed had lower metabolisms and reduced brain sizes.
The bottom line is that given all the research evidence, you should be aware that these over-the-counter medicines may reduce the effectiveness of your prescription medicines. If you or a loved is worried about memory loss, the first step is to get tested to see if it’s from a treatable or reversible cause. Jacksonville Center for Clinical Research offers a professional memory screening for no cost to you. Make an appointment today to help put your mind at ease.
1- https://www.medicinenet.com
2- https://www.healthline.com
Incredibly, migraines are the third most prevalent disease, and the sixth most disabling disease in the world. In the US alone, 18% of women, 6 % of men, and 10 % of children experience migraines. It comes as no surprise that 1 in 4 US households include a migraine sufferer.
Why are migraines a big deal? Unlike normal episodic headaches, migraines are a chronic disease that significantly diminish quality of life. Migraines can be excruciatingly painful, debilitating, and often incapacitating for hours or even days.
Migraines have four stages: prodrome, aura, headache, and post-drome, though you may not experience all stages. Prodrome is usually one or two days prior to a migraine, you may notice changes or sensitivities that warn of an impending migraine such as: constipation, mood changes, food cravings, neck stiffness, frequent yawning, and increased thirst and urination. Auras are symptoms of the nervous system, typically visual disturbances, however they can also be sensory, motor, or verbal disturbances. Luckily, most people have migraines without aura. During the Headache attack you may experience a throbbing or pulsing pain on one or both sides of your head. Extreme sensitivity to light, sounds, smells, or touch. These can be accompanied by nausea and vomiting, blurred vision and lightheadedness. Post-drome is the final phase which lasts for about 24 hours after the headache attack. During post-drome you may feel drained, confused, moody and weak.
Once thought of as a psychological disorder, migraines are now considered a chronic neurological disease with many triggers. A trigger sets off events that excite a nerve which releases a variety of neurochemicals and causes cranial blood vessels to swell and inflame.
You’ve probably already heard about the many possible migraine triggers, but maybe you’re not quite able to nail down what’s triggering your migraines. Consider the overload of information your brain consumes daily: everything from social media, to millions of breaking news stories. Your brain literally can’t get a break from the constant intake of new information. This increase of information causes stress on the brain, which can reach an overload point and shut down the prefrontal cortex; thus triggering a migraine.
What should you do if you are experiencing migraines? The best thing to do is see your doctor. Why? If you are having true migraines, over the counter medications usually just don’t work, and taking them for migraines several times a month can lead to overuse. This will almost certainly cause rebound headaches! It’s a vicious cycle; don’t get stuck in it! Your doctor can help you figure out the right treatment for you.
Fortunately for migraine sufferers there is a bright future ahead, and I don’t mean in a bright light during a migraine attack kind of way. Clinical trials are showing promising results for new migraine treatments. You can be part of the future of migraine treatments by volunteering for a migraine clinical trial! Call today to get involved! As always, there is no cost, and no health insurance required.
Many doctors prescribe metformin to diabetic patients. Doctors trust the drug, particularly since the landmark United Kingdom Prospective Study that showed that overweight Type 2 diabetics on metformin lived longer and suffered fewer heart attacks than those with the same blood glucose levels achieved using insulin. The history of metformin provides a good example of how an unusual herb can become a powerful treatment.
Metformin originates from the plant Galega officinalis or French lilac, goat’s plant or goat’s rue. This plant was fed to goats to improve milk production. It grows as a perennial herb, 3 feet tall, with purple, blue or white flowers and was used in the Middle Ages to treat frequent urination, a side effect of diabetes. The Native American Seminole tribe used the insecticide roterone, found in the roots of Galega officinalis, in fishing. Fish were stunned by roterone, and were much easier to catch. This plant has powerful properties and is now widely considered poisonous.
Metformin was first described by scientists in 1920. Chemists found that they could make the active compound from this plant, guanidine, more tolerable to be ingested by bonding two guanidines together forming a biguanide. This compound, which could lower blood sugar, was first synthesized in 1929. However, insulin had also been discovered during this time and became the more popular option for controlling blood sugar. Metformin was neglected and ignored until 1950 when metformin was used to treat influenza. Doctors noted metformin decreased glucose levels.
In 1958, Metformin was finally released in the United Kingdom as a treatment of lowering blood sugars. This drug was clinically developed and called Glucophage (“glucose eater”). Glucophage was released in the United States in 1995 and quickly became a popular medicine. Finally after half a century, it’s potential was realized. Metformin has now become the world’s most widely prescribed anti-diabetic agent and is universally recommended as the first therapy for Type 2 diabetes.
Metformin works by lowering the rate of hepatic glucose production, which is three times higher in people with Type 2 diabetes. Probably through reduction of insulin resistance, metformin can reduce cardiac risk factors and may decrease cardiac events. Since metformin does not cause hypoglycemia (low blood sugar), it can be safely utilized in a variety of diseases such as pre-diabetes, gestational diabetes, polycystic ovary disease, sleep apnea, osteoporosis and cancers.
Metformin’s has also been noted to have a positive effect on longevity due to its anti-cancer effect. Since having Type 2 diabetes is a major risk for developing cancer (pancreas, bladder, ovary, breast, prostate, colon and liver) patients with Type 2 diabetes have a lower risk of developing these cancers if they are utilizing metformin.
This very economical and widely available medication has been shown to safely treat multiple diseases in addition to Type 2 diabetes and to improve longevity in both the diabetic and non-diabetic patient. Metformin has come a long way from its humble “roots”. Fortunately, research rediscovered this powerful perennial herb. And now metformin has ascended to being the drug of first choice for patients with Type 2 diabetes.
The word “tsunami” describes a huge wave caused by an underground disturbance. Diabetes falls under that definition in our view. According to a study in Diabetes and Endocrinology, two out of five American adults may develop Type II Diabetes in their lifetime. About 95% of US diabetics are Type II. Type II diabetes occurs due to a condition of insulin resistance. Insulin, a hormone produced in the pancreas, does not have a sufficient effect on blood sugar levels, despite high levels of production in Type II diabetics. Fortunately, thanks to clinical research, surviving this diabetic tsunami should soon become easier. New research breakthroughs may lead diabetes to “dry land.”
For those currently battling diabetes, recent technological breakthroughs may make pricking your finger a thing of the past! Researchers at Arizona State University developed a method of testing glucose through saliva. To use, one simply licks a biosensor strip. The biosensing device then uses an electrochemical analysis to calculate blood glucose levels instantly. The company overseeing the development of this technology hopes to have it on the market in the next few years.
While tracking your blood sugar should become simpler, new ways of taking your diabetes medication may help keep diabetics afloat. Scientists have developed a “smart patch” that contains live pancreatic beta cells. A “smart patch” uses a system of tiny needles – each about the size of an eyelash, to detect high blood glucose levels and automatically inject insulin when needed. The live beta cells used in the newest versions of the smart patch can control rising blood glucose levels for roughly 10 hours at a time. Since the beta cells stay outside of the body on the patch, one’s body should not reject the cells. Current testing has been successful in mice studies, but the patch has yet to be tested on humans. Maybe one day we will seek volunteers for the “smart patch” at all of our seven research sites!
Another interesting diabetes finding comes from researchers at the Ottawa Hospital. Scientists turned from puzzled to amazed when they discovered a bacteria-killing protein in the pancreas. The bacterial-killing protein called cathelicidin antimicrobial peptide (CAMP) is produced by the same cells that produce insulin. Hoping to find a link between CAMP and diabetes, they injected diabetes-prone rats with CAMP. Not only did the rats have a healthier, more regenerated pancreas, but they had an increase in beneficial gut bacteria. CAMP could be a breakthrough in diabetes treatment.
Having diabetes is a big deal, and high sugar levels are themselves often less of a risk than other associated features of diabetes. In fact complications, such as high cholesterol levels and weight gain can be more problematic. High levels of cholesterol increase your risk of having a heart attack or stroke. Weight gain leads to higher blood sugar levels, high blood pressure and arthritis in weight bearing joints. We have several studies which target these complications. Many studies targeting cholesterol are enrolling right now at any of our sites, so if you have diabetes, heart disease, or even just high cholesterol give us a call and we can find the right fit for you! We also have a diabetes study enrolling with a medication that is said to cause weight loss at our Fleming Island, St. Johns, and Inverness offices. The future of diabetes management is looking bright! These research studies and new technologies coming down the pipeline may be just the life raft you’ll need to stay afloat in the diabetic tsunami.
As each year comes and goes we seem to go through the same cycle. We end the year by reflecting on what we accomplished (or didn’t) over the course of the past year and how we can improve over the next year. Many of us set specific goals which we call our ‘New Year’s Resolutions’. These goals range from budgeting to personal growth to accomplishing a specific task. One topic we all seem to consider though is improving our own health. One person may try a new fad diet and another may set a goal to start exercising once a week. One thing most people don’t consider is participating in a clinical trial.
Why would you make participating in a clinical trial part of your New Year’s Resolution? There are many reasons that participating in a clinical trial can improve your health. In the very least people should consider participating due to the Hawthorne effect. Patients receiving individual care in a trial tend to do better than those not in a trial regardless of whether or not they receive placebo. Also, patients may improve their health by receiving new medications or feeling more compelled to take their medications regularly. The many beneficial effects of participating in a trial can combine to make a real difference!
Here at ENCORE we are thankful for the patients that have put their trust in us over the past year. Our patients make us who we are and are an integral part of the ENCORE family. Moving forward into 2017 our New Year’s Resolution is to give our patients their best experience with us yet! Our goal is to help you with your health goals. If there is something we can help you with then we would love to go on that journey with you. Happy New Year!
Written by: Dr. Jeff Jacqmein
As we are beginning to prepare for vaccine season here at ENCORE Research now is a great time to inform you of some of the recent advancements in the field. There are many vaccines in the pipeline (1) and with volunteers like you we look forward to helping bring them to market. I have selected four major developments to share with you that demonstrate how the field is evolving and the technology is improving.
Recently there has been major concern worldwide about the spread of Zika virus, which is especially worrisome to pregnant patients. The National Institutes of Health is using a piece of DNA with genes that code for Zika, but are not infective to create a new vaccine. When the vaccine is injected into the arm muscle, the body reads the genes and creates virus-like particles which the body then thinks is an infection and then mounts a complete and lasting immune response. However, this is not the only way DNA is being used in vaccine creation.
DNA cloning has transformed the vaccine development process to shorten the average vaccine approval time while increasing safety. Previously, vaccine approval took 10-15 years to progress from laboratory development to clinical trials. Researchers can now genetically engineer cows or rabbits with human DNA to gather more accurate information on safety, efficacy and potency of vaccines in pre-clinical trials. This is important because it results in a safer and more effective product reaching patients in clinical trials sooner.
Pertaining to vaccine efficacy is the third advancement I would like to share with you, which is development of new vaccine adjuvants. Adjuvants are added to a vaccine to help the recipient create a stronger and longer-lasting immune response. According to a recent article in Immune Network, there are six new classes of vaccine adjuvants in clinical development. These developments are critically important because although recent vaccines are safer, they tend to provoke a weaker immune response when compared to past inoculations for smallpox and polio. An example of this is many older people requiring a Herpes Zoster booster vaccine to prevent shingles.
Lastly, is the invention of Nanopatch technology. Historically, vaccines needed to be stored frozen or refrigerated until just prior to dosing. This requirement significantly limited vaccine distribution, especially in remote locations. Nanopatch technology, does not have the same temperature requirement making it more practical for helping end diseases in countries where refrigeration is not readily available. The skin vaccination patch contains thousands of vaccine-coated microprojections that penetrate the skin and deliver the vaccine into localized immune cells. This technology could revolutionize the field!
Although we have more tools than ever, clinical scientific progress would be stunted without you, our volunteers. While it may be in self-interest to enroll in a vaccine trial aimed at keeping your cancer in remission (2), it is an act of service to your fellow man to dedicate yourself to a typical vaccine clinical trial. Because of you, we helped to bring the meningitis B vaccine to market within two years of major college campus outbreaks (3). It is recognized that adults who receive successful vaccines help prevent the spread of contagious disease and ultimately protect those who cannot be immunized for health or other reasons. I regularly appreciate our volunteers when I am able to prescribe an FDA-approved vaccine to a private practice patient. It is truly rewarding to work together to help prevent disease.
Dr. Dan here; this month of June I am leaving my desk and going out in the field to work as a volunteer physician on several different islands. First, I will be travelling to the Republic of Vanuatu, located in the South Pacific. Luckily for me the last recorded case of cannibalism in Vanuatu occurred in 1969, so that should not be a problem! Unfortunately, mosquito borne diseases are still an endemic. Malaria is present on all the islands of Vanuatu, but fortunately for visitors there are medications for prevention and treatment.
Another mosquito borne disease is dengue which causes as many as 400 million infections per year worldwide. A “bone-crushingly” painful flu-like disease, dengue can be fatal in severe forms, especially among children. At present there is no approved vaccine in the United States. Thankfully just last year the first dengue fever vaccine got the green light in 3 countries: Mexico, the Philippines and Brazil.
More than 1.4 million cases of dengue were reported in Brazil alone in 2015. Sanofi saw the need and developed a vaccine with the help of the Jacksonville Center for Clinical Research. We enrolled multiple patients in this vaccine study here in Jacksonville. Many of you may remember taking part in this clinical trial.
Sanofi’s vaccine is designed to coax the body’s immune system into making antibodies against all four forms of dengue. It is a live virus comprised of an attenuated yellow fever virus (yellow fever and dengue viruses have the same genus). For the vaccine, however, the virus is genetically engineered to include genes encoding for dengue proteins. Other dengue vaccines are also in development but none have received approval.
It is not a perfect vaccine; in clinical trials it only reduced the chances of developing the disease by about 60 percent. From the U.S. perspective it remains unclear how a vaccine would be used domestically, whether it would be used in areas that have already seen dengue including Hawaii or Florida or perhaps among those traveling to dengue endemic countries. The Food and Drug Administration is currently reviewing the application for the approval of the vaccine in the United States. Until the vaccine is available I will need to wear a lot of DEET and long sleeves on my travels.
I am proud of the work done here at JCCR and I want you to know that when you volunteer for these vaccine studies, your contributions have worldwide effects. Hopefully you will consider being a part of our next vaccine study to help combat the deadly disease of meningitis. Contact our Jacksonville, St. Johns, or Westside office to learn more about the meningitis vaccine trial.
Three New Breakthroughs in Heart Disease
Heart Disease is a general term for heart conditions that negatively impact the heart’s ability to perform its vital functions. On average 1 in 4 American deaths each year are due to heart disease. Fortunately, each year new discoveries are made that allow us to treat heart disease more successfully. Here are three of the latest discoveries.
- Dialysis for Heart Failure?
One of the symptoms of heart failure is fluid retention, which can lead to kidney
problems. Diuretics are currently the standard treatment for fluid retention, however there is a new treatment where a catheter in inserted through the neck so that it surrounds a major lymphatic vessel. The excess fluid is removed from the lymphatic system and then pumped back into the circulatory system where it is removed by the kidneys. This new treatment avoids some of the negative side effects of oral diuretics such as low blood pressure and decreased kidney function.
2. Beta Blockers: Old dog, new tricks?
A new study at York University in Toronto has analyzed the effect of beta blockers on
coronary gene expression in patients with heart failure. Researchers found that beta blockers “largely reverse the pathological pattern of gene expression observed in heart failure.” More research is needed to determine whether beta blockers can be used to protect against heart failure.
3. Tick saliva saving lives?
While ticks are often the subject of nightmares researchers now believe they can lead to a dream solution for myocarditis, heart attack and stroke. Ticks use proteins called ‘evasins’ to escape their host’s detection by blocking the host’s inflammatory response. Researchers are now isolating these evasins in a ‘bug to drug’ formula. Hopefully these drugs will be able treat a variety of inflammatory diseases.
At ENCORE Research Group we conduct cutting edge research similar to those seen above. While we do not have any ‘bug to drug’ studies at this time, we do have a heart failure study involving a new use for an already FDA approved medication. If you are interested in learning more about our current studies visit our “Enrolling Studies” tab at the top of the page.
Hot flashes and night sweats, medically known as vasomotor symptoms (VMS), are the most commonly reported menopausal symptom. A hot flash is “characterized by a sudden increase of blood flow, often to the face, neck, and chest, that causes the sensation of extreme heat and profuse sweating.” 1 Hot flashes are currently being studied around the world to better understand them. The great news for women struggling to deal with them is that answers are being found! Studies have already helped to clarify possible causes, what may trigger them, how they may relate to other health problems, how they affect quality of life, and what can be done to decrease them.
In a clinical trial of more than 3,000 midlife women, 60-80% experienced hot flashes at some point during the transition to menopause. During menopause, hormone levels fluctuate in the body, which has been shown to be associated with hot flashes. Interestingly, scientists have found that even though all women have hormone changes during their menopause years, not all women have hot flashes. Therefore, other factors must be involved, and further studies are needed.
Research has found that symptomatic women have small changes in core body temperature. This is believed to trigger the body’s mechanisms to cool the body, resulting in sweating and hot flashes. However, the promise of understanding and relieving hot flashes lies in continued research.
Women with hot flashes may be able to participate in helping to find answers which can lead to better treatments. To learn more about current clinical trial opportunities for Hot Flashes, and other conditions please contact our office.
Sources:
- http://www.obgyn.net/menopause/managing-menopause-part-1-vasomotor-symptoms
- NIH.gov
Writen by: Mike Mass, MD
Rheumatoid arthritis (RA) is an autoimmune disease that is localized in the joints but may also result in serious systemic symptoms. In the joints, RA begins in the lining tissue known as synovium. In RA inflammatory cells are stimulated in the synovium and release substances that will both activate other inflammatory cells and cause direct breakdown in the adjacent bone. If this inflammatory process is not interrupted it will immediately cause severe damage to the joint and, on occasion, other organs in the body.
Until recently, the only treatments available helped the symptoms of inflammation, such as pain and tenderness, but did little to stop the destructive process. The first drug that had some limited benefit was gold salts, but it was toxic and had to be monitored carefully. Low doses of a cancer drug (Methotrexate) were tried and proved effective in treating the symptoms of inflammation and also slowed down the destructive process in many patients and was a mainstay of therapy until the last decade.
As the understanding of the autoimmune abnormality increased, various substances released from inflammatory cells were identified. Initially, the most promising of these was known as tumor necrosis factor (TNF). While in other studies it had affected some tumor growth, it was also found to be a major cause of damage in RA. A group of anti-TNF monoclonal antibodies is on the market and has proven to be quite effective in a large number of patients. The search has continued for other substances that will either modify the autoimmune response or inactivate substances that cause damaging inflammation. Recently another protein has been identified that is present in the synovium and when activated will initiate a whole range of responses that result in a proliferation of synovial cells which then go on to damage the joint. This particular substance is part of a larger group of proteins known as “Integrins.” It is hoped that by giving a monoclonal antibody directed against the particular integrin a major portion of damaging inflammation will be shut down. A clinical trial of this antibody just opened at Jacksonville Center for Clinical Research University Blvd. Office and we are currently seeking volunteers. Call today to see if you qualify! 904-730-0166
If you have high cholesterol you may dread going to your doctor, especially if they are going to complete a cholesterol blood test. You know they prescribed a statin, but the muscle cramping you experience after taking it just isn’t worth it. How do you tell your doctor that the medication they prescribed just isn’t working for you? You are not alone, and there are options available for you.
We all know that having excess cholesterol in our blood is a bad thing, but why is it so bad? High cholesterol has often been called ‘The Silent Killer’. In fact, according to the CDC heart disease is responsible for 1 in 4 American deaths every year.[1] High cholesterol is known to cause plaque formation in arteries, constricting blood flow to vital organs in your body. Even worse, cholesterol plaques can become dislodged from the walls of the arteries potentially causing blood clots. Both heart attacks and strokes can be caused by plaques reaching the heart or brain respectively. If lifestyle changes such as a good diet and exercise can’t bring down your cholesterol numbers, you may need a medication. The most common cholesterol lowering medications to date are statins such as Crestor, Lipitor, or Zocor. These medicines have been life saving for many people that can tolerate them. However, some people are intolerant to statins and will experience side effects such as painful muscle cramps, inflammation and more.
If you are allergic to or can’t handle statins what can you do? It is crucial to keep your cholesterol levels down, lowering your risk for a heart attack and stroke. You may try one of the medications already on the market for people with statin intolerance such as Zetia, Juxtapid and Repatha. However, each of these drugs have their own risks. Zetia can cause symptoms similar to those caused by statins. Juxtapid, a newer medication, has been found to significantly reduce LDL bad cholesterol by 40-50%. Sadly, it also caused diarrhea, nausea, vomiting or abdominal pain in 28% of patients.[2] In 2015 the FDA approved Repatha, a new class of drug called a PCSK9 inhibitor that is very successful in lowering LDL. Unfortunately, due to the cost of development and production the annual cost is around $14,000 dollars making it unaffordable for most people.
If you’ve had trouble taking statins in the past you may be asking “what do I do now”? Many of our participants are looking for alternative treatments or want to be part of cutting edge research. I encourage you to check out the cholesterol research studies we are conducting at many of our research centers. You may qualify for a new oral medication or to receive PCSK9 in an upcoming study! The medicines being researched for people who cannot take statins may significantly alter the future of cardiovascular disease. We need your help to bring these new medications to market!
References:
[1] “Heart Disease Fact Sheet.” Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 16 June 2016. Web. 27 Apr. 2017.
[2] Orrange, Sharon, MD. “Finally, a Non-Statin Cholesterol Medication That Works: Introducing Juxtapid.” The GoodRx Prescription Savings Blog. N.p., 06 June 2014. Web. 27 Apr. 2017.
Medical progress has made the lives of folks with autoimmune conditions such as psoriasis and psoriatic arthritis (PsA) better than ever before. These conditions have been extremely difficult to treat successfully in the past. Now thanks to advancements in medicine using biological agents more people are living free of psoriasis and PsA flare ups.
Psoriasis is most commonly known for the raised, white or greyish patches that appear on the skin. These patches can progress to thick, scale-like plaques which may harden and become cracked. The severity of psoriasis is measured both by how much psoriasis a person has on their body and how much it affects their quality of life. For example, psoriasis can have a serious impact on one’s daily activities even if it involves a small area, such as the palms of the hands or soles of the feet.
Psoriatic arthritis is an inflammatory form of arthritis affecting the joints and is often accompanied by skin psoriasis. Early diagnosis and treatment of PsA can help prevent or limit extensive joint damage that occurs in later stages of the disease. Symptoms are similar to the discomfort associated with osteoarthritis (OA). One way to tell the two conditions apart is determining whether the arthritis is symmetrical or not. PsA usually affects major joints of the body symmetrically, while OA commonly affects one particular joint such as the left knee or right hip. An accurate diagnosis may require x-rays and blood tests. Once diagnosed an effective treatment plan may begin.
In the past, doctors could only treat psoriasis topically and with limited success. In the 1950’s researchers discovered methotrexate, an immune suppressant, and in the 1970’s it was approved for use in patients not responding to topical treatments. This medication and others like it are still used today, however there can be many possible side effects when suppressing the immune system. Through many years of research and clinical trials, researchers have now discovered biologics. Biologics are genetically-engineered human or animal based proteins designed to target the specific inflammatory pathways caused by psoriasis and PsA. Because of the large molecule size and complexity of biologics, they must be injected in order to be absorbed. Fortunately, injections are only needed once a month or every several months to be effective in most cases. There are several biologics currently FDA approved, however because of the recent discovery and high production costs, biologics can be extremely expensive through insurance.
At Encore Research Group, we are currently investigating many new and exciting biologic drugs for psoriasis and psoriatic arthritis. We are actively looking for qualified participants in North East Florida. Research provides participants with many great benefits. Some advantages of participating in a study include cutting-edge therapies, study-related medication at no cost and a stipend for time and travel. If you are interested in learning more about research, or our current studies please visit our website for more information. Without participants today, there won’t be new medications tomorrow!
Changes in mood are very common after childbirth. In fact, many new moms experience what is often called the baby blues, which can include mood swings, crying episodes, difficulty sleeping and anxiety. Baby blues usually only lasts up to a few weeks. However, feeling intensely depressed, overwhelmed, or anxious, could be something called postpartum depression, or PPD.
Postpartum Depression is a type of depression that can occur both during and after childbirth. It can consist of both major and minor depressive episodes and is thought to be caused by a combination of hormonal changes and fatigue due to pregnancy. Common symptoms include: feelings of sadness, hopelessness, loss of interest or pleasure, agitation or anxiety. PPD is one of the most common medical complications during pregnancy and the postpartum period. “According to the Centers for Disease Control, 11 to 20% of women who give birth each year have postpartum depression symptoms. If you settled on an average of 15% of four million live births in the US annually, this would mean approximately 600,000 women get PPD each year in the United States alone.” 1
In 58% of the women who develop PPD, the onset begins prior to delivery, with the remaining starting within 4 months of delivery. There are multiple risk factors for PPD, the most common include: a past history of depression, stress, poor social and financial support, young age, and single marital status. It is important to identify pregnant and postpartum women with depression because untreated PPD and other mood disorders can have devastating effects on women, babies, and families. Each expectant mother should be aware of the risks of PPD and should be proactive in procuring help. There are several screening tools used now by most obstetricians and hospitals on a routine basis in order to identify women with depression symptoms.
If diagnosed with PPD, there are multiple treatment options available including psychological therapy, pharmaceutical therapy or a combination of both. Presently, the pharmaceutical treatments on the market consist of either tricyclic antidepressants and/or selective serotonin reuptake inhibitors (SSRIs) such as Fluoxetine or Sertraline. We are now researching new ways to treat PPD with the hormones allopregnanolone and ganaxolone. Allopregnanolone is the neurosteroid metabolite of progesterone and is thought to play a major role in returning the body to equilibrium after trauma. Ganaxolone is the synthetic equivalent of allopregnanolone. Hopefully, these new medications will become the next golden standard to PPD care.
We are starting two new clinical trials for Postpartum Depression (PPD) with these hormones at our Jacksonville location. If you know an expectant mother or someone experiencing PPD please have them call (904)730-0166 to learn more about our clinical trial opportunities. If you live near our Nature Coast offices, please talk with your doctor and visit clinicaltrials.gov for clinical trials near you.
1: https://postpartumprogress.org/the-facts-about-postpartum-depression/
Ask anyone who has had a Clostridium difficile (C. difficile, or C. diff) infection and they will probably tell you that it was one of the worst experiences of their life. Imagine the worst flu you’ve ever had but on steroids! C. diff is affectionately referred to as “deadly diarrhea” and with symptoms such as watery diarrhea 10 to 15 times a day that’s no joke! It can also come with a multitude of other symptoms such as: severe abdominal pain/cramping, rapid heart rate, fever, blood or pus in the stool, nausea, dehydration, and kidney failure.
What is C. Diff?
C. diff is one of the many different types of bacteria that lives in our intestines. It may sound gross but bacteria in your intestines are completely normal and you need a good balance of them to remain healthy. When something such as antibiotic use throws off the balance in your intestines C. diff may start to grow out of control and begin release toxins that attack the lining of the intestines which leads to that deadly diarrhea.
Is C. Diff contagious?
C. diff is contagious, so even if you were not recently on antibiotics, you can still catch C. diff by contact with a contaminated surface. Spores from C. diff bacteria come from human feces, soil, water and animal feces. These spores can also live for weeks or months outside the body.
Who is at risk?
C. diff is most often associated with doctor or healthcare facility visits or recent antibiotic use. There is a higher risk for adults ages 50 and over, especially those that have frequent doctor visits or have had any type of recent surgery or a hospitalization.
What can you do to lower your risk?
Good handwashing practices, especially after doctor or healthcare facility visits are a great start to lowering your risk of getting a C. diff infection. Another way is to take probiotics daily anytime you take an antibiotic. The reason for this is because when you take an antibiotic it not only kills off the bad bacteria, but it also kills off the good bacteria, giving C. diff a chance to thrive. Taking a probiotic, even if it’s just store bought yogurt, helps feed and rebalance your good gut bacteria. These are not fool proof, but they may help.
A Vaccine to prevent C. Diff?
While Handwashing and probiotics are certainly a must, researchers agree they are still not enough when it comes to preventing this life-threatening infection. Which is why we are involved in a cutting-edge research study working on the development of a new vaccine for C. diff prevention. If you are interested in volunteering, this study is for people ages 50 and up who have been recently hospitalized, have an upcoming surgery, or have frequent healthcare contact. If you are not sure if you qualify, please give our office a call or click below on the site that is closest to your location to sign up and we will be glad to answer any questions!
Fleming Island Center for Clinical Research
904-621-0390
Jacksonville Center for Clinical Research
904-730-0166
Joint pain is an ancient disease. Dinosaur skeletons, cavemen remains, and ancient Egyptian mummies all have evidence of it. In 1886 an English doctor named John Kent Spender coined the term “osteoarthritis” (OA) which led to the modern understanding of the disease.
To relieve the pain and suffering of OA, ancient healers tried various concoctions, some of which persist until today. . More than 2500 years ago, Egyptian physicians treated OA with ointments containing fat, oil, honey or bone marrow, often added to various dry ingredients such as: flour, baking soda, cumin and incense. 1 The father of medicine, Hippocrates, observed that “Swelling and joint pain, ulcers, those of a gouty nature and muscle strain are usually improved by cold water, which reduces swelling and eliminates the pain, as a moderate degree of numbness eliminates pain”. Another Greek physician named Dioscorides floated a less enduring idea. He recommended using ivy. This treatment proved less effective although the subsequent itching may have distracted patients from thinking about their joints.
Acupuncture, an effective therapy for some folks, is another ancient treatment that has remained virtually unchanged over many years. An older medicinal approach using willow bark leaves remains in use today. These leaves contain salicylic acid. An understanding of the benefits of salicyclic acid ultimately led to a breakthrough by a French chemist named, Charles Frederic Gerhardt. Gerhardt’s claim to fame involved the chemically synthesize of Aspirin or acetylsalicylic acid in 1897 that improved upon salicylic acid.
In more recent years, clinical research has helped to shed some light on this painful disease. Though there is no cure for OA, researchers have found many treatments to manage symptoms. Science has proven that physical activity is one of the most beneficial ways to manage OA. The CDC recommends exercises such as: brisk walking, bicycling, swimming and muscle strengthening activities. It’s important for you to get moving and keep moving! Losing weight can also help relieve additional stress on your weight bearing joints.
If older therapies haven’t worked for you or someone you know, there is always the promises of modern medicine. Thanks to years of clinical research there are some great medications available both over-the-counter and by prescription. Analgesics such as Tylenol, opioids (narcotics) and tramadol are pain relievers. Nonsteroidal anti-inflammatory drugs (NSAIDs) are the most common anti-inflammation medication. NSAIDs include: aspirin, ibuprofen, naproxen, and Celebrex. Corticosteroids are powerful anti-inflammatory medicines most notably given by injection in a doctor’s office. Hyaluronic acid naturally occurs in joint fluid, acting as a shock absorber and lubricant. Hyaluronic acid is given by injection in a doctor’s office.2 We don’t suggest using any treatments without first checking with your doctor!
The future for OA treatments looks bright. You can participate in the path to the future by participating in a clinical trial. We have many programs available at no charge. Please give us a call so we can see which program works best for you!
Familial Chylomicronemia Syndrome (FCS) is a rare genetic disorder characterized by the build-up of chylomicrons, which are rich in triglycerides, a type of fat in your blood. The human body naturally produces an enzyme to eliminate the chylomicrons called lipoprotein lipase (LPL). However, people with FCS either do not have the LPL enzyme or it does not function properly. Due to the buildup of chylomicrons and very high triglycerides, they live at risk of severe recurrent abdominal pain and potentially fatal pancreatitis, as well as decreased quality of life in many areas.
To this day, there is no treatment for FCS; the current medications used for lowering triglyceride levels do not work for people with FCS since they are designed to work on the LPL enzyme. Currently, the only option is to follow an ultra-low or no fat diet, which is very difficult to maintain long term. People with FCS also must avoid alcohol, sweets, and simple carbohydrates due to their effect on raising triglycerides.
Lori Alexander is Director of the Lipid Center of Excellence at Jacksonville Center for Clinical Research. She is a Registered Dietitian Nutritionist and board member of the National Lipid Association (NLA) and the Foundation of the National Lipid Association. Lori has been coordinating clinical trials with Akcea, one involving a new potential treatment for people with FCS called volanesorsen (Waylivra).
Recently, Lori was asked to testify on behalf of people with FCS. On May 10, 2018 she traveled to the Food and Drug Administration (FDA) Headquarters in Bethesda, MD to testify in front of FDA Endocrinologic and Metabolic Drugs Advisory Committee. She was accompanied by Akcea scientists who shared clinical trial data, and some people diagnosed with FCS who got to share their stories, some of whom saw great relief from volanesorsen during the clinical trials. During her testimony she encouraged the approval of volanesorsen (Waylivra), “Treatment with volanesorsen offers hope to these people, many who have been struggling for years without medical therapy”. 1
After hearing from the Akcea scientists, the people with FCS and Lori’s testimony, the advisory committee voted 12-8 in favor of recommending volanesorsen’s approval to the FDA! The FDA has set a date for the completion of its review on August 30, 2018. 2
References:
- https://www.lipid.org/nla/alexander-testifies-front-fda-advisory-committee-behalf-fcs-patients
- http://www.raredr.com/news/fda-votes-in-favor-of-fcs-drug
Photo Credit: National Lipid Association
I recently stumbled across the work of Professor John Norcross, the “undisputed” guru on all matters related to New Year’s resolutions. Who knew? I guess a guru may exist for nearly all things. Professor Norcross surveyed and followed a few hundred folks who made New Year’s resolutions and compared them to those who did not commit themselves to goals as the calendar year turned.
Here are a few fun facts from the Professor’s findings:
- About 50% of Americans make New Year’s resolutions on any given year and 38% absolutely will not make one in principle (er, they’ve resolved not to resolve);
- 25% of resolutions fail within one week;
- Older folks have greater difficulty keeping resolutions than younger people – 20-somethings beat 50-somethings for one-year resolution success rates – 39% versus 14%. Of course, success rates were self-reported so we can either conclude that the adage about old dogs and new tricks rings true or that millennials tend to grade on a curve.
We can draw solace from Professor’s Norcross’s most persuasive finding: those who made New Year’s Resolution were 10 times more likely to change unwanted behaviors than those who didn’t make them. Yes, setting goals works and the New Year, fresh with the feelings of optimism and renewal, seems like the perfect time to make them.
We have an exciting agenda of educational programs called “Learn with the Leaders” that we will highlight throughout the year. In January, we will talk to people about how they can help themselves with autoimmune disease, cholesterol problems, diabetes, and memory loss. Please make an effort to attend these sessions.
Participating in a research study has lots of unintended benefits but perhaps most importantly the benefit of having a team help you stick with a program. Let’s resolve to keep our resolutions this year, or at least double the amount of time until we break them.
– Michael J. Koren, MD FACC CPI FAPCR
Reference: Journal of Clinical Psychology, 58(4), 397-405
THE RESULTS ARE IN!
We would like to wish a big heartfelt THANK YOU to all our volunteers that participated in this international (PCSK9) high cholesterol study of 1300 volunteers completed in 18 countries.
Jacksonville FL volunteers lead the world in this study with ground breaking results! Our own CEO Dr. Michael J. Koren was the lead international investigator and lead author on the study. Results published in Jama Cardiology.