Scroll down to listen to this article.
I remember the early days of COVID-19, everything was new and scary and dangerous and no one knew what was going on. It seemed to be very dangerous for two groups of people, those of advanced age and those who were immunocompromised. Vaccines rolled out, testing became easy, and things have calmed down quite a bit. But corona isn’t all limes on the beach, as any virus, it’s still dangerous for people who are immunocompromised. What does this term mean, who are the immunocompromised, and is there anything they can do in the new reality of COVID-19?
Immunocompromised is a broad term. It indicates that a person’s immune system cannot generate an appropriate response to infection. When bacteria or viruses make it inside these people’s bodies, they cause much more damage and are very hard to control. The immune system is very, very complicated, so there are many ways a person can become immunocompromised. We can generally lump these into two categories: primary and secondary immunodeficiency.
Primary immunodeficiency means the condition is built-in to the body; it’s genetic. Primary immunodeficiencies are fairly rare, with <0.1% of the population experiencing them. The rest of the almost 3% of people who have immunodeficiencies have secondary immunodeficiencies.Infectious diseases (such as HIV), malnutrition, age, surgery, environmental stress, and immunosuppressive drugs can all cause secondary immunodeficiency. Immunodeficiency affects millions of Americans. Women are twice as likely as men to have immunodeficiency; it is most common in white Americans and those aged 50-59. Nearly 3% of the population – over 9 million Americans – are suspected to have immunodeficiency.
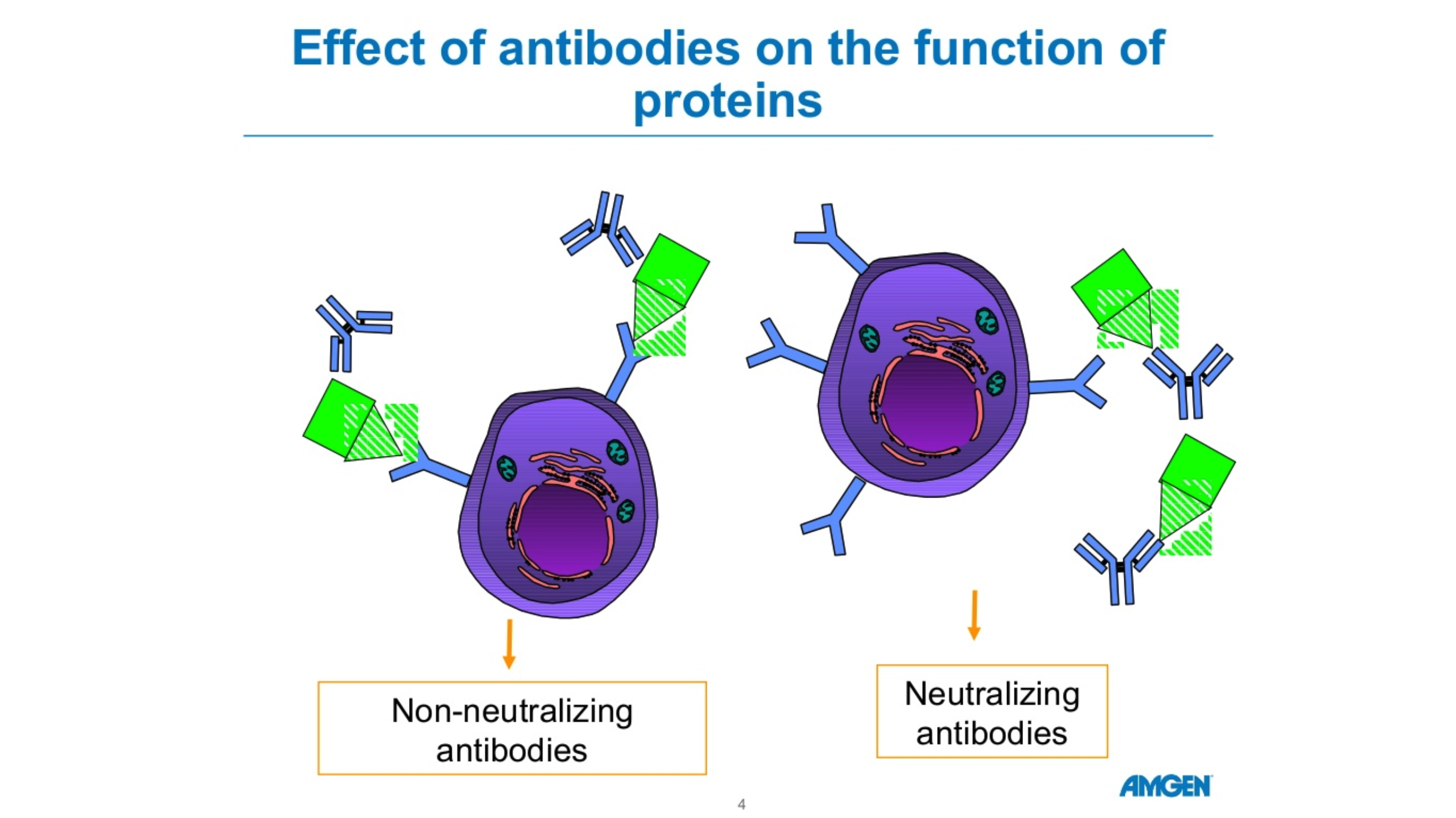
Unfortunately, immunodeficiency can greatly reduce a person’s ability to deal with a COVID-19 infection. The most obvious problem is that immunocompromised people are more susceptible to severe symptoms. A disproportionate amount of people who are hospitalized for COVID-19 are immunocompromised. Immunodeficiency doesn’t compromise, it packs a double-whammy. Those with a weak immune system also find vaccines less effective! In fact, 44% of people who had “breakthrough” cases (where they were vaccinated but still hospitalized) were immunocompromised. This is because the body is unable to produce enough protective antibodies for the body to be protected – a process called seroconversion.
Seroconversion is when antibodies are able to be detected in the blood. With vaccines, successful seroconversion indicates that the body is protected and has the equipment necessary to put up a good fight against the COVID-19 virus. When vaccinated against COVID-19, people with healthy immune systems showed seroconversion rates of 99%. The type of immunocompromisation affects how well vaccines produce seroconversion. People with solid tumor cancers, such as breast, colon, prostate, and lung cancer show seroconversion rates of 92%. Immune-inflammatory disorders like lupus, primary biliary cholangitis, psoriasis, and rheumatoid arthritis have seroconversion rates reduced to 78%. Vaccine effectiveness in people with blood cancers such as lymphomas, myeloma, and leukemia drops to 64%. Those with organ transplants have to be on strong immunosuppressive drugs to avoid organ rejection and because of this they have the lowest rates of seroconversion, only 27%.
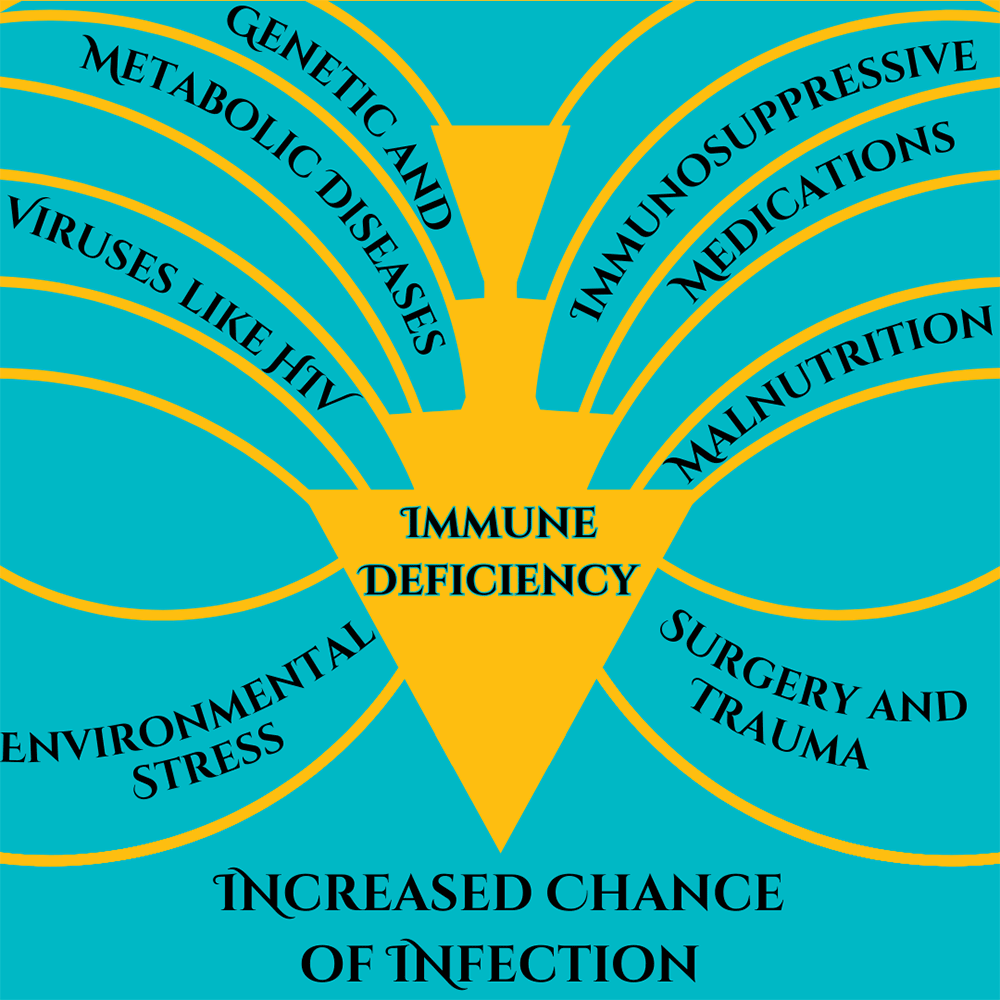
Some factors of immunocompromisation. Adapted from Chinen, J., & Shearer, W. T. (2010).
So what can immunocompromised people do to protect themselves against COVID-19? A lot of the same things as people who are immunocompetent! High quality masks and respirators can help. Avoiding crowds and indoor areas with poor ventilation is a must. Washing hands with soap and water is critical, though hand sanitizer is a good second option. Immunocompromised people who contract COVID-19 should contact their doctor or other healthcare provider right away. Isolating and using masks to prevent the spread is always a good idea. Immunocompromised people may also keep infections from getting out of control if their medical provider recommends an antiviral medication or convalescent plasma. Of course, the best way to avoid getting sick with COVID-19 is through prevention, including vaccines. A 27% seroconversion rate is much better than 0% after all. And there may be more hope for immunocompromised people, as new vaccines are being developed to serve this community.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Boyle, J. M., & Buckley, R. H. (2007). Population prevalence of diagnosed primary immunodeficiency diseases in the United States. Journal of clinical immunology, 27, 497-502. https://link.springer.com/article/10.1007/s10875-007-9103-1
Chinen, J., & Shearer, W. T. (2010). Secondary immunodeficiencies, including HIV infection. Journal of Allergy and Clinical Immunology, 125(2), S195-S203. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6151868/
Harpaz, R., Dahl, R. M., & Dooling, K. L. (2016). Prevalence of immunosuppression among US adults, 2013. Jama, 316(23), 2547-2548. https://jamanetwork.com/journals/jama/fullarticle/2572798
National Institute of Health. (July 21, 2023). Special considerations in people who are immunocompromised. COVID-19 Treatment Guides, https://www.covid19treatmentguidelines.nih.gov/special-populations/immunocompromised/
Parker, E. P., Desai, S., Marti, M., Nohynek, H., Kaslow, D. C., Kochhar, S., … & Wilder-Smith, A. (2022). Response to additional COVID-19 vaccine doses in people who are immunocompromised: a rapid review. The Lancet Global Health, 10(3), e326-e328. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(21)00593-3/fulltext
SY, L. A. W., SC, C. L. L., & Muthiah, L. M. (2021). Efficacy of COVID-19 vaccines in immunocompromised patients: A systematic review and meta-analysis. medRxiv. https://doi.org/10.1136/bmj-2021-068632