
Scroll down to listen to this article.
The eyes are the windows to the soul. But what happens when those windows don’t get properly cleaned? They might get scratchy, stingy, blurry, and discolored. Dry eye disease is when tears don’t adequately lubricate the eye. Symptoms include scratchy burning or stinging in the eyes, red eyes, sensitivity to light, and blurry vision. This disease affects 5%-30% of the world population and is more common in women and those above 50 years old. Dry eye is a multifactorial disease, meaning multiple things may have a hand in causing it. To understand what might be going wrong, we first have to understand a little about how the eye works.

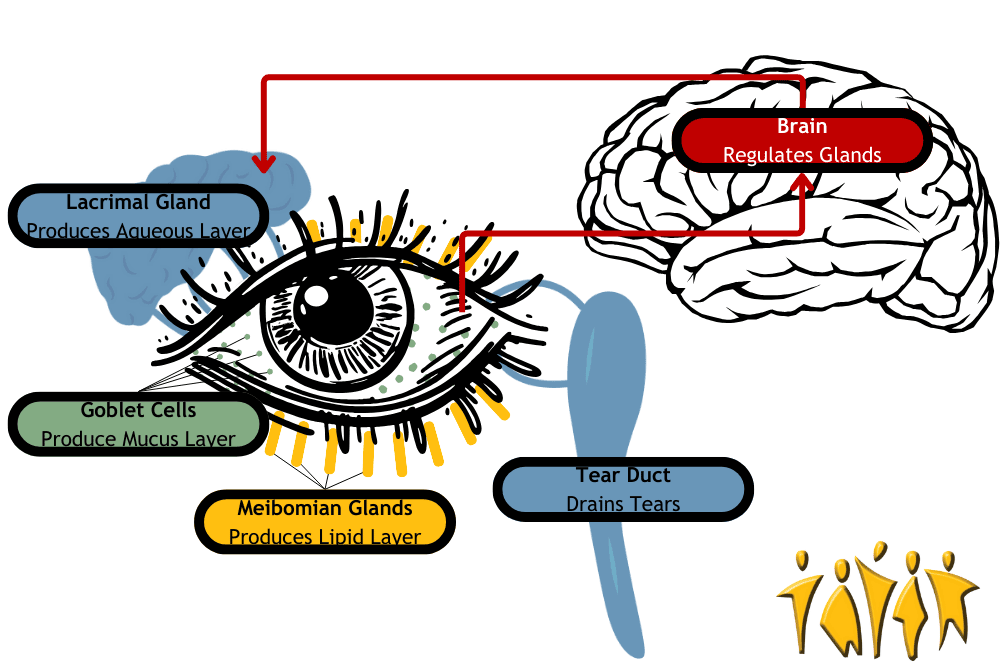
The eye is lubricated by a 3-layered film called the tear film on the outside. That’s tear like near, not tear like hair. The layers, from inner to outer, are the mucus layer, aqueous (water) layer, and lipid (oil) layer. These aren’t hard, distinct layers, but each has a separate purpose. The mucus layer is secreted by goblet cells located on the surface of the eye and lubricates it. The aqueous (water) layer is secreted by the lacrimal gland and keeps everything clean. It is susceptible to evaporation, which is where the lipid (oil) layer plays a part. The lipid layer is oily, which resists evaporation and is secreted by meibomian glands on the edge of the eyeball. Together, these layers act like a crew of window washers to keep the eye lubricated and clean.
Don’t let all the vocabulary make you googly-eyed: the lacrimal gland, goblet cells, and meibomian glands just produce different types of eye fluids. They work together to produce the tear film, but they don’t work alone. The brain receives moisture signals from the eye and sends signals to the glands to keep the eye moist. The eyelids spread the tear film and help prevent evaporation. Finally, the surface of the eye itself needs to be clean and healthy. Together, these components make up the lacrimal functional unit. Disruptions to this system are the cause of dry eye disorder. Problems can be divided into broad categories, but each can overlap and lead to problems with other parts of the lacrimal functional unit.
Problems can originate in the nerves to and from the brain. These can become inflamed or attacked by immune cells such as with Sjogren’s syndrome. When the nerves from the brain to the lacrimal gland are disturbed, tear production might be reduced. When the sensory nerves from the eye to the brain are disrupted, the brain doesn’t know to tell the lacrimal glands to secrete tears and keep the tear film intact. Nerve response can also be disrupted permanently by long-term contact lens use and temporarily by laser surgery. The cells of the eye itself can also be damaged. Epithelial (surface) cells need to interface smoothly with the tear film. The aqueous (water) layer can be deficient – you may not produce enough tears. This can be due to inflammation and autoimmune problems (as above), obstructed glands, nerve damage, and more. Medicines like antihistamines, beta-blockers, and diuretics can also reduce the aqueous layer. Allergies can cause dry eye, so the fact that antihistamines can cause it too is deeply eye-ronic. Finally, tears may evaporate too quickly. This is called tear instability or evaporative dry eye and is usually due to a problem with the oil layer. Other evaporative problems include eyelid problems, gland dysfunction, decreased blinking, vitamin A / omega-3 deficiency, and environmental problems (like wind and smoke).
To help with dry eye we can look at three methods: environmental, surgical, and medical. Environmental relief can be found by avoiding dry, dusty, and smoky air while ensuring you get enough vitamin A and Omega-3. Surgical blocking of the drainage tear duct can keep moisture on the eye surface longer. Medical solutions include different types of eye drops. Some mimic tears, and some deliver medicine. For severe and chronic problems, there are two major medications: cyclosporine and nerve growth factor (NGF). Cyclosporine is an immunosuppressive drug that can relieve inflammation in the nerves and glands. Nerve growth factor is an amazing medical category that can regenerate damaged nerve fibers and can heal surface epithelial cells. With new clinical trials on the horizon, we can peer through the window to new relief for dry eyes!
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Lemp, M. A., & Foulks, G. N. (2007). The definition and classification of dry eye disease. Ocul Surf, 5(2), 75-92.
Mantelli, F., Massaro‐Giordano, M., Macchi, I., Lambiase, A., & Bonini, S. (2013). The cellular mechanisms of dry eye: from pathogenesis to treatment. Journal of cellular physiology, 228(12), 2253-2256. https://onlinelibrary.wiley.com/doi/pdf/10.1002/jcp.24398
National Eye Institute. (April 8, 2022). Dry Eye. National Institute of Health https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/dry-eye



