Scroll down to listen to this article.
This article was requested by an ENCORE community member. We do not currently have a study enrolling for this topic.
The immune system is huge, complex, critical for life, and dangerous. It is good for us, protecting us by fighting infections and cancer; but there is a dark side: the inflammation it uses to fight can cause damage, it can overreact to cause autoimmune diseases, and its vigilance against invaders is what makes organ transplants difficult. The immune system is specialized in destroying cells and viruses. One of the most important features of the immune system is its ability to differentiate between cells we want and cells we don’t (including cancer cells!). However, when things go wrong, they can go very wrong. This may happen with autoimmune diseases like lupus or rheumatoid arthritis. Things may also go wrong when the immune system attacks transplanted organs; like a heart or liver. In these cases, we turn to immunosuppressant drugs. These do just what their name implies: they suppress the immune system. How they actually go about suppressing is very complicated, and requires a quick look at the immune system in general.
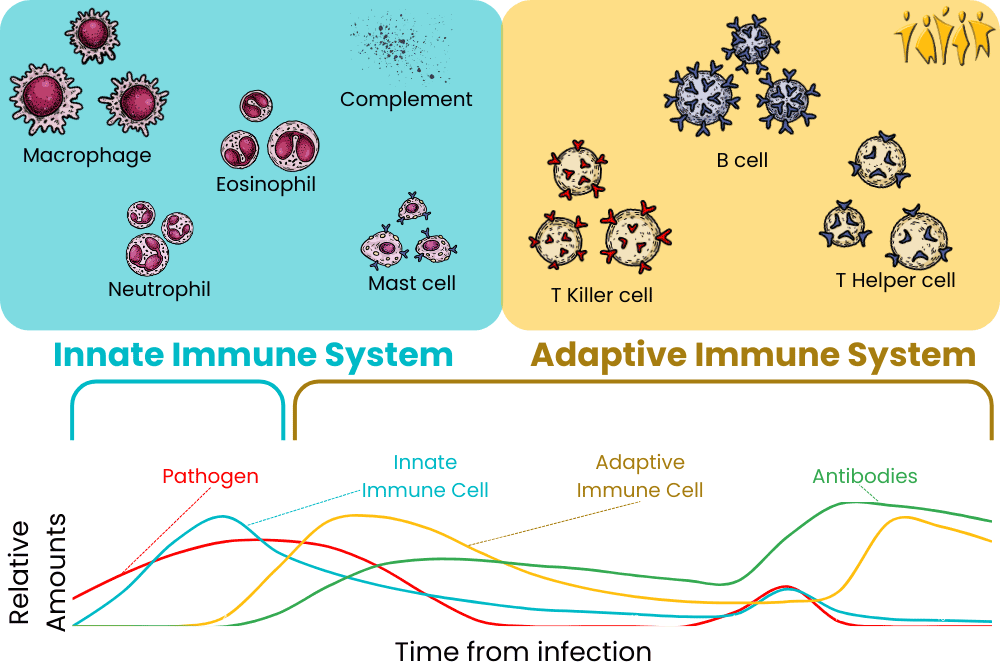
A very, VERY simplified version of the immune system and how it responds over time
The immune system can be divided into two major pieces, the innate and adaptive immune systems. There is overlap, as some cells have multiple functions. The innate immune system is made of cells that attack any invader they sense. These get activated immediately when we have infections or wounds and are like big, blunt weapons in their killing. The innate immune system includes monocytes, mast cells, macrophages, neutrophils, and eosinophils. These white blood cells ingest and eat perceived threats and cause inflammation. Inflammation helps bring in the complement system, a horde of mindless proteins that aim to attack invaders. If infections are not stopped immediately, dendritic cells activate the adaptive immune system. This is made up of T cells, B cells (including plasma cells), and antibodies. Throughout all this, cytokines like interferon and interleukin modify the immune system and are used for communication. Immunosuppressant drugs tend to target either the immune system at large or specific aspects of it, like T cells.
-mab Monoclonal antibody
-cept Targets receptor molecules
-mib Inhibits protein breakdown mechanisms
A quick guide to what the endings of some drugs mean
T cells are special cells that detect, remember, and fight against invaders. When they misidentify healthy cells as invaders, things get out of control quickly. Certain medications, like cyclosporin, tacrolimus, and voclosporin target the T cell’s ability to detect “dangerous” particles – like a transplanted organ. Others, such as Abatacept and Belatacept downregulate the ability of T cells to respond effectively. These tend to cause high blood pressure and associated problems.
B cells are critical for producing deadly antibodies. They also act as memory cells to ensure future infections are dealt with quickly. The two ways to deal with wayward B cells are by destroying them or limiting their ability to differentiate. Rituximab, ocrelizumab, ofatumumab, and veltuzumab target B cells for destruction, while bortezomib targets specialized plasma cells that spew antibodies at a rate of 2000 per second. By lowering the number of B cells they cause less autoimmune damage. Targeting B cell differentiation limits their functionality with medications like belimumab and atacicept, but comes at the expense of reducing some cell signals and possible pneumonia.
Free-floating proteins are critically important to the immune system. The complement system is composed of quintillions (!!!) of tiny proteins that act autonomously to hamper invaders. Eculizumab targets a specific protein that helps activate the destructive powers of the complement system. Cytokines are different but equally important proteins. They are the communication particles used by the immune system. Corticosteroids are broad immunosuppressant anti-inflammatory drugs. They reduce the activity of the immune system, slow fluid flow that causes inflammation, interfere with cytokines, and inhibit immune cell production. They can be effective, but the effects are not specific to the immune system and can cause problems with “virtually every system in the body” (Barshes, 2004). Major side effects include bone problems like osteoporosis, skin changes, obesity, diabetes, and neurologic changes. Advanced medications like basiliximab, anikara, and rilonacept target only specific cytokines, with hopefully reduced side effects that may be flu-like.
Finally, two medication classes reduce B and T cell counts through unique mechanisms. Polyclonal antibody immune globulins are additional antibodies that are given at high doses. These seem to overwhelm the immune system, depleting white blood cell counts and keeping it from attacking itself. These are potent but come with severe side effects that feel like getting sick: hives, fever, headaches, and even heart attacks. Alemtuzumab is a medication that targets proteins found outside B and T cells and targets them for death. This has the expected side effects of fever, nausea, etc.
Each class of medication targets a different part of the immune system. This means some may be more useful in some situations, and some may not work at all in some instances. Please note that all medications should be discussed with a medical professional who is aware of your unique medical history; don’t make medical choices based on an internet article! Further, we’ve mentioned some of the bigger, or more general side effects of these medications, but each has many more that should be considered before use. We’ve also left off the most important side effect of all: these suppress the immune system! Patients on these medications are more prone to infection, cancers, and dangerous particles in the body. They are dangerous and should not be taken lightly. Instead, prudence demands that taking an immunosuppressant medication be weighed against the alternative. In the case of a critical organ transplant, like a heart, it’s a no-brainer. Each situation is unique and should be discussed with your medical team.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Barshes, N. R., Goodpastor, S. E., & Goss, J. A. (2004). Pharmacologic immunosuppression. Front Biosci, 9(1-3), 411-420. https://doi.org/10.2741/1249
Claeys, E., & Vermeire, K. (2019). Immunosuppressive drugs in organ transplantation to prevent allograft rejection: Mode of action and side effects. Journal of immunological sciences, 3(4). https://immunologyresearchjournal.com/articles/immunosuppressive-drugs-in-organ-transplantation-to-prevent-allograft-rejection-mode-of-action-and-side-effects.pdf
Dettmer, P. (2021). Immune: A journey into the mysterious system that keeps you alive. Random House.
Nicholson, L. B. (2016). The immune system. Essays in biochemistry, 60(3), 275-301. https://portlandpress.com/essaysbiochem/article/60/3/275/78223/The-immune-system
Wiseman, A. C. (2016). Immunosuppressive medications. Clinical journal of the American Society of Nephrology: CJASN, 11(2), 332. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4741049/