When we think of an animal, we generally think of a single creature with a unique DNA code. A human starts as a single fertilized egg cell with the combined genetic code from our parents. By the time we’re walking and talking, however, we’ve already transformed into a superorganism. If you were to count the number of cells that make you up, only half would be human. Mature red blood cells lack a nucleus, so if we count only cells with nuclei, we’re only about 10% human. Going further, if we count all the genetic material in our body, only about 1% of it is human. Genetically, we’re 99% nonhuman. So then, what are we?
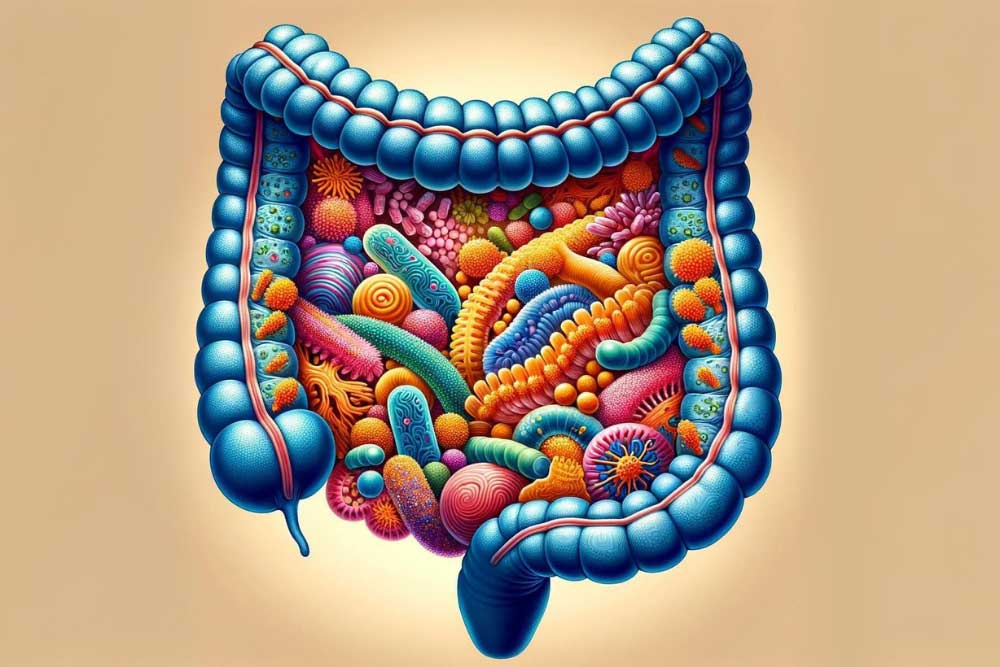
Bacteria. We’re primarily bacteria. These bacteria live with us our whole lives. They live on our skin, in our hair, on our eyelashes, and in our gut. The bacteria that live in the digestive tract, along with the relatively minuscule amounts of viruses, archaea, and yeasts, make up the gut microbiome. The gut microbiome is incredible. It establishes itself until around age two. It changes in response to the food we eat, diseases we get, medications we take (especially antibiotics), and our hygiene. We eat around 60 tons of food in our lives, and the gut microbiome has a hand in all of it. We usually think of bacteria (and viruses, etc) as parasitic (doing damage). The reality is the gut microbiome is truly symbiotic, we need it as much as it needs us.
The gut microbiome performs many tasks for us. It shapes the human cells and the mucus that lines our gut, strengthening it. It protects us from infections, keeps our cells together in a tight barrier, and communicates with the immune system. Microbiome cells outcompete other, destructive bacteria. They can also release bacteriocins (bacteria-targeting toxins) that destroy dangerous bacteria. The microbiome is so stellar it helps us even when it’s just eating.
The gut microbiome breaks down foods we can’t process, like dietary fiber. Through the process of fermentation, it uses this food to make vitamins, minerals, etc. As an example: we can’t make vitamin B12 at all in our cells; we rely on microorganisms to make it for us! Finally, the gut microbiome makes short-chain fatty acids. Short-chain fatty acids are the primary energy source for the human cells that line the intestine. They also increase insulin sensitivity and mediate immune regulation, inflammation, and other body processes.
Unfortunately, the gut microbiome can get out of whack, and issues like ulcerative colitis – an inflammatory bowel disease – can occur. To understand what can go wrong, let’s first investigate a healthy gut microbiome. The colony of colon bacteria is unique in everyone. A healthy microbiome has three qualities: high diversity, high richness, and high stability. Diversity is just what it sounds like: the total number of different species present. Richness is the balance between species; having roughly equivalent numbers of bacteria from each. Stability is the consistency of finding the same types and numbers of organisms over time. So what does a disruption in the balance of the gut microbiome look like? Loss of diversity, overgrowth of some types of organisms, and changes to the composition of the gut microbiome over time. The degradation of diversity, richness, or stability is called dysbiosis.
One cause of dysbiosis is antibiotics. They are designed to kill bacteria, which is bad news for the gut bacteria. Antibiotics frequently lead to a redistribution of gut microbiota. Other things that can cause dysbiosis include hygiene, infection, and smoking. The most important, however, is diet. All of the food we eat travels through the gut. In the western world, our diets aren’t always built to cultivate a healthy gut microbiome. Much of our food is built for shelf stability and is made using enzymes or chemicals instead of bacteria. We tend to eat more animal fats and proteins and fewer plant fibers than indigenous populations. To top this off, we eat refined sugar. Like, a LOT of refined sugar. Around 50 to 100 pounds of refined sugar per year. I’m not a nutrition expert, but I am a cookie expert, and that’s way too many cookies.
When the microbiome is in a state of dysbiosis, it can’t perform its helpful functions. The mucus layer is reduced, bacteria can’t interact with the immune and inflammation systems, and the gut is more permeable to undesirable substances. On top of this, short-chain fatty acid production decreases, making it more difficult for the human cells lining the gut. This loss of function is linked to diseases like ulcerative colitis. The exact causes of ulcerative colitis are unknown, but scientists think it is related to the gut microbiome. Ulcerative colitis is a chronic inflammatory disease with periods of high and low activity. Inflammation leads to painful ulcers along the colon and rectum.
So what can we do when the gut is out of whack? This is still a relatively new area of research, so there are many questions we have to answer. Our best solutions so far are food and feces. The importance of food to the gut microbiome should be obvious by now. Foods high in dietary fibers from plants are needed for gut bacteria to survive and thrive. The role of bacteria derived from human feces is still being developed. Fecal transplantation is a fascinating, but not-for-the-dinner-table line of study. The basic idea is that doctors would transfer some of the gut microbiome from a healthy person to a sick one, perhaps someone with ulcerative colitis. These bacteria would hopefully colonize and outcompete whatever is disrupting the sick microbiome, restoring diversity, richness, and stability. Focusing on the symbiotic relationship we share with our individual microbiome will revolutionize our approach to healthcare. Clinical trials may pave the way forward for treatments that support our human cells and our microbiome, nurturing the microbial communities vital to our survival and well-being as a superorganism. Also, don’t forget to eat your veggies.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Bengmark, S. (1998). Ecological control of the gastrointestinal tract. The role of probiotic flora. Gut, 42(1), 2-7. https://doi.org/10.1136/gut.42.1.2
Fan, Y., & Pedersen, O. (2021). Gut microbiota in human metabolic health and disease. Nature Reviews Microbiology, 19(1), 55-71. https://doi.org/10.1038/s41579-020-0433-9
Gomaa, E. Z. (2020). Human gut microbiota/microbiome in health and diseases: a review. Antonie Van Leeuwenhoek, 113(12), 2019-2040. https://link.springer.com/article/10.1007/s10482-020-01474-7
LeBlanc, J. F., Segal, J. P., de Campos Braz, L. M., & Hart, A. L. (2021). The microbiome as a therapy in pouchitis and ulcerative colitis. Nutrients, 13(6), 1780. https://doi.org/10.3390/nu13061780
Sender, R., Fuchs, S., & Milo, R. (2016). Revised estimates for the number of human and bacteria cells in the body. PLoS biology, 14(8), e1002533. https://doi.org/10.1371/journal.pbio.1002533
Świrkosz, G., Szczygieł, A., Logoń, K., Wrześniewska, M., & Gomułka, K. (2023). The Role of the Microbiome in the Pathogenesis and Treatment of Ulcerative Colitis—A Literature Review. Biomedicines, 11(12), 3144. https://doi.org/10.3390/biomedicines11123144
Tan, J., McKenzie, C., Potamitis, M., Thorburn, A. N., Mackay, C. R., & Macia, L. (2014). The role of short-chain fatty acids in health and disease. Advances in immunology, 121, 91-119. https://doi.org/10.1016/b978-0-12-800100-4.00003-9
The Human Microbiome Project Consortium. (2021). Structure, function and diversity of the healthy human microbiome. Nature 486, 207–214. https://www.nature.com/articles/nature11234
Thursby, E., & Juge, N. (2017). Introduction to the human gut microbiota. Biochemical journal, 474(11), 1823-1836. https://portlandpress.com/biochemj/article/474/11/1823/49429
Xiong, R. G., Zhou, D. D., Wu, S. X., Huang, S. Y., Saimaiti, A., Yang, Z. J., … & Li, H. B. (2022). Health benefits and side effects of short-chain fatty acids. Foods, 11(18), 2863. https://doi.org/10.3390%2Ffoods11182863
Young, V. B., & Schmidt, T. M. (2008). Overview of the gastrointestinal microbiota. Advances in experimental medicine and biology, 635, 29–40. https://doi.org/10.1007/978-0-387-09550-9_3