Scroll down to listen to this article.
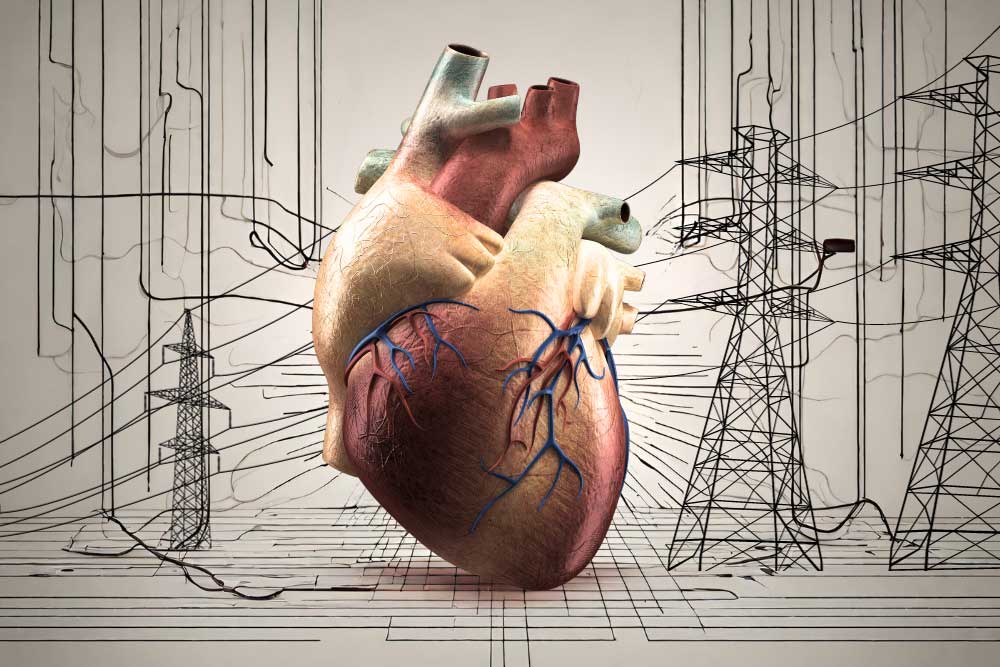
Electricity is essential for most modern-day activities. We use it for lights, air conditioning, and watching cat videos. We also use it to keep our hearts beating. Electricity coordinates the heart and causes it to contract into its familiar wub-dub. Why do we need electricity in the heart, and what can we do when the zips don’t zap properly?
Shockingly, we’ll start with a broad overview. The heart is an organ made of several billion cells. These are organized into many structures, including chambers. There are two small upper chambers called atria, which is the plural word for the left atrium and right atrium. There are also two large lower chambers called ventricles, which are again separated into left and right. The set on the left pumps fresh, oxygenated blood from the lungs to all the cells in the body. The set on the right pumps deoxygenated blood to the lungs to get more oxygen. It is a little strange to describe the heart only as a series of chambers, as the actual structure of the heart is a giant, very strong, coiled muscle. In order for muscles to contract and produce power, electricity is needed. Electricity tells the muscles they need to move. In most of the body, the electrical signals for muscles to contract are delivered by the brain. The heart is a little different.
The heart is involuntary, meaning we have no direct control over when it beats. We can send signals to the heart by breathing deeply or jumping, but the electrical signal that tells the heart to beat comes from within the heart itself. Near the top is a collection of cells called the sinoatrial (SA) node. Here resides a group of cells called pacemaker cells. These cells produce a small electrical zippy zappy signal around once per second. This signal rapidly amplifies and spreads throughout the atria, causing them to contract. This spreading comes out like a wave, which allows all the atrial muscle cells to contract in a big, coordinated manner. Soon after, the signal travels through the atrioventricular (AV) node into the ventricles, propagating outward. This takes a fraction of a second, so we hear wub-dub instead of just one big beat. This also gives blood time to travel from the atria to the ventricles, ensuring it goes correctly.
This system is pretty amazing, but it’s not foolproof. Many things can go wrong. The electrical signal might be disrupted, the heart might be too slow, or it might beat at a bizarre rhythm. When this happens, the heart pumps less efficiently than it needs to, and sometimes can’t pump enough blood for oxygen to get around the body. Unlike a heart attack, where heart cells die immediately, electrical problems can often be alleviated. When the electricity in our heart doesn’t behave correctly, we can put in artificial electricity.
When the heart’s pacemaker cells aren’t successfully sending coordinated signals to the whole heart, an artificial cardiac pacemaker (often just called a pacemaker) can be implanted. Temporary pacemakers may sit outside the body, but permanent ones are installed inside our body cavities. These are made of materials our bodies don’t find threatening, like titanium. They can be attached to the heart through wires called leads, mounted on the heart surface, or inside the heart muscle. Each patient will have electrical problems in specific areas; maybe the pacemaker cells aren’t working properly, or maybe electricity can’t travel to the ventricles, or maybe it can’t cross from the left to the right side. Because of this, pacemakers can attach to either an atrium, a ventricle, or to both ventricles.
Because the electrical problems are so varied, artificial pacemakers have many different patterns for firing. Artificial pacemakers don’t just cause beating; they also detect it. Little electrodes can tell when the heart has fired, and internal circuitry can measure this against when the cardiologist thinks a beat should have happened. Most will detect when a shock is needed and fire on demand, but some fire all the time. Pacemakers can respond to changes in heart rate, can sense abnormal rhythms, and have special modes for things like surgery. On top of all of this, medical professionals can often remotely monitor artificial pacemakers and adjust the pacemaker’s programming without surgery! This can be used to make sure heart rhythms stay ideal, but can also help alleviate the side effects of artificial pacemakers, which include chest pain, dizziness, fatigue, and shortness of breath. Pacemakers are amazing wonders of the modern era. As time goes on, scientists are developing new and more specific programs to zap the heart without zapping our fun. It’s nice to know that when you watch a video of a funny cat falling off the dresser, electricity makes your heart happy inside and out.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
Buckberg, G. D., Nanda, N. C., Nguyen, C., & Kocica, M. J. (2018). What is the heart? Anatomy, function, pathophysiology, and misconceptions. Journal of cardiovascular development and disease, 5(2), 33. https://www.mdpi.com/2308-3425/5/2/33
Lak, H. M., & Goyal, A. (2020). Pacemaker types and selection. https://www.ncbi.nlm.nih.gov/books/NBK556011/
Sundnes, J., Lines, G. T., Cai, X., Nielsen, B. F., Mardal, K. A., & Tveito, A. (2007). Computing the electrical activity in the heart (Vol. 1). Springer Science & Business Media.