Nonalcoholic Steatohepatitis, or NASH, has no approved medications available for treatment. This isn’t because the disease is safe, however. NASH can lead to cell death, cells going rogue, collagen accumulation, fibrosis, cirrhosis, and liver cancer. One problem with treating NASH is that it is a multifactorial disease, meaning there are many possible causes that all lead to the same outcome. The current best methods for treating NASH are exercise, weight loss, and treating other conditions that may contribute. We will discuss scientifically backed information regarding these treatment options, but it is critical that any medical advice be discussed with your doctor. NASH has many many causes and affects a lot of body systems. Medical professionals that may be involved in NASH treatment include your primary care physician, a hepatologist, dietitian, endocrinologist, cardiologist, and others. Every person is an experiment of one, and your specific circumstances may contraindicate one or all of the methods discussed below. Talk to your doctor.
Weight loss is the go-to method of treating NASH. A combination of diet and exercise is the best method to achieve weight loss. This ensures fewer calories enter the body than exit it, and that the body is burning weight from fat instead of from muscle. Losing weight very rapidly can be dangerous, so be conscientious of your body’s overall health (and speak with a professional!) Research has shown that reducing weight by as little as 5% (12.5 lbs for a 250 lb person) can help improve steatosis, the fat buildup in the liver. Losing 7% or more (17.5 lbs for a 250 lb person) also shows a reduction in inflammation and improved health of liver cells. When patients, particularly obese patients, lose 10% of their body weight (25 lbs for a 250 lb person) the structural liver changes known as fibrosis start to regress or stabilize. For NASH patients of a normal weight, they may see results when losing as little as 3-5% of body weight.
Exercise is a great way to lose weight, but studies have shown that exercise can help your liver even when you aren’t losing weight. The exact mechanisms for how this works are complex and not fully known. Scientists have found that exercise helps make the body more sensitive to insulin – which helps it regulate blood sugar better. It can also help cellular metabolism. Exercise is associated with a reduction in the markers of liver inflammation and may help liver cells stay healthy. Aerobic exercise, also called “cardio,” is highly recommended. Resistance training, called strength training, is also helpful, especially if aerobics are not possible. NASH patients start seeing benefits when doing exercise for 150-300 minutes (2 ½ – 5 hours) per week of moderate intensity exercise or 75-150 minutes (1 ¼ – 2 ½ hours) per week of high intensity exercise. Always ease into a new exercise routine to avoid injury. Talking to a medical professional is also a good idea before starting new exercises (there is a theme to this article).
Exercise burns calories, but to lose weight we also want to manage what calories we take in. Consult with your doctor or dietitian, but reducing caloric intake to around 500 fewer than the daily recommended value may help. Further, the number of calories is not directly correlated to the quality of the calories. NASH patients find improvements when reducing items that can damage the liver, including fructose and saturated fats. Fructose is a form of sugar that is often added to sugary beverages (usually in the form of high fructose corn syrup) and contributes to insulin resistance. Saturated fats are found in meats, including red meats and processed meats. As for specific diets, research is ongoing. The Mediterranean diet has the most research backing its success in NASH patients. It is rich in fruits, vegetables, whole grains, seafood, nuts, legumes, and olive oil. Other diets may be suitable as well, including intermittent fasting, ketogenic diet, and others. One recommendation is to take the Mediterranean diet and adjust it to fit you. Regardless of the diet choice, alcohol should be limited. For smokers and former smokers, alcohol should be eliminated entirely. It should go without saying that making major adjustments to your diet should be consulted with your doctor.
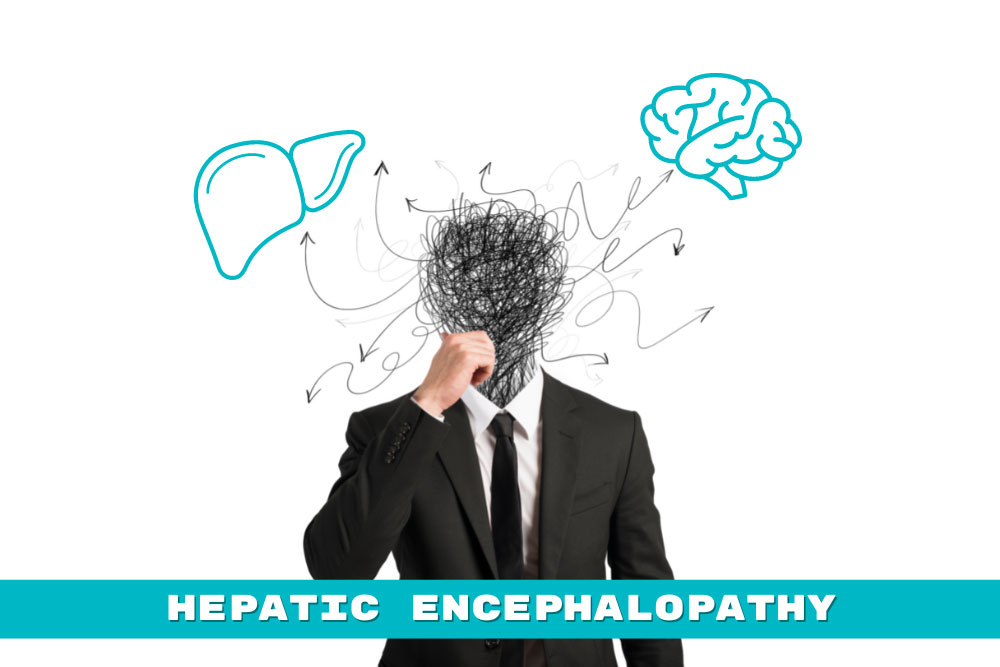
Other than diet and exercise, treatments for NASH are all achieved by treating other conditions that contribute, and will vary depending on the individual. Conditions that contribute are obesity, diabetes, high blood pressure, high cholesterol, cardiovascular disease, and obstructive sleep apnea. Cardiovascular disease and obstructive sleep apnea are major contributors of mortality for NASH patients and should be taken seriously. Obviously these conditions are best treated by going to your doctor.
NASH is a progressive disease that gets worse over time and leads to serious, occasionally deadly complications. Clinical trials may give us a medical NASH treatment in the future. Until then, give yourself a leg up (or liver) by consulting your doctor about treatments through diet, exercise, and underlying condition management.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA