Last week we talked about the actions of the Nazis, which resulted in the World Medical Association’s Declaration of Helsinki. The declaration provides an ethical guideline for physicians engaging in research involving humans. It has since become a requirement in most medical research. Unfortunately, in America, a study that began seven years prior to World War II undermined this ideal. It wouldn’t be until the 1970s that this study was exposed, and America was faced with its own dark practice of human research.
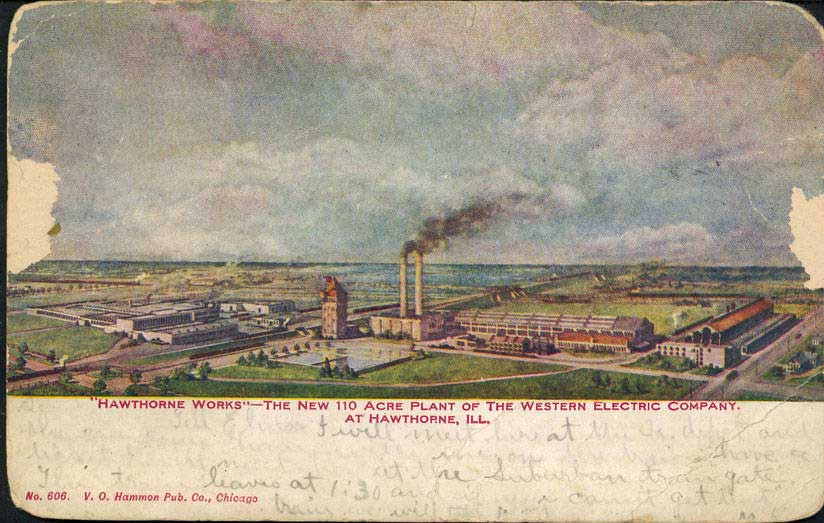
In 1932, doctors at the Tuskegee Institute (Now called Tuskegee University) started a fundamentally unethical experiment. The road to this study winds from good intentions to simple, terrible means. The historical context behind the study involves the Julius Rosenwald Fund, a wholly honorable philanthropic endeavor. This fund built schools in the South, funded Booker T. Washington to attend the Tuskegee Institute, and worked with the U.S. Public Health Service to provide medical services to the poorest Black Americans in the South. One of these medical service endeavors was providing syphilis treatment. Part of this effort involved cataloging the rate of syphilis in several areas. The great depression and Julius Rosenwald’s death brought much of this to a halt, and the syphilis project ended in 1932.
Other scientists wanted to pick up where the Julius Rosenwald Fund left off. These scientists believed that different races experienced diseases differently. The new study would observe the ravages of untreated syphilis in Black populations. They already had the groundwork built. They had a large number of men with untreated syphilis, a nearby hospital at Tuskegee Institute, a bank of goodwill built by Rosenwald, and a store of trust in medical professionals and the U.S. Public Health Service. The scientists successfully exploited all of these. They intentionally coerced and deceived 400 Black Americans into their study. The study had no protocol, patients had no informed consent, and one of the major endpoints was to wait until patients died and then deceive their loved ones into allowing an autopsy. This alone is terrible, but it was – unfortunately – much worse. After the end of World War II, an effective treatment for syphilis became widely available: penicillin. The researchers didn’t provide this to their patients and, in fact, actively thwarted its use in this population. They convinced hospitals, government agencies, and even the U.S. military that the torturous observation of sick and dying people was more important than their health and well-being. This continued for 40 years and only ended in 1972 after the experiment started getting public attention and press.
The Tuskegee study ended almost a decade after the Declaration of Helsinki and prompted the passage of the National Research Act and the creation of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. A group of 11 people spent four years developing the Belmont Report. Whereas the Declaration of Helsinki outlines ethical standards to follow, the Belmont Report gives specific guidelines and actionable procedures for determining the legitimacy of research involving human participants. It was initially incorporated into federal law in 1981 as the Protection of Human Subjects.
The Belmont Report first outlines the difference between medical practice and research. The goal of practice is normal therapy with a reasonable chance of success, while the goal of research is to test a hypothesis and answer a question. Whereas practice follows the needs of the patient, research follows well-defined, written protocols. The Belmont Report maintains the same three ethical principles in the Declaration of Helsinki – Respect for Persons, Beneficence, and Justice. It then outlines the practical, actionable processes: Informed Consent, Risk/Benefit Assessment, and Subject Selection.
Respect for Persons is the idea that most people can make their own choices, and those that can’t must be afforded special protection. These protections must be assessed by third parties, protect participants from harm, and be periodically reevaluated. The Belmont Report applies respect for persons as Informed Consent. Informed consent requires that before a study begins, all information, including the procedure, risks, etc. be clearly written and organized. It requires comprehension by all potential human participants of the above information. Patients cannot be enrolled if they do not understand the informed consent, and the information can’t be written in tiny print and put off to the side like a used car ad. This also means that vulnerable populations (those with limited comprehension, like children) must have extra protection, and third parties (like parents) must help determine comprehension. Finally, informed consent is only given if it is voluntary. This means no large sums of money, threats, or exaggerated promises can be used to coerce people into studies. This can make it more difficult to enroll patients but is critical to avoiding disasters like the Tuskegee syphilis study.
Beneficence is the obligation to secure the well-being of patients and to do no harm. Researchers may not injure some people to help others. This is applied as Risk/Benefit Analysis. Under this concept, all benefits must be weighed against potential risks. Risks are a possibility of harm, and include the chance harm will occur and the severity of the harm. This may include things like pain from the site of an injection and must be clearly laid out in the informed consent. Risk/Benefit Analysis is done by researchers, but is overseen and double-checked by Institutional Review Boards (IRBs) – third party boards that oversee studies involving human participants. The Belmont Report lays out specific ways these IRBs assess the risks of a study. These are then weighed against benefits. Benefits are a positive change in health or welfare and are usually much clearer – the alleviation of symptoms from being in a medical study, for instance.
Justice is an equal distribution of burdens and benefits across society. Further, justice demands that the groups that participate in research should be the ones that receive the benefits. The racially biased attitudes that formed the basis of the Tuskegee study are the prime example of a failure of justice. These groups were denied benefits, and researchers demanded they take the burdens. The Belmont Report applies justice by way of Selection of Subjects. On the individual level this means that all subjects get fair treatment: you can’t give UF fans all of the investigational medication and FSU fans all placebo, for instance. Societally, the selection of subjects should be done in ways that minimize risks, like choosing adults before children. Selection should be done as fairly as possible and should target the populations that will benefit from research.
Unfortunately, the Tuskegee study has undermined trust in government and research in some communities for the past 80 years. From this historical tragedy have arisen solid, unambiguous rules for conducting human research. These ensure safety, oversight, and mitigation of risk so participating in clinical research is beneficial for the community. With the Belmont Report, communities can get access to new medications, find relief from symptoms, and help define their legacy to find possible cures for future generations.
Staff Writer / Editor Benton Lowey-Ball, BS, BFA
Listen to the article here:
References:
National Commission for the Protection of Human Subject of Biomedical and Behavior Research. (1977). U.S. Department of Health and Human Services. https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/read-the-belmont-report/index.html
Baker, S. M., Brawley, O. W., & Marks, L. S. (2005). Effects of untreated syphilis in the negro male, 1932 to 1972: a closure comes to the Tuskegee study, 2004. Urology, 65(6), 1259-1262. https://doi.org/10.1016/j.urology.2004.10.023
Brandt, A. M. (1978). Racism and research: the case of the Tuskegee Syphilis Study. Hastings center report, 21-29. https://doi.org/10.2307/3561468
Gray, F. D. (1998). The Tuskegee syphilis study: The real story and beyond. NewSouth Books.